FIG. 40.1 Digestive system and its associated structures. (From Sole ML, Klein DG, Moseley MJ: Introduction to critical care nursing, ed 7, Philadelphia, PA, 2017, Elsevier.)
Herniorrhaphy, Diaphragmatic Replacement of abdominal contents that have entered the thorax through a defect in the diaphragm and repair of the diaphragmatic defect.
Herniorrhaphy, Epigastric and Hypogastric Repair and closure of the abdominal wall defect.
Herniorrhaphy, Femoral A defect in the region of the femoral ring, which is located just below the Poupart (inguinal) ligament and medial to the femoral vein. Femoral hernias are seldom found in children and occur most often in women.
Herniorrhaphy, Incisional Repair of a defect in the abdominal wall that was a prior site of placement of a surgical incision. These types of repairs commonly involve placement of prosthetic (synthetic) mesh (e.g., Prolene, Gore-Tex, Parietex).
Herniorrhaphy, Inguinal Repair of a defect in the inguinal region; may be direct (through Hesselbach triangle) or an indirect (through the internal ring) inguinal hernia. These repairs also commonly use some type of prosthetic mesh, most commonly Prolene or Parietex.
Herniorrhaphy, Umbilical Reconstruction of the abdominal wall beneath the umbilicus (umbilical ring); can occur in pediatric patients and is most common in African American infants. In children, this hernia often closes spontaneously in infants before 2 years of age; therefore, these repairs should generally not be performed until after the age of 2 years. Umbilical hernias in adults will never resolve spontaneously.
Ileostomy Terminal ileum brought through the abdominal wall to empty into a drainage device (bag). Commonly used to treat inflammatory conditions of the bowel such as ulcerative colitis and regional enteritis (Crohn’s disease) and to provide a permanent or temporary stoma after surgery for obstruction or cancer.
Intussusception Telescoping of the bowel into itself.
Laparoscopy (Peritoneoscopy) Direct visualization of the peritoneal cavity by means of a lighted instrument (often connected to a color video monitor) inserted through the abdominal wall via a trocar placed through a small incision. An increasing number of abdominal procedures are performed assisted via laparoscopic techniques. Gastrointestinal or abdominal procedures commonly performed via laparoscopy include cholecystectomy, gastrojejunostomy, lysis of adhesions, splenectomy, Nissen fundoplication, inguinal herniorrhaphy, appendectomy, jejunostomy, colostomy, colectomy, ileocolectomy, and pancreatectomy.
Laparotomy (Celiotomy) An opening made through the abdominal wall into the peritoneal cavity to perform an operation in the abdomen in an open fashion (e.g., not laparoscopic).
Pancreaticoduodenectomy (Whipple Procedure) Removal of the head of the pancreas, the entire duodenum, the gallbladder, a portion of the jejunum, the distal third of the stomach, and the lower half of the common bile duct with reestablishment of continuity of the biliary, pancreatic, and gastrointestinal systems. The procedure, which is used primarily for the treatment of malignant disease of the pancreas, duodenum, and ampulla, is associated with a less than 3% risk of perioperative mortality if performed in a high volume center. Sometimes, a pylorus-sparing procedure is performed, which leaves the entire stomach intact.
Percutaneous Endoscopic Gastrostomy (PEG) Endoscopic procedure for the insertion of a tube into the stomach, either for the purpose of decompression or feeding, performed with local anesthesia and intravenous sedation.
Pyloromyotomy (Fredet-Ramstedt Operation) Enlargement of the lumen of the pylorus with longitudinal splitting of the hypertrophied circular muscle without severing of the mucosa; used as treatment for pyloric stenosis in infants. Pyloric stenosis is most common in firstborn male infants.
Pyloroplasty A longitudinal incision made in the pylorus (full thickness) and closed transversely to permit the muscle to relax and establish an enlarged outlet. Heineke-Mikulicz is the most common type of procedure.
Splenectomy Removal of the spleen; can be performed in an open or minimally invasive approach.
Transduodenal Sphincteroplasty Partial division of the sphincter of Oddi and exploration of the common bile duct for treatment of recurrent attacks of acute pancreatitis caused by formation of calculi in the pancreatic duct or blockage of the sphincter of Oddi. Can also be used in treatment of biliary stones that cannot be removed by endoscopic or percutaneous means.
Volvulus Intestinal obstruction as a result of twisting of the bowel, most commonly sigmoid colon or cecum.
General Care after Abdominal Surgery
Abdominal or gastrointestinal surgery can be performed with regional or general anesthesia. The choice of anesthesia varies with the type of procedure, the patient’s cardiac and pulmonary status, and the surgeon’s need for muscle relaxation. Usually, only short simple procedures are performed with regional (spinal or epidural) anesthesia. Diagnostic procedures such as endoscopy, biopsy, and percutaneous gastrostomy often are performed with sedation only. Inguinal or femoral herniorrhaphies are often performed with regional (spinal) or general anesthesia and occasionally with only local anesthesia. Most other abdominal surgical and laparoscopic procedures are performed with general anesthesia. All laparoscopic procedures require general anesthesia because of the need for relaxation of the abdominal wall and the need to control the patient’s respirations.
A number of abdominopelvic incisions have been developed and are commonly used (Fig. 40.2). An ideal incision ensures ease of entrance, maximal exposure of the operative site, and minimal trauma. It should also provide good primary wound healing with maximal wound strength.
The reader should review Chapters 26 through 31 for general care after surgery. See Chapter 45 for a discussion on bariatric surgical procedures and care.
Perianesthesia Care
As with any procedure, the surgeon and anesthesia care provider should give the perianesthesia nurse a full report on the anesthesia used and the procedure performed. With every procedure, the surgeon will write an operative note, which describes the procedure performed, viscera removed, drains present, and any other relevant intraoperative findings or complications. This action assists those who are caring for the patient in an assessment of the wounds, dressings, and expected drainage.
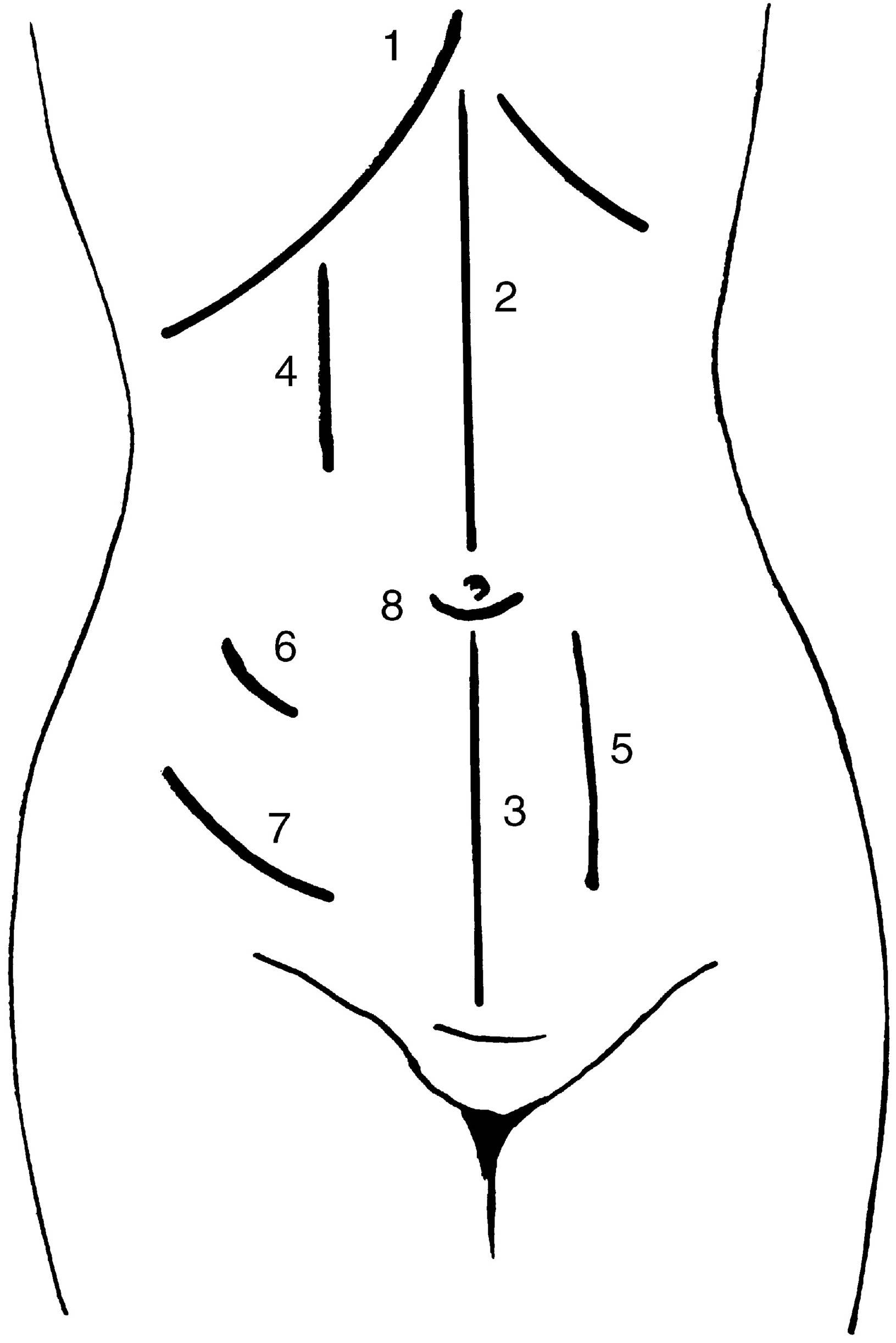
FIG. 40.2 Commonly used abdominal incisions. 1. Kocher incision: right side, gallbladder and biliary tract surgery; left side, splenectomy. 2. Upper abdominal midline incision: rapid entry to control bleeding ulcer. 3. Lower abdominal midline incision: female reproductive system. 4. Upper paramedian incision: right side, biliary tract surgery, cholecystectomy; left side, splenectomy, gastrectomy, vagotomy, hiatal hernia repair. 5. Lower paramedian incision: right side, appendectomy, small bowel resection; left side, sigmoid colon resection. 6. McBurney incision: appendectomy. 7. Inguinal incision: inguinal herniorrhaphy. 8. Infraumbilical: umbilical herniorrhaphy.
Positioning
After abdominal surgery, patients are often positioned on the side until laryngeal reflexes have started to return. The patient is then placed in a semi-Fowler position to ease the tension on suture lines and to promote respiratory effort. After some procedures on the stomach or esophagus, strict aspiration precautions with the head of the bed elevated to 30 degrees may be required. After hemorrhoidectomy, the patient may assume any position of comfort, which is most likely on the right or left side.
Dressings and Drains
All dressings should be checked. The nurse must know what kind of incision was used and whether any drains are in place. Drains are discussed in more detail in the specific procedure sections. Drainage should be assessed for character, volume, and odor. The nurse should determine who can or should remove the dressing if needed. Some surgeons reinforce the abdominal incision and dressing with a binder; they believe that this gives the incision valuable support. Others, however, believe that binders restrict respiratory effort and that this disadvantage outweighs the limited advantage of incisional support.
Because drainage may be copious after gastrointestinal surgery, frequent reinforcement of dressings may be necessary. Ask the surgeon for anticipated or expected amounts of drainage for the patient and procedure. If drainage becomes excessive (more than expected from the particular procedure), the surgeon should be notified and the incision directly inspected.
All tubes should be connected to the appropriate drainage devices, usually straight-gravity or closed-bulb suction drainage, as the surgeon specifies. Nasogastric tubes will usually be attached to constant or low intermittent wall suction. Maintenance of the patency of these tubes is one of the most important nursing functions after gastrointestinal surgery. Irrigation of nasogastric tubes after esophageal or gastric surgery should be directed by the surgeon’s orders.
Respiratory Function
The promotion of good respiratory function is a nursing priority for the patient who has had abdominal surgery. Painful abdominal incisions cause the patient to restrict chest expansion voluntarily, which is especially true with high abdominal incisions. The patient must be coached often in sustained maximal inspirations, coughing, and changing position to prevent respiratory complications. Assisting the patient with splinting of the incision and judicious use of pain medications aid in deep breathing and coughing and help to prevent the development of atelectasis. Coughing and incentive spirometry in the postanesthesia care unit (PACU) setting are valuable in promotion of respiratory function.
Frequent assessment of breath sounds during the postoperative period can alert the nurse to impending respiratory problems. An unrecognized injury to the diaphragm during upper abdominal surgery is possible and can result in respiratory distress. Positive pressure ventilation during anesthesia can also lead to respiratory problems. Breath sounds must be monitored closely to assess for pneumothorax and other respiratory complications.
Fluid and Electrolyte Balance
Fluid and electrolyte shifts or losses can be substantial during gastrointestinal surgery. Losses continue after surgery through gastrointestinal tubes or other drains and through third-spacing of fluid into the abdomen. For this reason, accurate intake and output records are mandatory. This recording begins with the intake and output report from the anesthesia care provider, which should be the first PACU entry. All drainage from incisions should be included in the assessment of electrolyte balance. Frequent serum electrolyte determinations may be necessary if losses are great. Intravenous fluids are used for replacement for at least the first 24 hours after surgery and at least until the nasogastric tube is removed. See Chapter 14 for a discussion of the specific problems in electrolyte loss from the gastrointestinal tract.
For patients who do not arrive in the PACU with a urinary catheter in place, urinary retention can become a problem after abdominal surgery because of incisional pain, opioid analgesics, anesthetics, and physiologic splinting. Urine output should be checked frequently, and accurate records should be kept. The nurse should also check for bladder distention and document the findings; the patient might not recognize the need to void, particularly after spinal or epidural anesthesia. Ultrasound examination of the bladder with a bedside scanner can aid in assessment of bladder status. The patient should void within 4 to 6 hours after surgery. If the patient has not voided by the time of discharge from the PACU, the receiving unit should be notified to check specifically for urinary retention. If permissible, the male patient may benefit by standing to void. If urinary retention causes pain, distends the abdomen, or becomes prolonged, intermittent urinary catheterization may become necessary. Patients who have had extensive surgery will return to the PACU with a urinary catheter in place. Accurate output records should be maintained. For an adult with normal renal function, a minimum of 30 mL/hour of urine output is expected; if less than this, the surgeon should be notified. Indwelling urinary catheters should be removed as soon as possible and as the patient’s conditions warrants to reduce the risk of infection.1
Care of the Patient With Nasogastric or Intestinal Tubes
Anesthesia and manipulation of the viscera during surgery cause gastric and colonic peristalsis to diminish or disappear completely for up to 5 days after surgery. Nasogastrointestinal or nasogastric tubes can be used after surgery to prevent the sequelae of this hypomotility although less frequently than they were used in the past. Edema at the operative site also can result in temporary obstruction.
If gastric decompression is needed, short tubes are generally used; long intestinal tubes are no longer used. Short tubes used include the Levin and the plastic Salem sump, which is a double-lumen nasogastric tube and is the most commonly used tube. The double lumen prevents excessive negative pressure from developing when the tube is connected to suction. An antireflux valve is used to prevent gastric contents from leaking out of the vent lumen. To benefit from the double-lumen tube, however, it is important that the lumen exposed to air is not obstructed and is “sumping” or the tube will become obstructed by sucking on the gastric wall.2
When the patient returns from the operating suite with a nasogastric tube in place, the nurse must ascertain why the tube was placed, where it was placed, and whether it should be connected to suction or to straight-gravity drainage. The physician often orders the tube to be connected to low-pressure intermittent suction (20 to 80 mm Hg). Usually only low-pressure intermittent suction is used because excessive negative pressure in either the stomach or the bowel pulls the mucosa into the lumen of the tube and can cause traumatic ulcers. For double-lumen nasogastric tubes, continuous suction at 40 to 60 mm Hg is usually ordered and is necessary for the tube to function properly. Keeping the open lumen above the midline improves functioning of the double-lumen tube.
Tube Patency
Patency of the tube must be ensured. The nurse should observe for drainage from the tube. All characteristics of the drainage must be noted: consistency, color, odor, quantity, and any deviations from the expected drainage. After gastrointestinal surgery, initial drainage may be bright red in small volumes but should become dark or thin, watery, cherry pink–colored liquid after 24 hours. Bloody drainage should not be expected from a nasogastric tube placed only for decompression of the stomach after biliary tract, liver, or spleen surgery. If no drainage is present, if the patient’s abdomen becomes distended, or if the patient vomits around the nasogastric tube or has nausea, the tube may be clogged or the suction apparatus may be malfunctioning; check both. For maintenance of the patency of the nasogastric tube, irrigation with 20 to 30 mL of normal saline solution can be performed every hour or more frequently if necessary. Before irrigating the tube, check with the surgeon regarding the permissibility of nasogastric tube irrigation. Plain water in 20-mL amounts can be used to irrigate the tube without creation of electrolyte abnormalities. Larger amounts of plain water should not be used when irrigating for gastric bleeding because of the large volume and the risk of electrolyte alterations. Frequent irrigations increase the loss of electrolytes from the gastrointestinal system. Some surgeons advocate the use of air to irrigate the nasogastric tube to maintain patency. Only air should ever be passed through the second (“sump”) lumen of the double-lumen tube.

Full access? Get Clinical Tree







