FIG. 32.1 Frontal section through outer, middle, and internal ear. CN, Cranial nerve. (From Patton KT, Thibodeau GA: Anatomy and physiology, ed 9, St. Louis, MO, 2016, Elsevier.)
If surgery has been performed near the brain (e.g., the inner ear), check for clear fluid in the ear or on the dressings that may indicate cerebrospinal fluid leakage. Use of aseptic technique for all dressing assessment and protection from infection are especially important elements in the care of the patient who has undergone surgery on the ears, because infection can be transmitted easily to the meninges and the brain. The outer ear is highly vascular and susceptible to circulatory damage and excoriation. The outer ear may even become necrotic if circulation is impaired by poor positioning or excessive pressure of a dressing. Assessment of the dressing should therefore include proper positioning.2,3
Positioning of the postanesthesia patient who has undergone ear surgery should be indicated by the surgeon. If position is unimportant, the patient should be allowed to assume a position of comfort, usually with the head of the bed elevated to facilitate drainage. Generally, lying on the unoperated side is most comfortable for the patient.
Nausea, vertigo, and nystagmus are common in patients after ear surgery. The patient may minimize discomfort by remaining in the position ordered, moving slowly, and avoiding quick jerky movements.2,3 The patient should be advised to take slow deep breaths through the mouth to minimize nausea. Antiemetic drugs and sedatives such as a 5-HT3 antagonist (e.g., ondansetron [Zofran]) may be ordered for prevention or treatment of nausea and vertigo. The nurse should avoid jarring the bed. When approaching the patient, the nurse should place a hand on top of the patient’s head as a reminder not to turn suddenly when the nurse speaks. Sudden turns should be avoided, and movement should be slow in patient transport. Particular attention must be paid to maintaining the integrity of the airway should nausea and vomiting occur.
Patient education should include not allowing water in the ears such as with swimming or during showering/hair washing. Special ear plugs can be purchased. Some surgeon’s offices have someone who can make ear plugs so they are a custom fit. Instructions should also include not blowing the nose forcefully, especially in the case of myringotomy with tube placement. Surgeons have varying preferences regarding these instructions; therefore, care should be made to give instructions pertinent to that specific practitioner.
Special Considerations
Myringotomy
Myringotomy is the most common procedure performed on infants and small children; it is performed for otitis media related to eustachian tube dysfunction. The procedure may also be performed in adults for similar reasons and for barotrauma or hyperbaric chamber treatment. Children will often exhibit frequent ear infections or symptoms of pain, poor coordination, hearing loss, or speech delays.4 After a hole in the tympanic membrane is created with a myringotomy blade, the surgeon will place a pressure-equalizing tube to maintain patency. There are several types of tubes available and are placed according to the surgeon’s preference.5
Special pediatric considerations must be given in the immediate postanesthesia phase to airway management, safety, parental involvement, and outpatient teaching.3 This procedure is commonly bilateral in children; however, in adults it is commonly unilateral.4 A small piece of sterile cotton can be placed loosely in the external ear to absorb the drainage that commonly occurs. The cotton should be changed when saturated to avoid contamination.
Mastoidectomy
A firm bulky dressing is placed over the ear and held in place with a circular head bandage after mastoidectomy.5 This dressing may be reinforced, if necessary, but should be changed only by the physician. Minimal serosanguineous drainage may be expected, but bright bloody drainage should be reported to the surgeon.
The patient should be placed in a position of comfort, usually on the nonoperative side. Grafts are often taken from the arm or leg for radical mastoidectomy, and the donor sites should be assessed for drainage and treated according to facility or department policy and surgeon preference. Cranial nerve assessment is also recommended. Dizziness and vertigo are common after mastoidectomy and can be treated with the previously mentioned measures.2,3
Tympanoplasty
Patients are usually positioned on the unoperated side after tympanoplasty. Care must be taken to keep bandages and grafts in place. Patients should be instructed not to blow the nose or cough and to avoid sneezing to prevent disruption of the grafts. Instruct the patient to open the mouth if sneezing occurs so that the force of the sneeze has a larger exit opening, keeping the pressure out of the eustachian tubes.
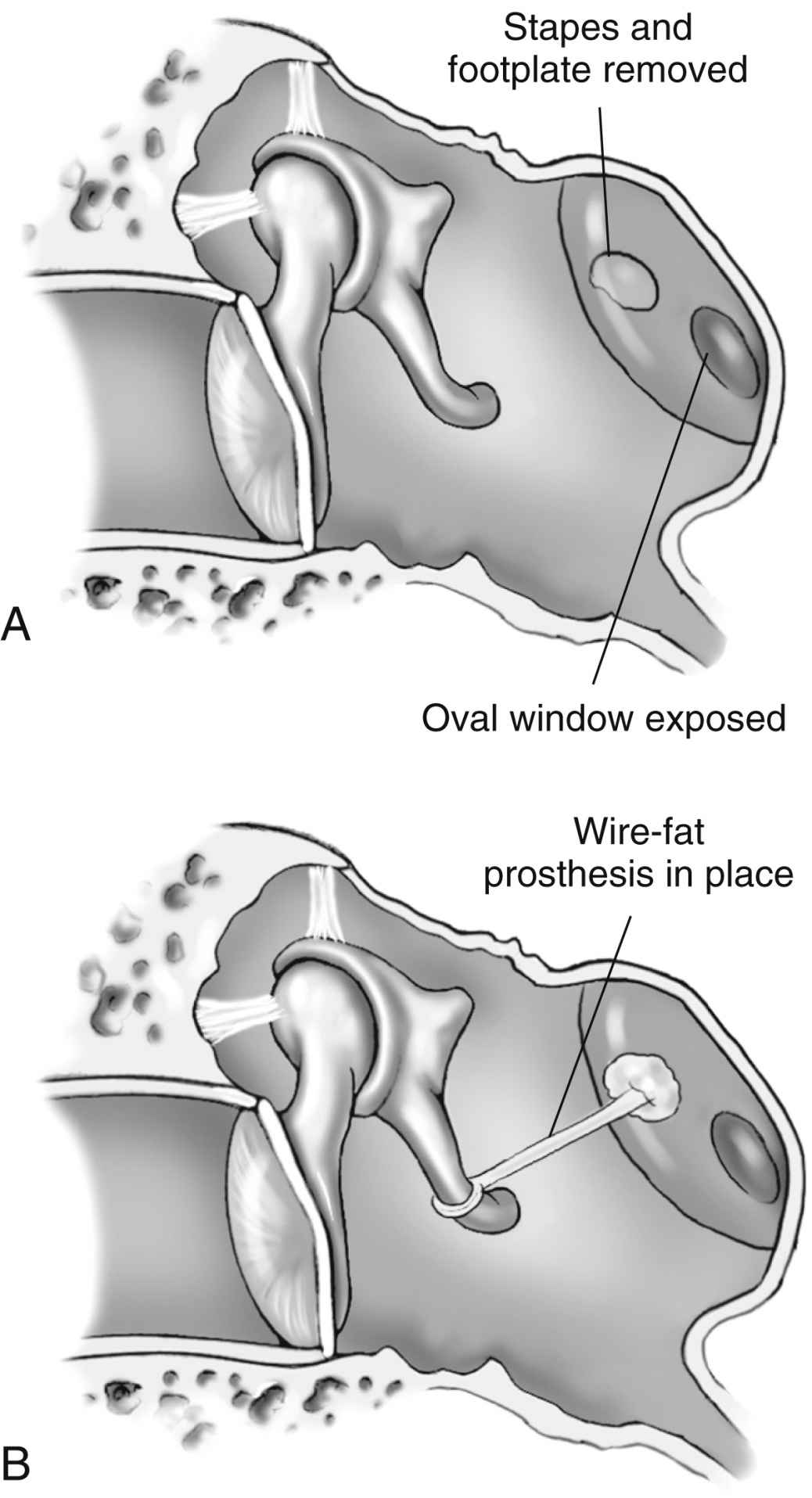
Stapedectomy
Cochlear Implant
Patients who have undergone a cochlear implant need the same postanesthesia care as any other patient for ear surgery. Verification of the integrity of the facial nerve is important. These patients do not have hearing immediately after surgery and need emotional support and a means of communication such as pen and paper, white board and markers, or a sign language interpreter.3
Surgery on the Nose and Sinuses
Nasal and sinus surgery can be accomplished with local or general anesthesia. The disposition of the patient is determined by the nature and type of surgery and anesthesia and by the perianesthesia course related to complications and sedation required in the PACU.6 Although no longer common with the use of endoscopic procedures, overnight observation of the patient in an inpatient setting may be necessary before discharge from the hospital. An inpatient stay may be considered for patients with comorbidities such as obstructive sleep apnea because they will have some difficulty with use of the continuous positive airway pressure (CPAP) machine owing to the nasal splints or packing.7 The anatomy of the nasal cavity is shown in Fig. 32.3.
Nasal Surgery
Patients admitted to the PACU after nasal surgery, such as septoplasty, rhinoplasty, functional endoscopic sinus surgery, or balloon sinuplasty, should be placed in a semi-Fowler position to promote drainage, reduce local edema, minimize discomfort, and facilitate respiration. Some postoperative serosanguineous drainage is expected; however, the nurse should observe closely for gross bleeding.2 Loss of vision is a complication that may indicate intraoperative breach of the orbital cavity and requires immediate attention by the surgeon. The patient is usually admitted with one or both nostrils packed and a mustache dressing in place to absorb any drainage from the packing.5 The position of the nasal packs and the amount of drainage should be checked frequently as packs may shift, causing airway obstruction. The mustache dressing may be changed as necessary; two or three changes within a 4-hour period are not unusual. Another method commonly used to facilitate postoperative drainage is the insertion of nasal stents. This approach affords more comfort and permits nasal breathing.
The back of the patient’s throat should be checked frequently for blood. Frequent belching (from the accumulation of blood in the stomach), nausea, frequent swallowing, and the classic signs of hemorrhage, such as tachycardia, are additional indicators of bleeding.3 The patient should be instructed not to blow the nose or swallow secretions but to expectorate them into a basin. An ample supply of disposable tissues along with an emesis basin should be placed within easy reach of the patient.
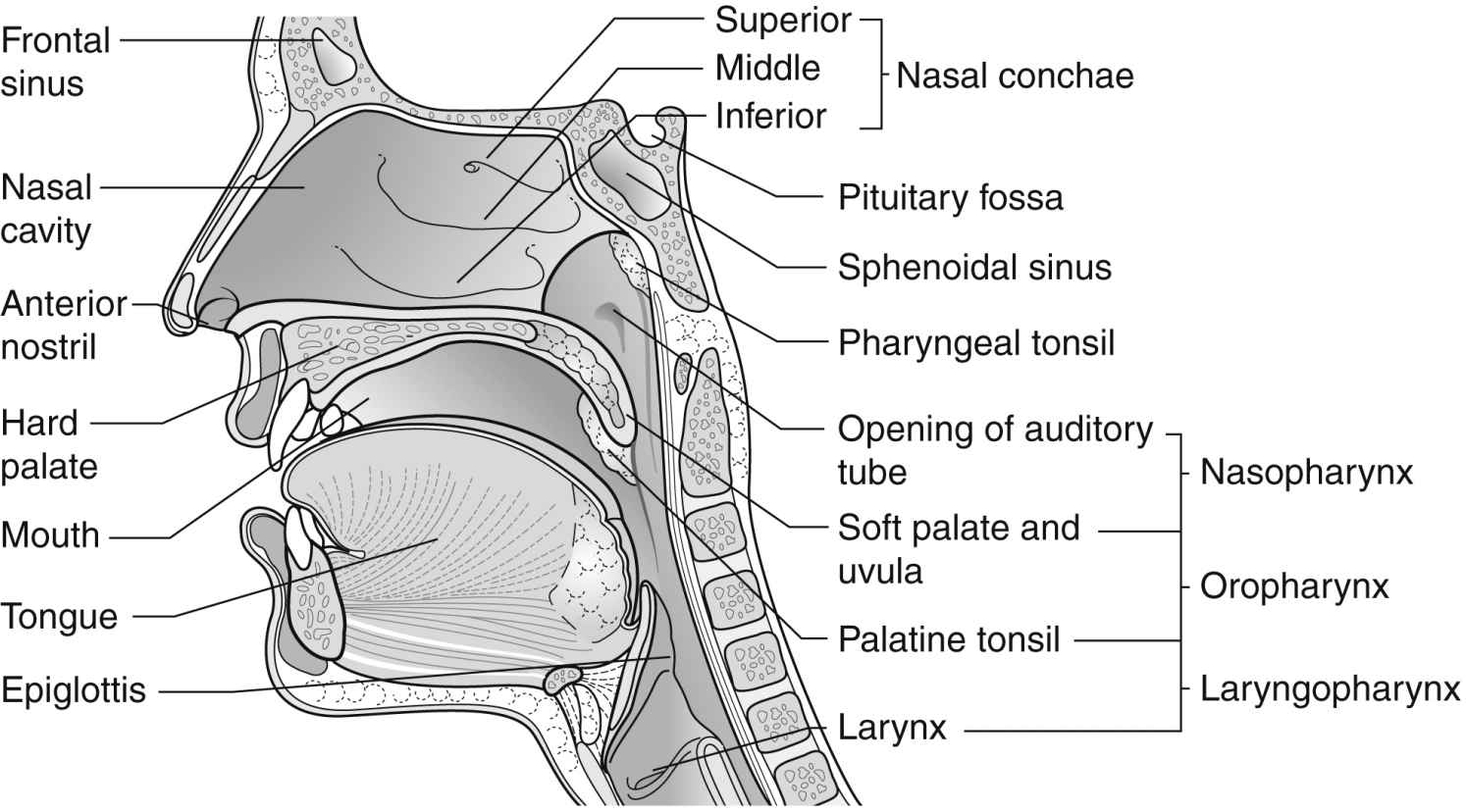
FIG. 32.3 Sagittal section of the nose, mouth, pharynx, and larynx. (From Watson R: Anatomy and physiology for nurses, ed 13, London, UK, 2011, Baillière Tindall.)
Airway obstruction or laryngeal spasm can occur if a postnasal pack accidentally slips out of place.1 A flashlight, scissors, and a hemostat for emergency removal of nasal packing and emergency airway equipment must be kept readily available at the patient’s bedside.
Oral fluids are withheld until bleeding is controlled, vomiting and nausea have subsided, and independent airway management has been established. Antiemetics are ordered to alleviate nausea and vomiting.
Mouth breathing, bleeding, and postnasal drainage create dryness and an offensive taste and odor in the patient’s mouth; therefore, once the gag reflex has returned, oral hygiene is a priority. Lemon-glycerin swabs or mouthwash may be used for mouth care and to make the patient more comfortable. An ointment may be applied to the lips to prevent drying and cracking.
Ice packs across the nose or to the cheeks may be ordered to minimize pain, edema, discoloration, and bleeding. These ice packs should be small and lightweight and have a covering to prevent pack sweating or frostbite to patient skin.
Oxygen should be delivered via cool mist mask through a face tent, because dry mucous membranes often produce coughing, dyspnea, and decreased respiratory exchange. Ice chips may be a comfort measure if intake is warranted.
When assessing the patient for pain and discomfort, the nurse should inquire about pain to the roof of the mouth and front teeth; this occurs from the edema underneath the septum. Most patients will complain of burning in the nose and a headache similar to the pain they experienced with sinus pressure before surgery.
Sinus Surgery
After surgery on the sinuses, the patient is usually admitted to the PACU with packing or splints in place. Reports of feelings of numbness in the upper lip and teeth are not unusual. After general anesthesia, the patient should be positioned well on one side to prevent aspiration of drainage. The patient should be placed in a semi-Fowler position to promote drainage and minimize edema. The same general care, including oral hygiene and instructions to the patient not to blow the nose, should be followed as for the patient with nasal surgery.1–3
Surgery on the Tongue
The tongue occupies a large portion of the floor of the mouth. Surgery on the tongue generally involves excision of benign or malignant lesions, correction of congenital anomalies, or repair of traumatic lacerations. Lesions may be excised without associated neck dissection; however, when the lesion is malignant, surgical treatment usually involves a combined operation that may include radical neck dissection and resection of both the mandible and the tongue.2,5
Local anesthesia is used for minor surgical procedures such as excision of lesions and repair of lacerations. More extensive surgical procedures on the tongue or procedures in children (e.g., for ankyloglossia) require general anesthesia with endotracheal or nasotracheal intubation.
After surgery, the patient must be placed in a side-lying position with the head slightly dependent to allow for the drainage of secretions out of the mouth. When protective reflexes have returned, the patient should be placed in a sitting position to promote venous and lymphatic drainage.
Maintenance of the airway is the most crucial nursing concern. Suctioning equipment with soft-tipped catheters must be immediately available at the bedside.1,3 The patient should be instructed to allow saliva to run out of the mouth. A wick of gauze is placed in the patient’s mouth to assist in the elimination of secretions. Swelling of the tongue can occur and obstruct the airway; therefore, frequent assessment is required. An intubation tray should be readily available.
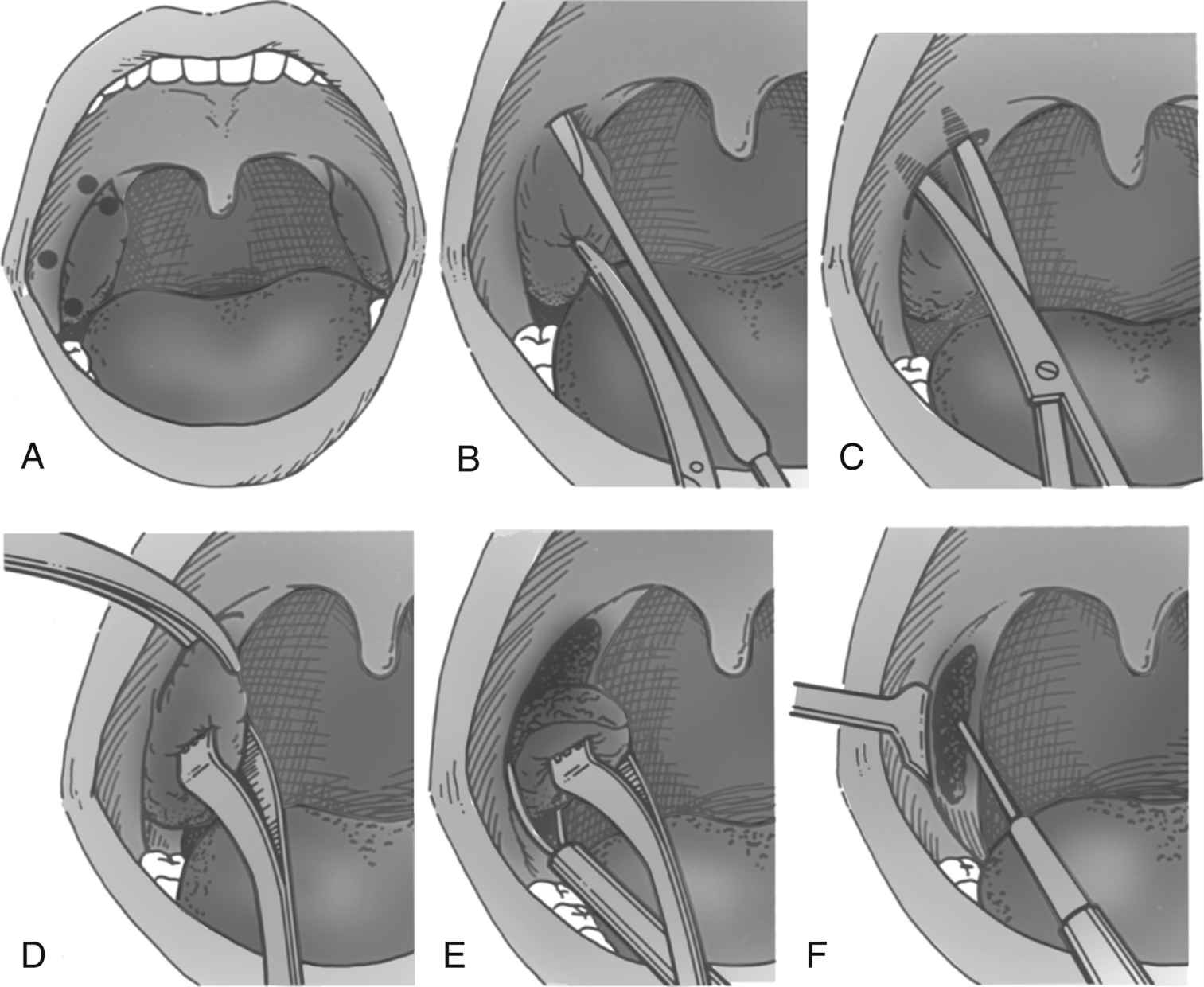
FIG. 32.4 Method of dissection tonsillectomy. A, Points of infiltration for local anesthesia. B, Start of incision with tonsil knife at attachment of anterior pillar to tonsil superiorly. C, Separation with scissor dissection of superior pole of tonsil. D, Continuation of dissection of tonsil from its attachment to pillars and bed of tonsillar fossa. E, Separation of tonsil with snare at lower pole including plica triangularis. F, Hemostasis. (From Luckman J, Sorenson KC: Medical-surgical nursing, ed 3, Philadelphia, PA, 1987, Elsevier.)
Because of the vascular nature of the tongue and oral cavity, postoperative bleeding may be a problem. If excessive bleeding occurs, local pressure should be applied until the surgeon can be notified and repair can be performed in the operating room.
Throat Surgery
Surgery on the throat and neck is generally accomplished with general anesthesia.6 Aside from routine care and assessment, specific postanesthesia care for the patient who has undergone surgery on the throat involves: (1) close observation for bleeding from the surgical site, (2) maintenance of a patent airway, (3) prevention of aspiration of secretions, and (4) awareness of possible cerebral neurologic complications that may develop.
The most common procedures are tonsillectomy, either alone or in combination with adenoidectomy, and tracheostomy. Other procedures performed on the throat include laryngoscopy with or without biopsies, laryngectomy, palatoplasty, uvulectomy, and uvulopalatopharyngoplasty.
Tonsillectomy and Adenoidectomy
Most patients who undergo tonsillectomy (Fig. 32.4) and adenoidectomy (T&A) are children and young adults. However, the number of young children who undergo T&A continues to be reduced each year as a result of improved antibiotic treatment. Patients who have undergone T&A and are admitted to the PACU alert and oriented can be positioned on their backs with the head elevated 45 degrees. Patients who return after general anesthesia and are unconscious or semiconscious must be placed in the tonsillar position—well over on the side with the face partially down. The Trendelenburg position can be used to facilitate drainage. The patient’s airway and chest expansion must be in full view of the nurse to ensure maximal respiratory integrity at all times. In this position, secretions are easily drained from the mouth.2 An oral airway should be left in place until the swallowing reflex has returned and the patient can handle secretions. The patient should be advised to expectorate secretions as much as possible and to try not to cough, clear the throat, blow the nose, or talk excessively. An ice collar can be applied to minimize pain and postoperative bleeding. The administration of cool humidified air to the patient after T&A provides comfort, helps to minimize swelling, and supplies oxygen. As soon as oral intake is permitted, ice chips should be offered to moisten the throat and reduce swelling.
The most common complication of T&A is postoperative bleeding for both children and adults. Frequent swallowing, clearing of the throat, and vomiting of dark blood are indications of possible bleeding. The nurse should frequently check the back of the throat with a flashlight for trickling blood. If any of the cardinal symptoms of hemorrhage occur, such as decreased blood pressure, tachycardia, pallor, and restlessness, the surgeon should be notified.3 Because the surgeon may want to treat a bleeding episode in the PACU, a tonsil tray should be available (Box 32.1). An electrocautery unit from the operating room and appropriate illumination with a headlight should also be available along with suction equipment. Postoperative bleeding after T&A can often be controlled with the application of vasoconstrictors via nasal packing with pressure. If significant bleeding occurs, however, the patient may have to return to the operating room for suturing or cauterizing of blood vessels.
With the advent of laser dissection of tonsils and adenoids, the potential for bleeding is significantly decreased.8 As with all methods of dissection, swelling can occur; therefore, observation and measures to alleviate swelling are crucial. When the patient is conscious and the reflexes have returned, ice chips and fluids may be offered. Oral liquids should be started with caution as the tonsillar beds are usually infiltrated with a local anesthetic. The nurse should have suction readily available in the case of choking or difficulty swallowing. Some practitioners prefer patients not to use straws so not to precipitate bleeding. Oral hygiene, including alkaline mouthwash, may provide comfort. Ointment should be applied to the lips to prevent drying and cracking.
Patients who have undergone T&A are especially prone to laryngospasms and must be observed closely for patency of the airway.1 Airway obstruction may be created by swelling of the palate or nasopharynx, swelling in the retropharyngeal space, or swelling of the tongue and nose. If laryngospasm does occur, positive pressure via a bag-mask device and 100% fraction of inspired oxygen (FiO2) is administered. If this method is not effective in breaking the spasm, reintubation and administration of succinylcholine and opioids as prescribed may be necessary.1,6

Full access? Get Clinical Tree