Chapter 19 Cardiac pacing and implantable cardioverter/defibrillators
Cardiac pacing has rapidly evolved since its introduction by Zoll in 1952.1 The technological knowledge gained in pacing has assisted in the even more rapidly advancing field of implantable cardioverter/defibrillators (ICDs). Although implantation and follow-up of permanent pacemakers and ICDs are in the domain of appropriately trained cardiologists, intensive care physicians should be familiar with such devices as a significant number of critically ill patients will have them in situ. It is also essential, when urgent pacing is required, that the intensivist is skilled in all aspects of temporary pacing, including lead insertion and testing.
CARDIAC PACING IN BRADYARRHYTHMIAS2,3
ELECTRODES
BIPOLAR (Figure 19.2)
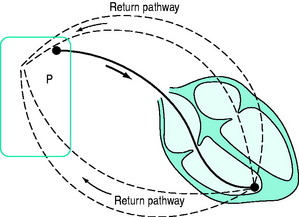
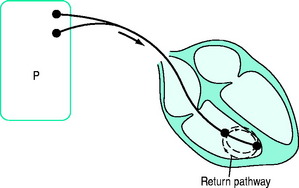
A bipolar lead has two conducting wires surrounded by a layer of insulation. Electric current travels down one wire to an electrode (usually the distal), passes through cardiac tissue to cause depolarisation, and returns to the pacemaker via the second electrode. Inappropriate sensing of EMI or myopotentials is uncommon. Bipolar pacing is the method of choice for temporary pacing. If one limb fails, a bipolar system can be converted to a unipolar system (see Figure 19.1) by connecting the other limb to one pacemaker pole (usually positive). The other pole (usually negative) is connected to an electrocardiogram (ECG) skin electrode to complete a unipolar pacing circuit.
PACING SITES
PACEMAKER MODES
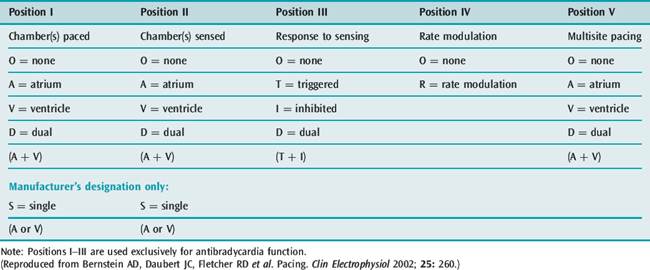
The North American Society of Pacing and Electrophysiology (NASPE) and the British Pacing and Electrophysiology Group (BPEG) developed the NBG code4 for pacing. It is a generic code used to identify modes of pacing (Table 19.1). The code was updated in 2002 to include multisite pacing therapy (position V).5
SPECIFIC PACING MODES
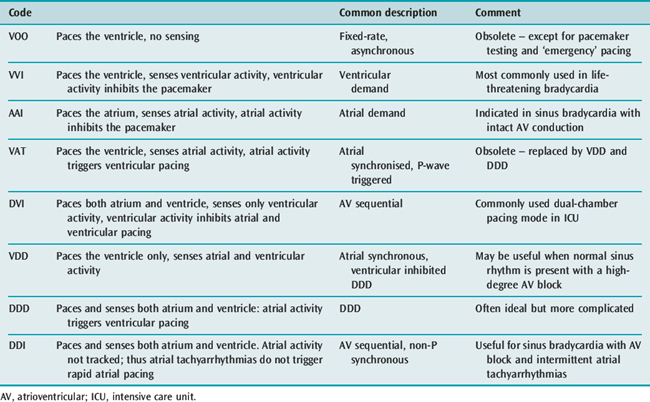
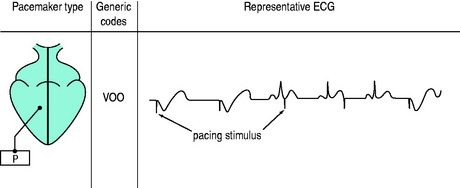
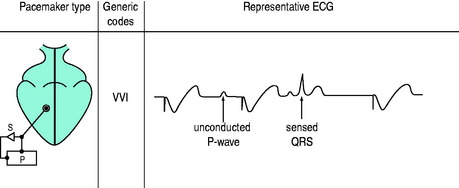
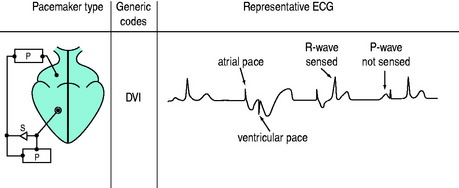
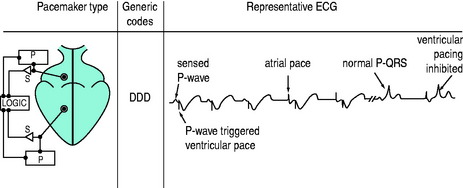
The three-position code (Figure 19.3) is adequate to describe emergency temporary pacing and most forms of permanent pacing in the intensive care unit (ICU) (Table 19.2).
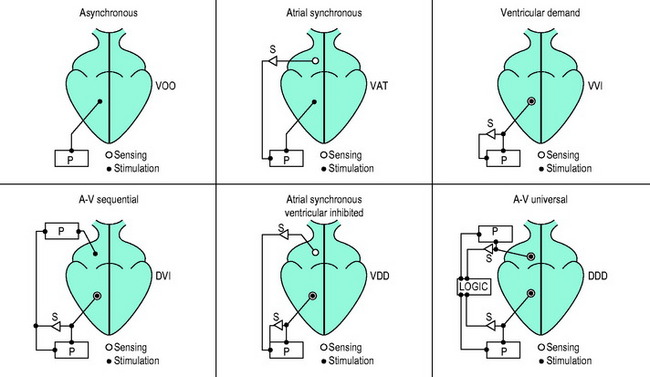
Figure 19.3 Examples of pacemaker modes and their three-position (letter) codes. P, pacemaker; S, sensing.
SINGLE-CHAMBER PACING
DUAL-CHAMBER PACING
Two sets of electrodes are required (atrial and ventricular).
DVI (AV SEQUENTIAL) PACING
Atria and ventricles are paced in sequence (Figure 19.7). After a stimulus is delivered to the atrium, there is a delay and an impulse is then delivered after atrial stimulation, to the ventricles. If AV conduction is successful, the ventricular output of the pacemaker is inhibited; otherwise the ventricle is paced. The advantage of this mode is that the atria and ventricles usually contract in sequence. To maintain AV synchrony in the absence of atrial sensing, the pacemaker discharge rate must be greater than the spontaneous atrial rate; asynchronous atrial pacing can precipitate AF. Self-inhibition (‘cross-talk’) can occasionally occur, that is, inappropriate detection of the atrial pacing stimulus by the ventricular channel. If there is no escape rhythm, asystole may result. DVI pacing is indicated when there is impaired AV conduction with an atrial bradycardia. It is of no value when atrial tachyarrhythmias are present.
VDD (ATRIAL SYNCHRONOUS VENTRICULAR INHIBITED) PACING
This mode paces only the ventricle. Sensing takes place in both atrium and ventricle. A sensed P-wave triggers ventricular pacing. VDD pacing is used in some permanent pacemaker systems as a single-lead system capable of pacing the ventricle in response to atrial sensing (from an electrode situated in the intra-atrial part of the lead) with ventricular electrodes at the apex of the RV.
DDD PACING
There is pacing and sensing in both chambers (Figure 19.8). An atrial impulse will trigger a ventricular output and simultaneously inhibit an atrial output. If the impulse is conducted normally to the ventricle, the ventricular output is then inhibited, as with the DVI mode. Upper rate-limiters prevent the pacemaker from following excessive atrial activity with paced ventricular responses. DDD pacemaker function depends on the underlying cardiac rhythm:
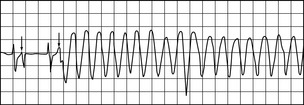
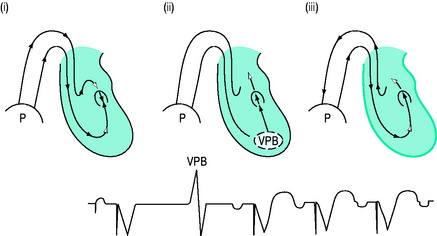
Self-inhibition can be prevented by introducing a ventricular blanking (refractory) period coinciding with the atrial pacing stimulus. With DDD and VDD pacing, re-entry pacemaker-mediated ‘endless-loop’ tachycardias are possible.7 These are commonly initiated by a ventricular premature beat (Figure 19.9) conducted retrogradely to the atria, where it is sensed and ventricular pacing is triggered with an endless loop: the circuit’s anterograde limb is the pacemaker, and the retrograde limb is via the AV node. Conversion to asynchronous (non-sensing) mode or DDI or increasing the postventricular atrial refractory period (PVARP) will prevent endless-loop tachycardia.
HAEMODYNAMICS OF CARDIAC PACING
In the normal heart, cardiac output increases three- to fourfold during exercise, due mainly to increased heart rate and increases in stroke volume. Atrioventricular synchrony – the normal activation sequence of the heart in which the atria contract first and then, after an appropriate delay, the ventricles contract – contributes only about 20% of cardiac output.8 Thus the ability of pacemakers to increase heart rate is paramount, although AV synchrony may on occasions be vital (e.g. in low-cardiac-output states). Many permanent pacemakers are rate-adaptive. When temporary pacing is used, the arbitrary back-up rate of 70–80 beats/min may need to be increased if oxygen delivery is inadequate. For life-threatening bradyarrhythmias, increasing heart rate with VVI mode pacing is the treatment of choice. Permanent VVIR pacing (most commonly using an activity or respiration sensor) will allow heart rate modulation. However, in the ICU, adaptive rate changes may not occur. For example, no activity will be sensed in a patient with septic shock, even when the cardiac output is low.
During VVI and VVIR pacing the atria and ventricles beat independently and AV synchrony is lost. Occasionally this can have deleterious effects and cause a ‘pacemaker syndrome’.9 The pacemaker syndrome is, however, a complex of clinical signs and symptoms associated with loss of AV synchrony. A fall in blood pressure coinciding with the onset of ventricular pacing is consistent with the pacemaker syndrome. It was initially recognised with VVI pacing but can occur with any pacing mode if there is AV dissociation, and can be compared to the effects in patients with complete heart block and AV dissociation. The atria contract against closed AV valves with significant regurgitation of blood into the pulmonary and systemic circulation. Blood pressure, stroke volume and cardiac output may fall. The pacemaker syndrome can be eliminated by restoring AV synchrony.
Emergency and long-term haemodynamic effects of DDD or AAI pacing are generally superior to VVI pacing. In studies of patients with permanent pacing, there is a consistent lower mortality with DDD or AAI pacing compared to VVI pacing, and a significantly lower incidence of AF.2 DDD and/or DVI pacing requires two pacing leads, one each in the RA and RV. Under appropriate conditions AAI and DVI pacing provide AV synchrony but not rate adaptation. DDD pacing will usually ensure AV synchrony and heart rate responsiveness, provided the SA node is normal.
Dual-chamber pacemakers require the AV interval to be set as close as possible to the normal P-R interval (140–200 ms). Traditionally, the pacing AV interval is arbitrarily set at about 150–200 ms. If interatrial conduction time (between the RA and LA) is significantly prolonged, the LV may contract before or at the same time as the LA, causing DDD pacemaker syndrome10 with decreased stroke volume and cardiac output (due to LA contraction against a closed mitral valve). Hence, if there is evidence of inadequate cardiac output or impaired oxygen delivery, the AV interval may need to be increased appropriately, or optimised using thermodilution cardiac output or echocardiographic techniques at various AV intervals.