![]() Hemodynamic instability (presyncope, angina, altered mentation, pulmonary edema) secondary to:
Hemodynamic instability (presyncope, angina, altered mentation, pulmonary edema) secondary to:
![]() Bradydysrhythmias:
Bradydysrhythmias:
![]() Sinus bradycardia
Sinus bradycardia
![]() Sinus node dysfunction
Sinus node dysfunction
![]() Atrioventricular (AV) node conduction blocks (second and third degree)
Atrioventricular (AV) node conduction blocks (second and third degree)
![]() Acute myocardial infarction with bifascicular block, alternating bundle branch block, new left bundle branch block (LBBB), escape rhythm <40 bpm
Acute myocardial infarction with bifascicular block, alternating bundle branch block, new left bundle branch block (LBBB), escape rhythm <40 bpm
![]() Malfunctioning permanent pacemaker
Malfunctioning permanent pacemaker
![]() Electrolyte/metabolic disturbances (i.e., hyperkalemia) if medical therapies fail or are unavailable
Electrolyte/metabolic disturbances (i.e., hyperkalemia) if medical therapies fail or are unavailable
![]() Post–cardiac surgery (i.e., valve replacement)
Post–cardiac surgery (i.e., valve replacement)
![]() Thoracic trauma (i.e., cardiac contusion)
Thoracic trauma (i.e., cardiac contusion)
![]() Other (i.e., lyme carditis, endocarditis)
Other (i.e., lyme carditis, endocarditis)
![]() Tachydysrhythmias (overdrive pacing, typically transvenous only):
Tachydysrhythmias (overdrive pacing, typically transvenous only):
![]() Supraventricular tachycardia (SVT)
Supraventricular tachycardia (SVT)
![]() Ventricular tachycardia (VT)
Ventricular tachycardia (VT)
![]() Transvenous Pacing—same as above, but also including:
Transvenous Pacing—same as above, but also including:
![]() Failure or nontolerance of transcutaneous pacing
Failure or nontolerance of transcutaneous pacing
![]() Bridge to permanent pacemaker placement
Bridge to permanent pacemaker placement
![]() High risk of progression to complete heart block
High risk of progression to complete heart block
![]() Overdrive pacing
Overdrive pacing
CONTRAINDICATIONS
![]() Absolute
Absolute
![]() Asymptomatic, stable rhythms (i.e., first-degree AV block)
Asymptomatic, stable rhythms (i.e., first-degree AV block)
![]() Prosthetic tricuspid valve (transvenous only)
Prosthetic tricuspid valve (transvenous only)
![]() Relative
Relative
![]() Severe hypothermia (may be physiologic bradycardia; can induce fibrillation)
Severe hypothermia (may be physiologic bradycardia; can induce fibrillation)
![]() Brady-asystolic arrest >20 minutes
Brady-asystolic arrest >20 minutes
![]() Drug-induced dysrhythmias (although can be utilized as last resort if antidote fails)
Drug-induced dysrhythmias (although can be utilized as last resort if antidote fails)
TRANSCUTANEOUS PACING PROCEDURE
![]() Landmarks
Landmarks
Pacer pads should preferentially be placed over the precordium anteriorly and in the interscapular paraspinous region posteriorly. Anterolateral pad placement is also acceptable.
![]() Supplies
Supplies
![]() Cardiac monitor with pacemaker capabilities (if electrocardiogram [ECG] monitor is not part of the pacer unit, a separate monitor and adaptor will be required)
Cardiac monitor with pacemaker capabilities (if electrocardiogram [ECG] monitor is not part of the pacer unit, a separate monitor and adaptor will be required)
![]() Adhesive pacing pads
Adhesive pacing pads
![]() ECG electrodes
ECG electrodes
![]() Safety razor
Safety razor
![]() Technique
Technique
![]() Preparation
Preparation
![]() In conscious patients, reassurance and explanation of the procedure, including expectations for discomfort, are extremely important
In conscious patients, reassurance and explanation of the procedure, including expectations for discomfort, are extremely important
![]() Remove excess hair if time permits
Remove excess hair if time permits
![]() Continuous cardiac and pulse oximetry monitoring, intravenous access, and bedside capability for resuscitation, including airway management, defibrillation, and arrhythmia treatment, should be at the bedside before initiation
Continuous cardiac and pulse oximetry monitoring, intravenous access, and bedside capability for resuscitation, including airway management, defibrillation, and arrhythmia treatment, should be at the bedside before initiation
![]() Pacer/Electrode Placement
Pacer/Electrode Placement
![]() Pads are placed as shown in FIGURE 9.1
Pads are placed as shown in FIGURE 9.1
![]() Anterior chest pacing pad (negative charge electrode) is placed over the point of maximal impulse
Anterior chest pacing pad (negative charge electrode) is placed over the point of maximal impulse
![]() If access to the posterior chest wall is limited or difficult, posterior pacer pad may also be placed in cardiac apex/base position (identical to electrical cardioversion placement)
If access to the posterior chest wall is limited or difficult, posterior pacer pad may also be placed in cardiac apex/base position (identical to electrical cardioversion placement)
![]() ECG electrodes should be placed in limb lead positions for monitoring
ECG electrodes should be placed in limb lead positions for monitoring
![]() Pacing
Pacing
![]() Identify pacemaker mode on equipment and turn to “on”
Identify pacemaker mode on equipment and turn to “on”
![]() Set heart rate to 70 bpm
Set heart rate to 70 bpm
![]() Place and maintain one hand in pulse-check position (radial, femoral, or carotid) or observe noninvasive or invasive blood pressure response
Place and maintain one hand in pulse-check position (radial, femoral, or carotid) or observe noninvasive or invasive blood pressure response
![]() In bradyasystole and unconscious patients, set current to 150 to 200 mA and lower in 10-mA decrements; set current at the lowest level that will consistently achieve mechanical capture
In bradyasystole and unconscious patients, set current to 150 to 200 mA and lower in 10-mA decrements; set current at the lowest level that will consistently achieve mechanical capture
![]() In stable and conscious patients, set current to 10 mA and raise in 10-mA increments until mechanical capture is achieved
In stable and conscious patients, set current to 10 mA and raise in 10-mA increments until mechanical capture is achieved
![]() Observe cardiac monitor for pacemaker spikes and electrical capture—“electrical capture” refers to narrow pacemaker spikes followed by typically wide ventricular complexes
Observe cardiac monitor for pacemaker spikes and electrical capture—“electrical capture” refers to narrow pacemaker spikes followed by typically wide ventricular complexes
![]() Monitor constantly for “mechanical capture”—a palpable arterial pulse induced by pacemaker discharges or perfusing blood pressure by noninvasive or invasive blood pressure monitoring
Monitor constantly for “mechanical capture”—a palpable arterial pulse induced by pacemaker discharges or perfusing blood pressure by noninvasive or invasive blood pressure monitoring
![]() Titrate sedation/analgesia/anxiolysis to allow for tolerance of ongoing pacing
Titrate sedation/analgesia/anxiolysis to allow for tolerance of ongoing pacing
![]() Failure to achieve mechanical capture should prompt immediate preparation for transvenous pacer placement
Failure to achieve mechanical capture should prompt immediate preparation for transvenous pacer placement
![]() Complications
Complications
![]() Unrecognized ventricular fibrillation
Unrecognized ventricular fibrillation
![]() Local discomfort
Local discomfort
![]() Cutaneous injury
Cutaneous injury
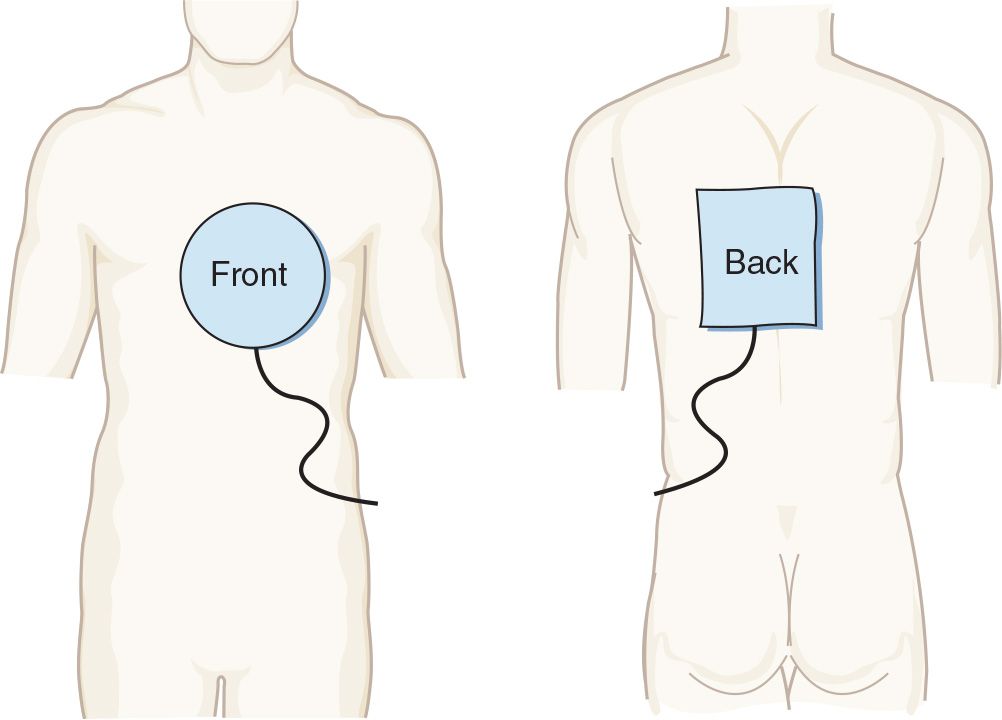
FIGURE 9.1 Proper placement of transcutaneous pacing electrodes. (From Morton PG, Fontaine DK. Critical Care Nursing. 10th ed. Philadelphia, PA: Wolters Kluwer Health; 2012.)
SAFETY/QUALITY TIPS
![]() Procedural
Procedural
![]() The most common causes of failure to capture in transcutaneous pacing are improper electrode placement or large patient size
The most common causes of failure to capture in transcutaneous pacing are improper electrode placement or large patient size
![]() For many patients, adequate amperage will not be possible without aggressive sedation/analgesia
For many patients, adequate amperage will not be possible without aggressive sedation/analgesia
![]() Cognitive
Cognitive
![]() Compared to transvenous pacing, transcutaneous pacing is painful and ineffective. Transcutaneous pacing should be thought of as a brief bridge to transvenous pacing or correction of the underlying disorder.
Compared to transvenous pacing, transcutaneous pacing is painful and ineffective. Transcutaneous pacing should be thought of as a brief bridge to transvenous pacing or correction of the underlying disorder.
![]() Electrical capture is not mechanical capture, and mechanical capture is what counts. Once electrical capture occurs, mechanical capture must be immediately verified using pulses, invasive arterial pressure monitoring, ultrasound, or (most conveniently) pulse oximetry.
Electrical capture is not mechanical capture, and mechanical capture is what counts. Once electrical capture occurs, mechanical capture must be immediately verified using pulses, invasive arterial pressure monitoring, ultrasound, or (most conveniently) pulse oximetry.
![]() Be careful not to mistake ventricular fibrillation or tachycardia for a paced rhythm
Be careful not to mistake ventricular fibrillation or tachycardia for a paced rhythm

Full access? Get Clinical Tree


