(1)
Department of Surgery, R Adams Cowley Shock Trauma Center, University of Maryland School of Medicine, Baltimore, MD, USA
Keywords
Cardiac woundBlunt cardiac ruptureGunshot wound (GSW)Stab woundTraumatic pericardial tamponadePericardiotomyAmerican Association for the Surgery of Trauma Organ Injury Scale (AAST-OIS)Heart injury scale
The heart is the chief mansion of the Soul, the organ of vital faculty, the beginning of life, the fountain of the vital spirits … the first to live and the last to die …
Ambrose Paré (1510–1590)
French Barber-Surgeon
Scope of the Problem
Cardiac wounds are uncommon and seen mainly at urban trauma centers [1]. Despite advancements in surgical care, prehospital treatment, and resuscitation, cardiac injury remains highly lethal. In fact, over several decades survival has not improved, underscoring their lethality [1–6]. One factor that may influence the poor outcome is a mortality bias due to the rapid transit of patients with devastating, non-survivable injuries to the hospital [4, 7].
When considering only the patients who survive to treatment at trauma centers, the incidence of cardiac injury is quite low. Asensio [8] defined the national incidence of penetrating cardiac injuries to be 0.16 % in a study utilizing the National Trauma Data Bank (NTDB), and Rhee [4] defined the penetrating rate as 1 in 210 admissions in a single-center retrospective analysis over 7 years. The number of patients with blunt cardiac rupture who survive to treatment is even less common, with an overall incidence of 0.041 % [9]. It is estimated that 8–86 % of immediate deaths after significant blunt chest trauma are a result of blunt cardiac rupture [9].
Gunshot wounds (GSWs) account for the majority of penetrating cardiac injuries (58–76 %) [1, 4, 8], while stab wounds account for most of the remainder. Unfortunately the mortality associated with GSWs is significantly higher (32.6–84 %) than that of stab wounds (9.7–35 %) [1, 4, 10]. Blunt cardiac rupture is the most lethal of cardiac wounds with rates of mortality approaching 90 % [9].
History of Care
Claude Beck discussed the history of cardiac injuries in a 1926 review article and described three distinct periods: mysticism (ancient times to the sixteenth century), experimentation and observation (sixteenth to the late nineteenth century), and cardiac repair (early twentieth century to present) [11].
Homer’s Iliad [12] includes the earliest known description of cardiac injuries, and authors in antiquity including Hippocrates [13, 14], Aristotle [15], and Galen [16] considered these wounds to be universally fatal [14]. In the sixteenth and seventeenth century, Hollerius [14, 17] promoted the idea that not all wounds to the heart were necessarily mortal, and Wolf [18] and Cabriolanus [14] described healed cardiac wounds.
Morgagni reported the first case of traumatic pericardial tamponade. Larrey described successful treatment of traumatic pericardial tamponade by inserting a catheter through a stab wound to the chest [14]. There was strong resistance to surgeons attempting cardiac repairs, which was typified by Billroth’s assertion that such an attempt “approaches very closely to that kind of intervention which some surgeons would term a prostitution of the surgical act and other madness” [11, 14].
Despite this resistance, Roberts suggested cardiac injuries could be sutured, and Block demonstrated that successful repair of cardiac wounds with survival in a rabbit model was possible [11, 14]. This was ultimately demonstrated in humans in the late 1890s when Axel Cappelen successfully repaired a left ventricular laceration, though the patient subsequently succumbed to sepsis [11, 14].
The new era of cardiac repair began when Ludwig Rehn, at the 26th Congress of the German Surgical Society in 1897, described the successful repair of a right ventricular wound with survival. He stated, “The feasibility of cardiorrhaphy no longer remains in doubt … I trust that this case will not remain a curiosity, but rather, that the field of cardiac surgery will be further investigated. Let me speak once more my conviction that by the means of cardiorrhaphy, many lives can be saved that were previously counted as lost” [19].
The ensuing century saw an explosion of innovation and advancement in cardiac surgery, which included the advent of positive pressure ventilation and cardiopulmonary bypass. In parallel were improvements in care of the trauma patient including prehospital care, patient transport, and concepts of volume resuscitation, as well as the development of anesthesia and critical care specialties. These all led to the improved outcome of those sustaining cardiac injuries [20, 21].
Techniques
Diagnosis
Initial Evaluation
Cardiac injury occurs in 6.4 % of cases of penetrating thoracic trauma [22]. Those involving the “cardiac box” (an imaginary area inferior to the clavicles, superior to the costal margins, and medial to the midclavicular lines) (Fig. 10.1) are the most worrisome [23]. However, wounds that occur outside “the box” can also result in cardiac injury [24, 25], and the increased mortality with such injuries is at least in part related to the clinician having a lower suspicion leading to delays in diagnosis [24].
Fig. 10.1
The cardiac box. Penetrating injuries within the borders inferior to the clavicles, superior to the costal margin, and between the midclavicular lines should increase the concern for cardiac injury. However, wounds that occur outside these borders do not exclude cardiac injury.
Patients who arrive at the trauma center after cardiac injury may present anywhere along the range from hemodynamically stable to cardiac arrest. Patients who manifest hemodynamic compromise may have exsanguinating hemorrhage, cardiac tamponade, or both. The classic findings of Beck’s triad (muffled heart sounds, hypotension, and jugular venous distension), caused by the rapid accumulation of a small amount of blood (30–50 ml) in the non-expansible fibrous pericardium, are rarely recognized in the resuscitation suite. Delayed recognition of hemopericardium will result in the development of tamponade physiology, decreased cardiac filling due to high intra-pericardial pressures, impaired cardiac output, hypotension, and death.
On presentation an evaluation that includes a brief history, identification of the location and possible trajectory of wounds, and an evaluation of the cardiopulmonary status of the patient must be completed rapidly. Resuscitative thoracotomy may be lifesaving for patients who present in extremis [1, 10, 20, 23, 26, 27]. As recommended by the Western Trauma Association, its use has expanded to include patients without signs of life with short prehospital times and a blunt mechanism and asystole if signs of tamponade are present or cannot be excluded (Table 10.1) [27, 28].
Table 10.1
Limits of resuscitative thoracotomy.
Limits of resuscitative thoracotomy |
|---|
Prehospital CPR >10 min after blunt trauma without responsea |
Prehospital CPR >15 min after penetrating trauma without responsea |
Asystole is presenting rhythm, and there is no pericardial tamponade |
FAST
The focused assessment with sonography for trauma (FAST) examination is extremely sensitive for detecting hemopericardium in precordial and penetrating transthoracic wounds, with sensitivity and specificity that approach 100 % [29–31]. It is especially useful in patients who present with maintained hemodynamics to assess the safety of subsequent diagnostic testing [30] and to determine the appropriate management in hemodynamically compromised patients with multiple wounds and potential for multi-cavitary hemorrhage. Penetrating precordial stab wounds with concurrent hemothorax require special consideration as the FAST examination has been shown to produce false-negative results due to cardiac injury decompressing into the left hemithorax [32]. In these cases, the liberal use of subxiphoid pericardial window is wise, as repeat ultrasonography and echocardiography may fail to diagnose underlying cardiac injury [32]. Occasionally, adequate windows will not be obtainable due to concomitant hemopneumothorax or subcutaneous emphysema.
CXR
A CXR is important to assist in missile trajectory, presence of concomitant thoracic injury, and operative planning. It can be obtained in most patients even when hemodynamically marginal. For those who need emergent operative intervention, a plate can be placed on the operating room table and a CXR obtained prior to incision [25].
Subxiphoid Pericardial Window
Subxiphoid pericardial window has been validated to be extremely accurate for overt and occult cardiac injuries [6]. It can be utilized to diagnose hemopericardium in patients with equivocal ultrasound results, when ultrasound windows are unobtainable, when ultrasound is unavailable, or when a precordial stab wound is associated with a left hemothorax [32]. It should be performed under general anesthesia in the operating room (OR) with the patient prepared and draped in an adequate fashion to proceed with sternotomy if necessary. When possible it is wise to have the patient adequately prepared and draped prior to the induction of anesthesia as patients with compensated tamponade may quickly deteriorate to cardiac arrest when preload is decreased from vasodilation and positive pressure ventilation [6]. An incision is made in the midline overlying the xiphoid, which should be excised to facilitate dissection and exposure [6]. The distal sternum is then elevated with a retractor. The diaphragm is identified and kept inferior, while blunt dissection is utilized to identify the pericardium. Meticulous hemostasis is necessary to prevent difficult-to-interpret results of the pericardial window. Once identified, the pericardium is grasped with Allis clamps and incised. If clot or blood is returned, immediate conversion to a sternotomy should occur.
Incisions
Median Sternotomy
Median sternotomy is most useful for stable patients who have proven cardiac injury or those that are at least marginally stable [20]. It provides excellent exposure to the mediastinum and can be extended for a laparotomy if indicated. It is our practice to explore most of these wounds via sternotomy even with a concomitant lung injury, as both pleural spaces are accessible. Surgeons with less experience may find the incision limiting and should utilize anterolateral thoracotomy with extension as necessary.
Anterolateral Thoracotomy
Anterolateral thoracotomy is the incision of choice for patients arriving in extremis with severe hemodynamic compromise (Fig. 10.2) and may be extended to a right anterior “clamshell” thoracotomy (Fig. 10.3) when necessary. It is the most useful for ED thoracotomy [1, 4, 10, 20, 23, 26]. It is also useful in patients who deteriorate during laparotomy from a suspected cardiac injury and for those who are hemodynamically unstable from injuries that have traversed the mediastinum [20, 23]. Care must be taken to not perform the incision too inferiorly or optimum exposure may be limited and subsequent thoracic and sternal closure may be compromised [6]. Elevating the left hemithorax 20° by placing a roll under the left chest improves exposure [6] and should be considered in hemodynamically maintained patients and those with penetrating thoracic wounds who are undergoing laparotomy in case rapid entry into the chest is necessary.
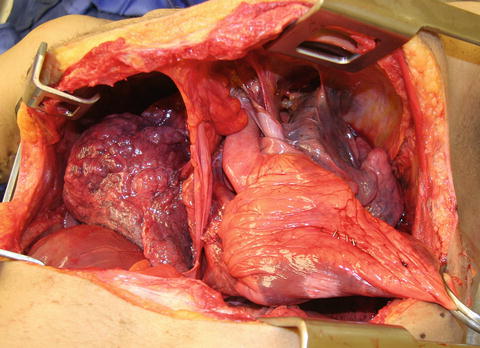
Fig. 10.2
Left anterolateral thoracotomy. The incision is made at the inframammary fold, carried into the fourth intercostal space, and curved toward the ipsilateral axilla. Positioning a rolled towel under the left hemithorax allows for additional extension of the incision and improved visualization of the posterior thoracic structures.
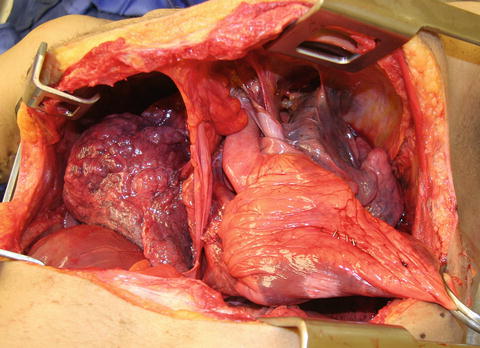
Fig. 10.3
Bilateral anterolateral “clamshell” thoracotomy. A left anterolateral thoracotomy can be extended across the sternum and into the fourth intercostals space on the right. This affords excellent exposure to the mediastinum and bilateral pleural spaces. Attention must be paid to proper incision placement, as incisions that are made too low may limit access to the upper mediastinum and great thoracic vessels (Facilities: Surgical Laboratory, Anatomical Services Division, School of Medicine, UMB. Cadavers and specimens: Anatomical Donor, Maryland State Anatomy Board).
When the clamshell thoracotomy is utilized, it is important to ligate the transected internal mammary arteries, after repairing the cardiac injuries [20]. In this situation, the arteries will often be in vasospasm and thus easy to overlook. The surgeon who omits this step will have the opportunity to return to the operating room to correct their mistake should the patient survive the subsequent hemorrhage.
Exposure and Immediate Control
Pericardiotomy is the first step in evaluation of the injured heart. In the presence of tamponade, the pericardium can be tense and difficult to grasp. Uncontrolled opening can result in injury to the underlying cardiac structures. The use of Allis clamps to grasp the pericardium helps. Initially, it is wise to make a 1–2 cm incision. The pericardium is further incised with Metzenbaum scissors [20, 23]. When approached from an anterolateral thoracotomy, the phrenic nerve is identified and the pericardium is widely opened anterior and longitudinal to it. The incision can be extended medially at the pericardial base if further exposure is needed. The pericardium is opened in the midline when a sternotomy incision is utilized and may be teed off at its inferior aspect for better exposure, again avoiding the phrenic nerve. In the stable patient, taking the time to suture the pericardium to the skin to create a cardiac sling facilitates visualization and repair [6].
Once the pericardium is opened, the surgeon should rapidly assess for location and degree of cardiac injury, paying special attention to wounding patterns that suggest multiple, posterior, septal, or valvular injuries. Involvement of the thoracic great vessels is also important to identify. The American Association for the Surgery of Trauma (AAST) Organ Injury Scale (OIS) [35] (Table 10.2) can be utilized to classify injury and has been validated to predict mortality [1, 10, 20] but offers little benefit for intraoperative decision-making.
Table 10.2
American association for the surgery of trauma organ injury scale: heart injury.
AAST-OIS: heart injury scale | |
|---|---|
Grade | Description of injury |
I | Blunt cardiac injury with minor ECG abnormality (nonspecific ST or T wave changes, premature atrial or ventricular contraction, or persistent sinus tachycardia) |
Blunt or penetrating pericardial wound without cardiac injury, cardiac tamponade, or cardiac herniation | |
II | Blunt cardiac injury with heart block (right or left bundle branch, left anterior fascicular, or atrioventricular) or ischemic changes (ST depression or T wave inversion) without cardiac failure |
Penetrating tangential myocardial wound up to, but not extending through, the endocardium, without tamponade | |
III | Blunt cardiac injury with sustained (≥6 beats/min) or multifocal ventricular contractions |
Blunt or penetrating cardiac injury with septal rupture, pulmonary or tricuspid valvular incompetence, papillary muscle dysfunction, or distal coronary arterial occlusion without cardiac failure | |
Blunt pericardial laceration with cardiac herniation | |
Blunt cardiac injury with cardiac failure | |
IV | Penetrating tangential myocardial wound up to, but not extending through, the endocardium, with tamponade |
Blunt or penetrating cardiac injury with septal rupture, pulmonary or tricuspid valvular incompetence, papillary muscle dysfunction, or distal coronary arterial occlusion producing cardiac failure

Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |





