Cardiac Arrhythmias: Introduction
Patients with cardiac arrhythmias often present to the emergency department. The patient’s clinical presentation determines the urgency with which the assessment and management should proceed. Patients with serious signs and symptoms (ie, shock, hypotension, congestive heart failure (CHF), severe shortness of breath, altered level of consciousness, ischemic chest pain, or acute myocardial infarction) require immediate treatment. With stable patients, more time is afforded for review of the 12-lead electrocardiogram (ECG) and rhythm strip to diagnose the cardiac arrhythmia. Review of available prior ECGs may also assist in arrhythmia diagnosis.
Eleven Helpful Hints for Emergency Department Arrhythmias
Obtain as much information as available. Always look at all 12 leads and be sure of name, date, age, correct lead placement, and standardization.
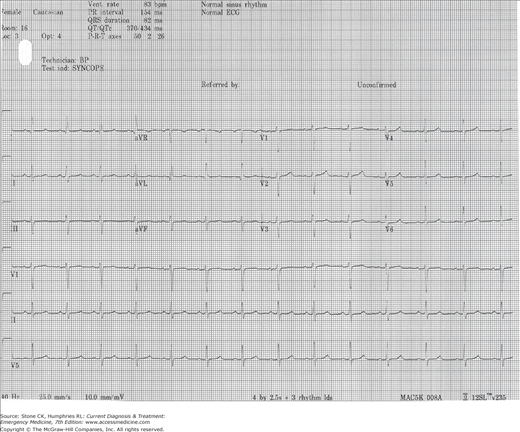
Know what each lead looks like normally (Figure 35–1); eg, lead I (and usually lead II and aVF) should look like the textbook PQRST except no Q wave. In lead I, the P, QRS, and T should all be upright, the intervals should be normal and the PR and ST baselines should be isoelectric.
A regular tachycardia with a rate close to 150 should prompt a search for atrial flutter.
Precise diagnosis of wide complex tachycardias (WCTs) can be difficult. If ventricular rate is irregular consider atrial fibrillation (AF) or atrial flutter with variable conduction and underlying bundle branch block (BBB).
Do not rely on computer readings. They may or may not be correct.
Single-lead rhythm strips may not have enough information. If time permits, always obtain a 12-lead ECG.
You cannot have too many ECGs. Serial ECGs are important. Sinus tachycardia rates tend to change over time.
Arrhythmias are common in acute ST elevation myocardial infarctions.
Tachyarrhythmias are divided into narrow or wide QRS width and then into regular or irregular.
Arrhythmia classifications and terminologies can be confusing and they change as new information becomes available.
If the heart rhythm is slow and the patient is hypotensive with signs of poor perfusion, assume transthoracic or transvenous pacing will be needed.
No consensus exists on correct pad positioning and current ACLS guidelines endorse both the conventional or sternal apical positioning (one pad on the superior–anterior right chest just below the level of the clavicle and one pad on the inferolateral left chest) and the anteroposterior (the anterior pad as in the conventional method and the posterior pad on the right or left upper back). However, some authors feel that anteroposterior placement with the anterior pad over the right atrium and the posterior pad at the tip of the left scapula optimizes cardioversion of atrial tachyarrhythmias while placement of the anterior pad over the ventricles and posterior pad again at the tip of the left scapula works well for ventricular arrhythmias.
All currently manufactured defibrillators use biphasic waveforms so unless you are using an older machine, the energy setting will range from 0 Joules (J) to 200 J. All energy doses mentioned in this chapter will be for biphasic defibrillators. In addition to disease-specific energy recommendations, there are device-specific recommendations for the different biphasic defibrillator models for first shock energy dose in some situations. Notably, in ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) the initial shock is 120 for devices using a rectilinear waveform and 150–200 J for devices using a truncated exponential waveform ranging from 120 to 200 J. ACLS guidelines recommend that IF THE OPERATOR IS UNSURE of device-specific recommendations then the defibrillator’s highest energy level should be used in this setting; this will be 200 J for all biphasic units and 360 J if you happen to still have a monophasic unit. The bottom line is that if you are uncertain on the energy dose in any emergent situation where electricity is required for an adult your best bet is turn the energy up as high as it will go as even maximal doses of energy are felt to be relatively safe.
Tachyarrhythmias
Immediate synchronized cardioversion should be performed on all unstable patients with tachydsrythmias. The specific arrhythmia diagnosis (supraventricular or ventricular) does not need to be made immediately because initial management is the same. Patients with polymorphic ventricular tachycardia (PMVT) of 30 seconds or more and all unstable patients should be treated with immediate defibrillation.
In stable patients, the initial medical management will be guided by the underlying rhythm and a detailed history and physical examination. In recent years, the more traditional approach to categorize patients as either stable or unstable has been modified. Hemodynamically stable patients can be further subdivided into those with preserved or impaired cardiac function. Findings of impaired cardiac function in a patient who is otherwise stable may alter the pharmacologic treatment.
(See Appendix, Figure 35–3.) Sinus tachycardia occurs when the sinus rate is faster than 100 beats/min. Usually the rate is 101–160 beats/min. Young, healthy adults can accelerate their heart rate up to 180–200 beats/min, particularly during exercise. Young children have been noted to have sinus rates up to 220 beats/min. Sinus tachycardia should not be viewed as a primary arrhythmia but more as a response to an underlying illness or condition. It is often normal in infancy and early childhood but can occur as a result of a number of conditions including pain, fever, stress, hyperadrenergic states, anemia, hypovolemia, hypoxia, myocardial ischemia, pulmonary edema, shock, and hyperthyroidism. Certain medications and illicit drugs can also cause tachycardia. The P wave in sinus tachycardia should have a positive axis in the frontal plane, ie, the P wave should be positive in lead I and aVF.
The treatment of sinus tachycardia is directed at the underlying cause. This may include correction of dehydration with intravenous fluids, analgesic or antipyretic administration, or supplemental oxygen to correct hypoxia. Treatment aimed at correcting the heart rate rather than the underlying condition may be harmful if the tachycardia is compensatory and is supporting the cardiac output. Gradual slowing of the heart rate with treatment of the underlying condition or during carotid sinus massage may help to differentiate sinus tachycardia from other supraventricular arrhythmias. Adenosine administration with a 12-lead rhythm strip is helpful in differentiating from other causes of tachyarrhythmias. Further management, including the need for hospitalization, depends on the underlying condition.
(See Appendix, Figures 35–6, 35–7, 35–8, 35–9, 35–10, and 35–11.) Paroxysmal supraventricular tachycardia (PSVT) is a general term that refers to a number of tachyarrhythmias that arise from above the bifurcation of the His bundle. Approximately 90% of these arrhythmias occur as a result of a reentrant mechanism; the remaining 10% occur as a result of increased automaticity.
Atrioventricular nodal reentrant tachycardia (AVNRT) is the most common form of PSVT, accounting for 50–60% of cases. The heart rate is usually 180–200 beats/min and is characterized by sudden onset and sudden termination. Because the reentrant mechanism occurs within the AV node itself, virtually simultaneous excitation of the atria and ventricles occurs. As a result, the P waves occur concurrent with the QRS complexes and are difficult to visualize on the ECG. Often, patients with AVNRT do not have underlying heart disease. Common precipitating factors include alcohol, caffeine, and sympathomimetic amines. Patients with AVNRT usually present in their third or fourth decade of life, and the majority (approximately 70%) are female.
Atrioventricular reciprocating tachycardia (AVRT) accounts for 30% of PSVT. In most cases, the impulse travels down the AV node and follows a retrograde path up the accessory bypass tract. Because activation of the ventricles occurs through normal conduction pathways, the accessory pathway is concealed, and the QRS morphology is normal. Consider AVRT if the heart rate is faster than 200 beats/min or if P waves are seen following the QRS complex.
Sinus node reentry and intraatrial reentry are uncommon causes of PSVT, accounting for approximately 5% of cases. In these arrhythmias, the heart rate is usually 130–140 beats/min. More often, patients with these arrhythmias have underlying heart disease.
Automatic atrial tachycardia is another uncommon arrhythmia, accounting for less than 5% of cases of PSVT. The heart rate is usually 160–250 beats/min but may be as slow as 140 beats/min. In this case, the underlying mechanism is increased automaticity rather than reentry. Automatic atrial tachycardia is commonly associated with underlying heart disease. This arrhythmia is difficult to treat and may be refractory to standard measures including cardioversion.
PSVT can be classified as AV nodal dependent or independent. This strategy may prove useful in formulating treatment options. AVNRT and AVRT are AV nodal dependent, meaning that the AV node is involved in the reentrant circuit. For these rhythms, pharmacologic management is designed to decrease conduction through the AV node.
Patients with PSVT who are hemodynamically unstable require immediate synchronized DC cardioversion. Current recommendations are to start with low-energy levels (50–100 J) and then to increase the initial dose by 50 J as needed until sinus rhythm is restored. If clinical circumstances permit, administer intravenous sedatives. Avoid the common error of delaying emergency cardioversion to perform other patient care activities. If immediate cardioversion is unavailable, physical maneuvers that cause vagal stimulation can be attempted.
Adenosine, β-blocker, or calcium channel blocker may be administered.
Tachycardia associated with PSVT is usually well tolerated unless the patient has underlying heart disease or left ventricular dysfunction.
In stable patients, physical maneuvers causing vagal stimulation can be attempted prior to medication administration. Maneuvers that stimulate the vagus nerve such as the Valsalva maneuver (expiration against a closed glottis), Mueller maneuver (deep inspiration against a closed glottis), cold water facial immersion, and carotid sinus massage are at times effective in terminating PSVT that results from AV nodal and sinoatrial (SA) nodal dependent mechanisms. Perform carotid sinus massage only after auscultation for carotid bruits.
If vagal stimulation is contraindicated or ineffective, adenosine is considered first-line medical therapy for conversion of PSVT. In general, pharmacologic agents with AV nodal blocking properties such as adenosine, β-blockers, calcium channel blockers, and digoxin are used for the acute management and prevention of AV nodal dependent PSVT. Other antiarrhythmic agents, such as procainamide and amiodarone, which exert effects at various levels of the cardiac conduction system are used for the management and prevention of AV nodal independent PSVT. Antiarrhythmic medications may be considered for conversion of PSVT when AV nodal blocking agents are unsuccessful.
Adenosine is an endogenous nucleoside that slows conduction through the AV node and is successful in terminating more than 90% of PSVTs resulting from AV nodal reentry mechanisms (AVNRT and AVRT). Adenosine may also be effective in terminating sinus node reentry tachycardia but is usually ineffective in terminating automatic atrial tachycardia. Often adenosine will cause a transient AV block, briefly exposing the underlying atrial activity. Administration of a medication with more prolonged effect on the AV node (β-blockers or calcium channel blockers) may provide a more sustained reduction in ventricular rate.
Administer adenosine rapidly, and follow each dose immediately with a 20-cc saline flush. Although current recommendations are to administer an initial intravenous dose of 6 mg over 1–3 seconds repeated at 2 and 4 minutes with 12-mg doses if this does not terminate the PSVT, many clinicians choose to forgo the initial 6-mg dose and will increase the dose to 18-mg if the 12-mg dose does not produce AV blockade. The 18-mg dose has been shown to be both safe and effective. Common side effects include unexplainable feeling of impending doom, facial flushing, hyperventilation, dyspnea, and chest pain. These side effects are often transient owing to the short half-life of adenosine (less than 5 seconds). Prewarning to the patient of these symptoms is helpful. The effects of adenosine are antagonized by caffeine and theophylline and potentiated by dipyridamole and carbamazepine. Heart transplant patients may be overly sensitive to the effects of adenosine; if necessary, use smaller doses. Because adenosine can provoke bronchospasm, use caution if it is being administered to patients with a history of reactive airway disease.
Adenosine can also be administered to a stable patient with a wide QRS complex tachycardia suspected to be supraventricular in origin. Adenosine is preferred over calcium channel blockers in patients with hypotension or impaired cardiac function and in patients concomitantly receiving β-adrenergic blocking agents.
β-blockers such as metoprolol or esmolol slow SA node impulse formation and slow conduction through the AV node. These medications should be used with caution in patients with a history of severe reactive airway disease and CHF.
Metoprolol is an alternative to calcium channel blockers, and is administered intravenously at a dose of 5 mg every 5 minutes for three doses. Esmolol is an ultrashort-acting β1-selective β-blocker that has the advantage of a brief half-life (∼10 minutes) and a rapid onset of action. Administer a loading dose of 0.5 mg/kg over 1 minute. This is followed by a maintenance infusion of 50 μg/kg/min. If the response is inadequate, another dose of 0.5 mg/kg can be administered after 4 minutes and the maintenance infusion increased to 100 μg/kg/min. When heart rate control is achieved, reduce the maintenance infusion to 25 μg/kg/min.
Calcium channel blockers such as diltiazem or verapamil are effective in converting PSVT to sinus rhythm. The efficacy of diltiazem and verapamil in terms of conversion rates, rapidity of response, and safety profile appear similar. These medications decrease SA and AV node conduction and cause prolongation of the AV node refractory period. Calcium channel blockers also decrease myocardial contractility and peripheral vascular resistance. Use calcium channel blockers with caution in patients with left ventricular dysfunction or CHF. Avoid these medications in patients with WCT of unknown origin, ventricular tachycardia (VT), or tachycardia with ventricular preexcitation. Hypotension is the most concerning side effect of intravenous administration and occurs in 10–15% of patients.
The initial dose of verapamil is 5–10 mg administered intravenously over 1–2 minutes. Additional doses of 5–10 mg can be administered every 15 minutes as needed until the desired effect is achieved or a total of 30 mg has been administered.
The initial dose of diltiazem is 0.25 mg/kg administered intravenously over 2 minutes (20 mg for the average adult). If necessary, a dose of 0.35 mg/kg can be administered in 15 minutes. After conversion, a maintenance infusion can be started at 5–10 mg/h and can be increased to a maximum of 15 mg/h if needed.
The choice between β-blockers and calcium channel blockers depends on multiple factors, but both should not be given intravenously to the same patient. Both have rapid onset (minutes) and both should be used with caution in severe COPD and severe CHF. Medication that the patient is currently taking and physician preference are considerations. In patients with hyperthyroidism and congenital heart disease, β-blockers are the best choice.
Digoxin administration will increase vagal tone while reducing sympathetic activity. As a result, conduction through the AV node is slowed. Digoxin may be administered as an intravenous bolus dose of 0.5 mg. Additional doses of 0.25 mg may be given as needed every 4–6 hours, with a total dose not to exceed 1.25 mg in 24 hours. The immediate benefit of digoxin is lessened by its slow onset of action. When used in combination, digoxin may allow for lower doses of subsequently administered antiarrhythmic agents. Avoid digoxin in patients with AF with ventricular preexcitation.
Amiodarone is a class III antiarrhythmic agent with sodium- and potassium-channel blocking properties and β-blocking and calcium channel blocking properties. By virtue of its β-blocking and calcium channel blocking properties, amiodarone slows conduction through the AV node. In patients with impaired cardiac function or CHF, treatment options narrow. Amiodarone has a solid safety profile and may be an effective alternative agent in this situation. Amiodarone can be administered as a slow intravenous infusion of 150 mg over 10 minutes. This is followed by a maintenance infusion of 1 mg/min for 6 hours and then 0.5 mg/min. Additional bolus doses of 150 mg can be repeated as needed for resistant or recurrent PSVT up to a total daily dose of 2 g.
Procainamide is a class IA antiarrhythmic agent with sodium channel blocking properties. Procainamide will slow conduction through both the AV node and, if present, an accessory bypass tract. Procainamide can be considered for patients with PSVT refractory to AV nodal blocking agents. The recommended loading dose of procainamide is 17 mg/kg administered as a slow intravenous infusion at a rate of 20–30 mg/min (1 g for an average adult). Stop the initial infusion if the arrhythmia is suppressed, hypotension develops, or the QRS complex widens by more than 50% of its original duration. After arrhythmia suppression, start a maintenance infusion at 1–4 mg/min.
Hospitalization should be considered for patients in PSVT with accompanying serious signs and symptoms, patients requiring emergency cardioversion, patients in PSVT with ventricular preexcitation, and patients with arrhythmias refractory to standard treatment. Outpatient follow-up care should be provided for the otherwise healthy patient with a transient episode of PSVT converted to sinus rhythm in the emergency department.
(See Appendix, Figures 35–12 and 35–13.) In AF, the atrial rate is disorganized and is 300–600 beats/min. AF is characterized by an irregularly irregular ventricular rate with the absence of discernible P waves.
AF is the most common sustained cardiac arrhythmia in adults. It is estimated that AF affects more than 2 million persons in the United States; its prevalence increases with age, approaching 10% in those older than 80 years. AF can occur in the absence of underlying heart disease or may be associated with a number of conditions, including chronic hypertension, valvular disease, cardiomyopathy, myocardial ischemia, myocarditis, pericarditis, or congenital heart disease. AF may also occur in the presence of other systemic disorders, including hyperthyroidism, pulmonary embolism, hypoxia, and excess consumption of alcohol or caffeine.
Patients with nonvalvular AF have approximately a 5% annual incidence of stroke as a result of a thromboembolic event. This risk increases fourfold in patients with mitral stenosis and increases dramatically in older patients, approaching 30% in patients aged 80–89 years.
Acute management of AF includes ventricular rate control and prevention of thromboembolic complications. Additional management considerations include restoration and maintenance of sinus rhythm.
Patients in AF with a rapid ventricular response who are hemodynamically unstable require immediate synchronized DC cardioversion. Recommendations are to start between 100 and 200 J biphasic and then to increase the dose in stepwise fashion as needed until sinus rhythm is restored.
In stable patients with a rapid ventricular response, the initial goal is rate control. This can usually be achieved with β-blockers, calcium channel blockers, or digoxin. β-blockers may prove most helpful in patients with hyperthyroidism but are relatively contraindicated in patients with acute decompensated CHF. Diltiazem and verapamil can often slow the ventricular rate and have the added benefit of antianginal effects and blood pressure control in hypertensive patients. In more than 90% of patients, a reduction in heart rate of at least 20% is noted. Diltiazem appears to be safe for use in patients with mild CHF. Digoxin can also help control the ventricular rate in patients with AF and may be useful in patients with left ventricular dysfunction. Its slower onset of action as compared to other agents makes it less useful for acute rate control. In patients with mild to moderate CHF, the administration of amiodarone may prove useful. Intravenous amiodarone can also be considered an alternative agent for rate control when the above agents fail. The specific medication choice will often be dictated by the urgency of the situation, the medication profile, physician preference, and the patient’s underlying condition.
Prophylactic anticoagulation with warfarin has been shown to significantly reduce the incidence of stroke in patients with AF. If new-onset AF is of undetermined duration or greater than 48 hours duration, initiation of anticoagulation is necessary. Current recommendations include anticoagulation for 3 weeks, followed by elective cardioversion and then continued outpatient anticoagulation for four more weeks. An alternative strategy is initial anticoagulation with unfractionated or low-molecular-weight heparin followed by transesophageal echocardiography to evaluate the left atrial appendage for the presence of clot. If no clot is identified, the patient may safely undergo cardioversion, followed by anticoagulation for 4 weeks. If a left atrial appendage clot is identified by transesophageal echocardiography, recommendations include anticoagulation for 3 weeks, followed by cardioversion and then continued anticoagulation for four additional weeks. In patients with AF of less than 48 hours duration, anticoagulation is not recommended.
Various antiarrhythmic agents, including amiodarone, procainamide, and sotalol (class III), are used to chemically convert AF. Pharmacologic or electrical cardioversion may be considered in selected stable emergency department patients with AF of less than 48 hours duration. Remodeling, both anatomically and electrically, occurs soon after the onset of AF. Postponing cardioversion could lead to an increased resistance to attempts at conversion.
Patients with chronic rate-controlled AF do not require hospital admission. In patients with new-onset AF, hospitalization is often required for ventricular rate control, initiation of anticoagulation, and sometimes for initiation of antiarrhythmic therapy. If a patient presents with thromboembolic complications, hospital admission will also be necessary.
(See Appendix, Figure 35–14) In atrial flutter, the atrial rate is usually 250–350 beats/min. It is the most common underdiagnosed tachyarrhythmia. Sawtooth flutter waves may sometimes be seen on ECG, but should not be relied upon. Typically, atrial flutter will present with 2:1 AV conduction. For this reason, it is important to consider atrial flutter in the differential diagnosis of a regular tachycardia at approximately 150 beats/min, even in the absence of flutter waves. Atrial flutter is most commonly identified as negative waves in II, III, and aVF with positive flutter waves in lead V1.
If atrial flutter is suspected, several options are available to better identify atrial activity. Vagal maneuvers or administration of adenosine with a 12-lead rhythm strip may unmask flutter waves.
Acute management of atrial flutter includes ventricular rate control and prevention of thromboembolic complications. Additional management considerations include restoration and maintenance of sinus rhythm.
Patients in atrial flutter with a rapid ventricular response who are hemodynamically unstable require immediate synchronized DC cardioversion. Current recommendations are to start with between 50 and 100 J biphasic and then increase the energy dose in stepwise fashion as needed until sinus rhythm is restored.
In stable patients with a rapid ventricular response, the initial goal is rate control. Adequate heart rate control can be achieved with the administration of either β-blockers or calcium channel blockers. Digoxin is often less effective acutely because of its slow onset of action. Amiodarone and diltiazem are alternatives for rate control in the stable patient with impaired cardiac function or CHF.
The stroke risk for patients in atrial flutter is less than that of AF. The same anticoagulation guidelines exist for atrial flutter as in AF.
Patients with chronic rate-controlled atrial flutter do not require hospital admission. In patients with new-onset atrial flutter, hospitalization is often required for ventricular rate control, initiation of anticoagulation, and sometimes for initiation of antiarrhythmic therapy.
(See Appendix, Figure 35–15) In multifocal atrial tachycardia (MAT) the heart rate is typically 100–130 beats/min. The characteristic ECG finding is at least three different P wave morphologies. The rhythm often appears irregular and can at times be confused with AF. Varying PR intervals may also be noted. When the rate is slower than 100 beats/min, the term wandering atrial pacemaker is applied. Unless underlying aberrant conduction is present, the QRS complexes are narrow. Severe underlying chronic obstructive pulmonary disease accounts for approximately 60–85% of cases. Theophylline and digoxin levels should be checked since toxicity of these drugs can cause MAT.
The initial treatment of MAT is directed at correcting the underlying cause. As with AF, the initial goal of therapy is to achieve heart rate control. Because MAT does not respond to electrical cardioversion, pharmacologic intervention may be required.
Magnesium may be effective in converting MAT and can be administered as a 2 g intravenous bolus over 1 minute. This is followed by a 2 g/h infusion for 5 hours. Magnesium can still be effective if serum magnesium levels are in the normal range. Potassium repletion may be helpful in patients who are hypokalemic.
Amiodarone, digoxin, or diltiazem may be considered as alternative agents for rate control, especially when the patient exhibits findings of CHF.
Patients may require hospitalization for MAT if the heart rate is difficult to control or for further management of the underlying condition.
(See Appendix, Figures 35–11 and 35–13) Patients with Wolff-Parkinson-White (WPW) syndrome have an accessory pathway. Anatomical location varies and the pathways can be AV (Kent), atrio-His (James), intranodal, and nodoventricular (Mahain). On the ECG, a short PR interval (less than 120 ms) and the presence of a δ wave (initial upward slurring of the QRS complex) signify ventricular preexcitation.
A variety of arrhythmias may occur in patients with WPW syndrome; approximately 70% is orthodromic AVRT. In this case, the cardiac impulse travels down the AV node (antegrade conduction) and stimulates the ventricles through the normal conduction pathways. The accessory AV bypass tract serves as the retrograde limb of the circuit. In the absence of aberrant ventricular conduction or a fixed BBB, the morphology of the QRS complex is narrow without evidence of ventricular preexcitation (absent δ wave). The bypass pathway is considered concealed if the short PR and δ wave are not present on the baseline ECG.
Rarely, antidromic AVRT occurs whereby the accessory AV pathway acts as the antegrade limb of the circuit and the AV node as the retrograde limb. Antidromic AVRT will produce a wide QRS complex tachycardia and may masquerade as VT. The tachycardia may be extremely rapid (with ventricular rate 220–300), leading to ventricular fibrillation (VF) as a result of an R-on-T phenomenon.
AF is the second most common arrhythmia associated with WPW syndrome. AF with ventricular preexcitation has a high potential to precipitate hemodynamic compromise. AF with a rapid ventricular rate is characterized by an irregular tachycardia and a wide QRS complex resulting from ventricular preexcitation.
Patients with orthodromic AVRT who are hemodynamically unstable require immediate synchronized DC cardioversion. Current recommendations are to start between 50 J and 100 J biphasic and then to increase the initial dose in stepwise fashion as needed until sinus rhythm is restored. In patients with known WPW syndrome presenting with a narrow complex regular tachycardia, orthodromic AVRT can be assumed. In stable patients, the medical treatment will be the same as in AVNRT. Pharmacologic treatment with adenosine, β-adrenergic blocking agents, or calcium channel blockers can be administered as deemed necessary and appropriate for the individual case. In general, the treatment of orthodromic AVRT with AV nodal blocking agents is safe. The risk of enhancing antegrade conduction down the bypass tract is very low.
Treatment of AF with ventricular preexcitation (antidromic AVRT) is different from that of orthodromic AVRT. If the patient is hemodynamically unstable, immediate synchronized DC cardioversion starting at 100–200 J is warranted. The use of AV nodal blocking agents, specifically β-blockers, calcium channel blockers, and digoxin, is contraindicated. If conduction through the AV node is slowed, conduction down the accessory pathway may be enhanced, possibly degenerating to VF. Because procainamide will slow conduction through both the AV node and the accessory pathway, it is the medication of choice when AF with a rapid ventricular response is associated with ventricular preexcitation. Procainamide is also the medication of choice in antidromic AVRT. Amiodarone can be used as an alternative agent in treating AF with ventricular preexcitation and findings of CHF.
Hospitalization is not required for patients who are asymptomatic with evidence of ventricular preexcitation on the ECG (sinus rhythm, short PR, and a δ wave). Consider hospitalizing patients who have serious signs and symptoms or those requiring cardioversion. In addition, hospitalization is recommended for patients with AF and ventricular preexcitation or antidromic AVRT. Patients who present with stable orthodromic AVRT may be discharged with close outpatient follow-up after pharmacologic conversion in the emergency department.
Ventricular Arrhythmias
(See Appendix, Figures 35–16 and 35–17) Ventricular tachycardia is the most common cause of wide QRS complex tachycardia. The term VT is used when six or more consecutive ventricular beats occur. The ventricular rate is usually 150–220 beats/min, although rates slower than 120 beats/min may occur. Nonsustained VT is characterized by an episode lasting less than 30 seconds. Sustained VT is characterized by an episode lasting longer than 30 seconds, associated with hemodynamic compromise, or requiring therapeutic intervention for termination. WCT refers to a regular tachycardia with a QRS complex greater than 0.12 seconds (120 ms) in duration. WCT most often occurs as a result of either VT or SVT with aberrant conduction (underlying or rate-dependent BBB).
In more than 75% of patients presenting in the emergency department with regular WCT, the underlying arrhythmia is VT. The presence of structural heart disease, coronary artery disease, prior myocardial infarction, or CHF strongly suggests VT. Certain ECG findings favor VT over SVT with aberrant conduction. These findings include a QRS complex wider than 160 ms, the presence of fusion beats, and evidence of AV dissociation. AV dissociation occurs in about 20% of patients with VT and confirms the diagnosis (this is usually seen with ventricular rates less than 150). A common clinical error that must be avoided is to assume that WCT is SVT with aberrant conduction. All cases of WCT of unknown origin should be managed as VT.
Electrical storm is a somewhat rare but well described entity that consists of recurrent ventricular tahchycardia, usually with an implanted defrillator that discharges repeatedly. Patients with this condition have a high mortality and will likely need sedation as well as sympathetic blockade to control the recurrent dysrhythmias. Anti-arrhythmics use is usually required and IV amiodarone is the drug of choice.
A WCT is most likely VT.
Consider toxicity—always think of hyperkalemia, tricyclic antidepressants, and digoxin. Treatment is different and cardioversion is not helpful.
If unstable, treat immediately with cardioversion.
Ask two questions: Prior MI? Tachycardia new since MI? Answering yes increases likelihood of VT to >90%.
Twelve-lead ECG is always best, if possible, before, during, and after treatment. Save all tracings.
Old ECGs are invaluable when looking for similar BBB patterns.
There are many algorithms for determining VT (vs SVT with BBB, aberrancy) and none are 100% accurate. The rules are difficult to remember and interpret. VT is likely if the following are identified:
RS absent in all precordial leads (seen in less than 25% of VT). If cannot find RS (only QS, QR, monophasic R, or rSR complexes) this favors VT.

Full access? Get Clinical Tree