CHAPTER 101
Bursitis
Presentation
Following minimal trauma or repetitive motion, a nonarticular synovial sac or bursa protecting a tendon or prominent bone becomes swollen, possibly fluctuant, and possibly painful and inflamed. It may be nontender or tender. The elbow, hip, knee, and shoulder are most commonly involved unilaterally.
Olecranon bursitis can be caused by trauma from a direct blow (often only causing acute hemorrhage into the bursa), chronic crushing friction from prolonged leaning on the elbows, crystal deposition (gout), systemic diseases (rheumatoid arthritis, diabetes, systemic lupus erythematosus [SLE], alcoholism, uremia), or infection (usually from an overlying skin lesion or wound).
Trochanteric bursitis causes pain and tenderness that is greatest over the area of the greater trochanter of the hip. Active resistance to abduction of the hip may increase the pain.
Ischial bursitis can result from trauma or prolonged sitting on a hard surface. This causes buttock pain that may radiate down the back of the thigh. Palpation will reveal point tenderness over the ischial tuberosity.
Prepatellar bursitis, also known as “housemaid’s knee,” is caused by frequent or prolonged kneeling on hard surfaces. There may be marked swelling and tenderness over the anterior surface of the patella.
Pes anserine bursitis is located on the medial inferior aspect of the knee at the inferior margin of the medial collateral ligament about 4 to 5 cm below the joint margin and just superior to the pes anserinus tendon. Inflammation of this bursa is common in overweight patients and those beginning an exercise program. The knee pain is worsened when climbing stairs, and there is tenderness to direct palpation over the area of the bursa.
Subdeltoid (or subacromial) bursitis can be the result of traumatic injury or chronic overuse, and it frequently accompanies other shoulder problems. A history of pain in the lateral shoulder, which can be severe with acute onset, and tenderness to palpation along the acromial border help make the diagnosis.
Because there is no joint involved, there is usually little decreased range of motion, except in the shoulder, where bursitis can produce dramatic limitation. If the tendon sheath is involved, there may be some stiffness and pain with motion. Swelling is less evident when the bursa is deep, such as in the case of ischial bursitis.
What To Do:
 Obtain a detailed history of the injury or precipitating activity, document a thorough physical examination, and rule out a joint effusion (see Chapter 120).
Obtain a detailed history of the injury or precipitating activity, document a thorough physical examination, and rule out a joint effusion (see Chapter 120).
 Obtain a radiograph or ultrasound study if the possibility of a foreign body exists.
Obtain a radiograph or ultrasound study if the possibility of a foreign body exists.
 Primarily pertaining to olecranon and prepatellar bursitis, swelling and fluctuance suggest an effusion in the bursa, and cellulitis-like erythema, fever, warmth, and tenderness with an overlying skin lesion suggest infection. Prepare the skin with alcohol and povidone-iodine antiseptic solution, and either anesthetize the skin with 1% lidocaine using a 30-gauge needle or spray with ethyl chloride. Puncture the swollen bursa with an 18- or 20-gauge needle using aseptic technique, withdraw some fluid to drain the effusion, and have the fluid analyzed to rule out a bacterial infection. A tangential approach to the olecranon bursa can be performed by keeping the barrel of your 10-mL syringe parallel to the ulna over the forearm while puncturing the bursa (Figure 101-1). The elbow can be held in extension or up to 90 degrees of flexion.
Primarily pertaining to olecranon and prepatellar bursitis, swelling and fluctuance suggest an effusion in the bursa, and cellulitis-like erythema, fever, warmth, and tenderness with an overlying skin lesion suggest infection. Prepare the skin with alcohol and povidone-iodine antiseptic solution, and either anesthetize the skin with 1% lidocaine using a 30-gauge needle or spray with ethyl chloride. Puncture the swollen bursa with an 18- or 20-gauge needle using aseptic technique, withdraw some fluid to drain the effusion, and have the fluid analyzed to rule out a bacterial infection. A tangential approach to the olecranon bursa can be performed by keeping the barrel of your 10-mL syringe parallel to the ulna over the forearm while puncturing the bursa (Figure 101-1). The elbow can be held in extension or up to 90 degrees of flexion.
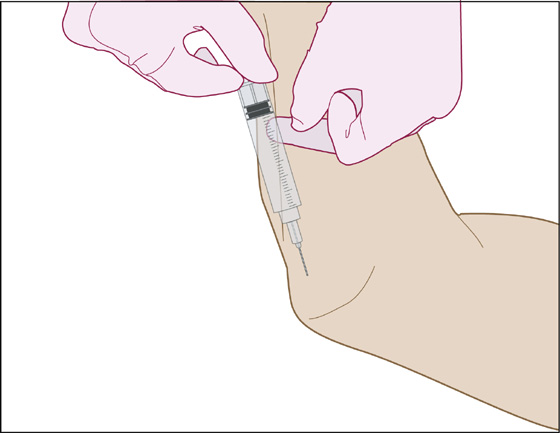
Figure 101-1 Technique for draining olecranon bursitis.
 A tangential approach to the prepatellar bursa can be obtained by keeping the barrel of your syringe parallel to the long axis of the tibia.
A tangential approach to the prepatellar bursa can be obtained by keeping the barrel of your syringe parallel to the long axis of the tibia.
 Relatively clear yellow or serosanguineous fluid drained from a minimally inflamed bursa needs to be sent only for culture, because clear fluid indicates nonseptic bursitis. Using a hemostat to grasp the needle hub to twist off and remove the syringe, the needle can be left within the bursa for later instillation of a corticosteroid. When the fluid appears purulent or cloudy, or if the clinical picture is unclear, the needle can be removed. This fluid should be sent for leukocyte count, Gram stain, culture, and sensitivity; it should also be analyzed for crystals when there is suspicion of gout.
Relatively clear yellow or serosanguineous fluid drained from a minimally inflamed bursa needs to be sent only for culture, because clear fluid indicates nonseptic bursitis. Using a hemostat to grasp the needle hub to twist off and remove the syringe, the needle can be left within the bursa for later instillation of a corticosteroid. When the fluid appears purulent or cloudy, or if the clinical picture is unclear, the needle can be removed. This fluid should be sent for leukocyte count, Gram stain, culture, and sensitivity; it should also be analyzed for crystals when there is suspicion of gout.
 Examine a Gram stain of the effusion. This may be negative in about 30% of patients with septic bursitis. Leukocyte counts greater than 2000/mm3 have a high sensitivity and specificity for bursal infections. The white blood cell (WBC) count for the nonseptic bursitis will usually be only a few hundred/mm3 With or without fluid to examine, it is often difficult to clinically distinguish an inflamed bursa from an infected one. Therefore, if there is any suggestion or sign of a bacterial infection, hold any steroids and prescribe appropriate oral antibiotics. Bacterial infections tend to be gram-positive cocci, specifically Staphylococcus aureus, and respond well to dicloxacillin (Dynapen), 500 mg qid for 2 to 3 weeks. Alternatively, prescribe drugs that are active against community-acquired, methicillin-resistant S. aureus (CAMRSA), such as trimethoprim-sulfamethoxazole (TMP/SMX) (Bactrim DS), sulfamethoxazole 800 mg, trimethoprim 160 mg bid × 14 days; doxycycline 100 mg bid × 14 days; clindamycin (Cleocin), 300 mg qid × 14 days; or, in the most worrisome cases, linezolid (Zyvox), 600 mg bid for 2 to 3 weeks (extremely expensive).
Examine a Gram stain of the effusion. This may be negative in about 30% of patients with septic bursitis. Leukocyte counts greater than 2000/mm3 have a high sensitivity and specificity for bursal infections. The white blood cell (WBC) count for the nonseptic bursitis will usually be only a few hundred/mm3 With or without fluid to examine, it is often difficult to clinically distinguish an inflamed bursa from an infected one. Therefore, if there is any suggestion or sign of a bacterial infection, hold any steroids and prescribe appropriate oral antibiotics. Bacterial infections tend to be gram-positive cocci, specifically Staphylococcus aureus, and respond well to dicloxacillin (Dynapen), 500 mg qid for 2 to 3 weeks. Alternatively, prescribe drugs that are active against community-acquired, methicillin-resistant S. aureus (CAMRSA), such as trimethoprim-sulfamethoxazole (TMP/SMX) (Bactrim DS), sulfamethoxazole 800 mg, trimethoprim 160 mg bid × 14 days; doxycycline 100 mg bid × 14 days; clindamycin (Cleocin), 300 mg qid × 14 days; or, in the most worrisome cases, linezolid (Zyvox), 600 mg bid for 2 to 3 weeks (extremely expensive).
 Initially, reaspirate any recurrent infected effusion on a daily basis.
Initially, reaspirate any recurrent infected effusion on a daily basis.
 When there is no indication of a bacterial infection, inflammatory bursitis may respond to injection of local anesthetics such as lidocaine (Xylocaine) 1% or bupivacaine (Marcaine), 5 to 9 mL, mixed with corticosteroids, such as methylprednisolone (Depo-Medrol) 0.25%, 40 mg, or betamethasone (Celestone Soluspan), 1 mL. Use the 18- or 20-gauge aspiration needle that you left in place. Alternatively, use a 25-gauge, 1¼-inch needle and review the anatomy so that the needle can be carefully pushed through the lowest density tissue and the shortest pathway, causing the least amount of pain while probing for the bursa sac. For olecranon bursitis, perform the injection with the arm in extension, and penetrate the sac parallel to the ulna on the lateral side, away from the ulnar nerve. Approach the greater trochanteric bursae from the lateral and posterior side. For the subacromial bursa, insert the needle just inferior to the posterolateral edge of the acromion and then direct the needle toward the opposite nipple. The anesthetic and steroid should flow freely into the space without any resistance or significant discomfort to the patient. After injection, it may take several minutes or longer for patients to perceive pain relief and regain lost range of motion. The literature suggests that the instillation of a long-acting cortisone solution is associated with a significantly better cure rate than aspiration or nonsteroidal anti-inflammatory drugs (NSAIDs) alone or in combination.
When there is no indication of a bacterial infection, inflammatory bursitis may respond to injection of local anesthetics such as lidocaine (Xylocaine) 1% or bupivacaine (Marcaine), 5 to 9 mL, mixed with corticosteroids, such as methylprednisolone (Depo-Medrol) 0.25%, 40 mg, or betamethasone (Celestone Soluspan), 1 mL. Use the 18- or 20-gauge aspiration needle that you left in place. Alternatively, use a 25-gauge, 1¼-inch needle and review the anatomy so that the needle can be carefully pushed through the lowest density tissue and the shortest pathway, causing the least amount of pain while probing for the bursa sac. For olecranon bursitis, perform the injection with the arm in extension, and penetrate the sac parallel to the ulna on the lateral side, away from the ulnar nerve. Approach the greater trochanteric bursae from the lateral and posterior side. For the subacromial bursa, insert the needle just inferior to the posterolateral edge of the acromion and then direct the needle toward the opposite nipple. The anesthetic and steroid should flow freely into the space without any resistance or significant discomfort to the patient. After injection, it may take several minutes or longer for patients to perceive pain relief and regain lost range of motion. The literature suggests that the instillation of a long-acting cortisone solution is associated with a significantly better cure rate than aspiration or nonsteroidal anti-inflammatory drugs (NSAIDs) alone or in combination.
 For knee and elbow, apply a bulky compressive dressing for protection and comfort. Construct a splint, and instruct the patient in rest, elevation, and ice packing. A sling should suffice for the shoulder.
For knee and elbow, apply a bulky compressive dressing for protection and comfort. Construct a splint, and instruct the patient in rest, elevation, and ice packing. A sling should suffice for the shoulder.
 Prescribe NSAIDs if tolerated, and arrange for follow-up. When a long-acting cortisone solution has been used, NSAIDs can be avoided.
Prescribe NSAIDs if tolerated, and arrange for follow-up. When a long-acting cortisone solution has been used, NSAIDs can be avoided.
 Fluid may reaccumulate and require additional aspiration.
Fluid may reaccumulate and require additional aspiration.
 When symptoms have subsided, prior to returning to any previous activity, have the patient add appropriate padding to prevent further bursal irritation.
When symptoms have subsided, prior to returning to any previous activity, have the patient add appropriate padding to prevent further bursal irritation.
 Septic bursitis resolves slowly and may take weeks to get better. Two to 3 weeks of antibiotics are required, and close follow-up is mandatory.
Septic bursitis resolves slowly and may take weeks to get better. Two to 3 weeks of antibiotics are required, and close follow-up is mandatory.
What Not To Do:
 Do not inject corticosteroids into an infected bursa. The infection is likely to worsen and spread.
Do not inject corticosteroids into an infected bursa. The infection is likely to worsen and spread.
 Do not puncture an area of olecranon bursitis by needling perpendicular to the ulna. Flexion and trauma may produce a chronic sinus.
Do not puncture an area of olecranon bursitis by needling perpendicular to the ulna. Flexion and trauma may produce a chronic sinus.
 Do not routinely obtain radiographs when there is minimal trauma involved. They are generally not helpful or necessary in acute bursitis.
Do not routinely obtain radiographs when there is minimal trauma involved. They are generally not helpful or necessary in acute bursitis.
Discussion
Common sites for bursitis include the subacromial bursa of the shoulder, the prepatellar bursa of the knee, the olecranon bursa of the elbow, and the trochanteric bursa of the hip. In shoulder bursitis, radiographs may reveal calcific bursitis. There may be bony spurs in olecranon bursitis, but these images are not needed for routine emergency therapy.
Burning pain and sometimes numbness in the anterolateral thigh, which may be worsened by prolonged standing or walking, may be caused by compression of the lateral femoral cutaneous nerve in the area of the anterior superior iliac spine (meralgia paresthetica). Obese, pregnant, or diabetic patients or workers who carry a heavy tool belt are commonly affected. Tightly fitting garments may also precipitate the syndrome. There is no tenderness over the greater trochanter of the hip, and this should not be confused with bursitis. Meralgia paresthetica usually resolves after conservative treatment, such as weight loss and the wearing of loose-fitting clothes.
Patients with septic bursitis, unlike those with septic arthritis, can often be safely discharged on oral antibiotics, because the risk for permanent damage is much less when there is no joint involvement. Severe cases with extensive cellulitis or lymphangitis, however, may require hospitalization and IV antibiotics. Immunocompromised patients may require longer courses of antibiotics. Grossly purulent fluid that reaccumulates must be repeatedly reaspirated on a daily basis.
Some long-acting corticosteroid preparations can produce rebound bursitis several hours after injection, after the local anesthetic wears off but before the corticosteroid crystals dissolve. Patients should be so informed. Patients should prevent recurrence by wearing knee or elbow pads at work, avoiding pressure and trauma to vulnerable areas, and caring for skin wounds near bursae.

Full access? Get Clinical Tree


