Burns/Inhalation Injury
James H. Holmes IV
I. Introduction
Epidemiology
Approximately 45,000 people in the United States require hospitalization each year for burn injuries, with10% suffering a concomitant inhalation injury.
Overall mortality rate is 4%, with the LD50 (50% lethal dose) occurring at 70% total body surface area (TBSA).
Most burn deaths occur in residential fires and nearly half are smoking-related or due to substance abuse.
Suspect abuse and report when seeing a patient with unusual burns like a child (e.g., immersion burns, odd shape/distribution, recurrent injuries, etc.), or when the history and injury do not match (see Chapter 21).
Approximately 5% of burn patients have concomitant non-thermal injuries.
Transfer to burn center
American Burn Association (ABA) criteria for transfer to a dedicated burn center:
Partial-thickness burns >10% TBSA
Burns involving the face, ears, hands, feet, genitalia, perineum, or major joints
Full-thickness burns of any size
Electrical burns or injuries, including lightning
Chemical burns
Inhalation injury
Burns in patients with preexisting medical conditions
Burns associated with concomitant non-thermal trauma in which the burn injury poses the greatest risk of morbidity or mortality
Burned children in hospitals without qualified personnel
Burns in patients requiring special social, emotional, or long-term rehabilitation interventions
II. Prehospital
History
Time of injury (start time for calculating fluid resuscitation)
Open or closed space (inhalation injury is more likely in closed space)
Source of burn: Flame, liquid, steam, chemical, explosion, electrical
Duration of exposure
Mechanism of any associated injury: Motor vehicle crash (MVC), fall, etc.
Quantity of prehospital fluid
Care at scene
Safely remove patient from source of injury.
Extinguish flames and remove clothing.
Burn patients are trauma patients and receive full evaluation until proven otherwise.
Assess for immediate life-threatening injuries, as per advanced trauma life support (ATLS) and advanced burn life support (ABLS).
Provide supplemental oxygen and airway protection.
Apply dry dressings.
Maintain normothermia.
Initiate transport to hospital.
III. Initial Assessment and Resuscitation
General
Burn injury can be dramatic and distract the resuscitation team from concomitant non-thermal injuries.
Patients with severe burn injury may appear deceptively stable on arrival. A patient may be talking on admission with stable blood pressure and mild tachycardia. Within 24 hours, the patient is frequently critically ill.
Provide early pain control with frequent small doses of intravenous (IV) opiates.
Elevate the ambient room temperature to avoid heat loss from the burn wound.
Burns are tetanus-prone and mandate prophylaxis.
Airway
Note: Although urgent endotracheal intubation is sometimes necessary, time usually exists to assess the airway and provide a semi-elective intubation, when necessary.
Provide supplemental oxygen to all patients.
Criteria for intubation are the same as in all trauma patients. The following clinical conditions may require immediate or early intubation in a burn patient:
Apnea, respiratory failure, or profound hypoxia.
Patients with severe facial burns may appear initially stable. Consider semi-elective intubation because profound orofacial swelling over the next few hours can make intubation very difficult.
Signs and symptoms of inhalation injury:
Injuries sustained in a closed-space fire
Carbon deposits in the naso/oropharynx
Expectorated, carbonaceous sputum
Wheezing
Hoarseness
Stridor
PaO2: FiO2 <300
Upper airway injury and obstruction frequently occur in patients with burns of the face and neck. Soft-tissue swelling of the face, oropharynx, glottis, and trachea can be dramatic, precluding safe intubation and making cricothyroidotomy/tracheostomy difficult. Any patient with phonation changes or stridor should be considered for immediate intubation.
Breathing
If intubated, deliver 100% oxygen (generally with 5 to 10 cm H2O of positive end-expiratory pressure [PEEP]) with a goal to avoid high airway pressures while maintaining patient comfort. Perform arterial blood gasses (ABGs) to ensure adequate oxygenation, ventilation, and clearance of acidosis.
Perform a chest radiograph to look for associated trauma, early signs of inhalation injury, and position of tubes/lines.
Bronchoscopy may be necessary to assess inhalation injury.
Circumferential torso burns causing elevated airway pressures may require escharotomy. Note: Patients without complete circumferential torso burns may also require escharotomy to provide adequate ventilation at lower airway pressures.
Circulation
Intravenous access is ideally obtained with large-bore (14 to 16 gauge in adults) peripheral catheters placed through unburned tissue. In severe burns (>30% TBSA), it is optimal to obtain central venous access early before massive swelling and edema occur. Placement through burned tissue is acceptable, if it is the only option.
Initial fluid resuscitation
Typically, only burns ≥20% TBSA in adults require formal IV fluid resuscitation.
Start with and use only Lactated Ringer’s (LR). Do not use normal saline (NS), as profound hypernatremia and hyperchloremia may result when a large burn resuscitation is completely done with NS.
The Parkland/Baxter formula (4 mL LR/kg body weight/% TBSA burn) is used to guide initial resuscitation.
How to use the Parkland/Baxter formula:
The formula is only a guide for fluid requirements in the first 24 hours following injury. Fluid resuscitation should be adjusted based on the patient’s physiologic response to treatment, notably urine output and blood pressure.
Only partial- and full-thickness burns (aka second and third degree) are included in the TBSA estimation.
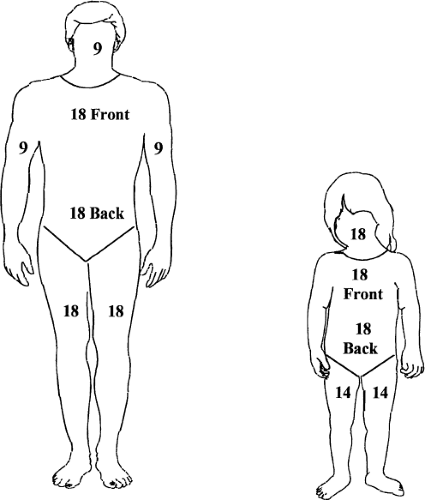
TBSA is determined by the rule of nines (Fig. 33-1) or age-appropriate burn diagrams.
Give one-half of the calculated requirement in the first 8 hours from the time of injury. The second half is given over the subsequent 16 hours.
The first 8 hours begin at the time of burn, not at the time the patient is first seen.
For example, a 35% TBSA burn in a 70 kg person gets 9,800 mL LR over 24 hours, 4,900 mL over the first 8 hours (613 mL/hour), and 4,900 over subsequent 16 hours (306 mL/hour).
Once started, use urine output to guide the fluid rate to obtain 30 to 50 mL/hour in an adult.
In the second 24 hours post-burn, a patient’s maintenance fluid requirements are ∼1.5 to 2 times normal maintenance fluid volumes. This volume should be given as crystalloid, with the composition of the fluid determined by serum electrolyte levels. Any colloid supplementation (i.e., albumin) should occur >24 hours post-burn.
A subset of patients (inhalation injury, high-voltage electrical, delayed resuscitation, massive deep burns) may require additional fluid over that estimated by the Parkland/Baxter formula. Hemoconcentration (i.e., hematocrit >55%) may be an early clue to increased fluid requirements.
Any patient who does not respond with adequate urine output during the first few hours of resuscitation, is elderly, or has a history of cardiopulmonary/renal disease may require a more formal goal-directed resuscitation, guided by any of the various means of invasive hemodynamic monitoring.
Pediatric fluid resuscitation (infants and toddlers <20 kg)
The head and neck represent larger proportions of calculated TBSA than in adults (Fig. 33-1 and Table 33-1).
Careful fluid resuscitation is necessary to avoid:
Pulmonary edema from excessive fluid administration
Cerebral edema associated with hyponatremia
Formula for estimated fluid = dextrose-based maintenance + 3 mL/kg/% TBSA LR over 24 hours
Table 33-1 General Body Differences: Children Versus Adults
Factor
Difference
Size and shape
- Less fat and connective tissue available for protection.
- Energy is transferred and dispersed over a smaller body surface area.
- Internal organs are in relatively close proximity, which predisposes to multiple organ injuries.
- Solid organs are larger compared with the rest of the abdomen.
- Rib cage is higher, affording less protection to abdominal organs.
- The infant’s head is disproportionately larger compared with the adult and subjected to a high incidence of shear injuries.
Skeleton
- Incomplete ossification of bones causes them to be more pliable and thus less likely to fracture. As a result, pulmonary contusions and splenic lacerations often occur without rib fractures.
- A different array of partial fractures (e.g., greenstick, torus, and buckle fractures).
- Injuries to the growth plates during the various stages of childhood development result in a specific pattern of fractures.
Surface area
- Large surface-area-to-weight ratio results in a greater predisposition to heat loss (three times greater) and hypothermia.
Psychological development
- Children often regress to a previous developmental stage during stressful and anxiety-provoking situations.
Long-term effects of injury
- Splenectomy in children places them at lifelong risk for overwhelming postsplenectomy infection (OPSI).
Maintenance volume is pro-rated over 24 hours.
One half of burn component in first 8 hours, and second half over ensuing 16 hours.
For example: A 3-year-old male weighing 20 kg with a 35% TBSA burn would require 2,100 cc LR and 1,500 cc D51/2NS with 40 mEq KCl/L over the first 24 hours following injury. The LR would be administered at 130 cc/hr for the first 8 hours and then at 65 cc/hr for the subsequent 16 hours, while the D51/2NS would run continuously at 60 cc/hr.
- Less fat and connective tissue available for protection.
Goal is a well-perfused child with a urine output of 1.0 to 1.5 mL/kg/hour.
IV. Initial Wound Assessment and Management
Assessment
The TBSA of any burn is best estimated by age-appropriate diagrams. The rule of nines (Fig. 33-1) provides an initial approximation of burn size in adults. Further, for all individuals, the palmar surface of the entire hand (palm + digits) represents 1% TBSA and may be helpful in estimating the size of smaller burns.
Terminology for burn depth using “degree” has been replaced by the description of “thickness.” Classification of depth at the time of admission is an estimate and may be inaccurate because severe burns tend to progress or evolve over the 12 to 72 hours following injury.
Burn depth (Fig. 33-2)
Superficial (first degree, such as sunburn)
Confined to epidermis with minimal tissue damage.
Full access? Get Clinical Tree