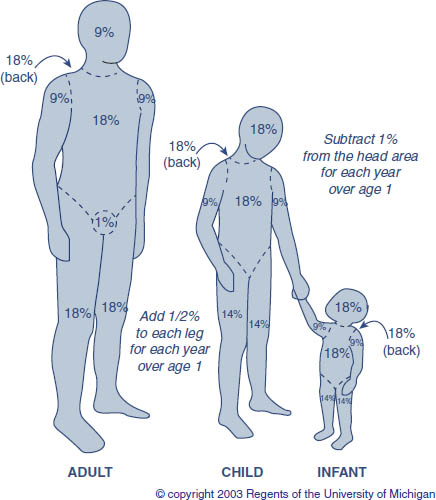
Chapter 23 This chapter is an overview of the assessment and management of adult burn patients. The focus is on thermally injured patients with special considerations for chemical, cold injury and electrical burns. The management principles in the first 48 hours after burn injury until the patient can be transferred to a specialized burn care facility are highlighted. Burn care involves a multidisciplinary team of specialists and allied health professionals to manage both the medical and psychological impact of the injury. The initial management of the burn patient follows the Advanced Trauma Life Support Course as outlined by the American College of Surgeons. The American Burn Association has also designed its own Advanced Burn Support Life Course and specific differences in the two protocols will be outlined in this section. Airway management of a burn patient is important for transport as well as the long-term management. The endotracheal tube needs to be of large bore to protect from the massive fluid shifts and edema that occur in the early burn period. Intubation for burns greater than 20% body surface area is prophylactic recognizing that the process of swelling and possibly large volumes of fluid will be required in the first 72 hours. Securing the airway with facial burns might require intraoral fixation to dentition or bone if dentition is absent. High flow oxygen (FiO2 100%) should be initiated for every patient and especially if carbon monoxide (CO) poisoning is suspected. Ventilation may be restricted with low tidal volumes and high airway pressures in the setting of inhalation injury and/or circumferential thorax and abdominal wounds. Escharotomies may be required to correct this abnormality. Systemic and peripheral circulation is monitored. Peripheral IV access is preferentially obtained through non-burned tissue. In massive burn injury indwelling catheters through burned tissue are sometimes required. Burned extremities should be evaluated by Doppler examination if pulses cannot be palpated. Circumferential burns, especially full thickness injuries, will impair blood flow to the limbs by acting as a tourniquet. Escharotomies may be required to restore perfusion. Central access with multi-lumen catheters is required to manage the number and types of resuscitation fluids and medications, these patients require. Ringer’s lactate fluid should be started and titrated to treat the degree of burn shock. The burn patient may initially be awake and alert. If there is altered level of consciousness then consider CO poisoning, head injury, substance abuse, hypoxia or pre-existing medical conditions. Finally, the patient should be kept warm to avoid hypothermia. All clothing and jewelry should be removed and the patient covered with dry warming blankets. Intravenous and irrigation solutions should be warmed. A thorough history, physical, and determining the etiology of the burn are important. Etiology is divided into flame, scald, electrical, chemical and contact burns. The environment where the patient was injured will give clues to further injuries or the degree of injury. If the patient was found in an enclosed space (e.g., house fire) then inhalation injury should be suspected. A patient in a MVA requiring extrication could be a multi-trauma patient with life threatening fractures, head injury or intra-abdominal injuries. The same is also true if there was an explosion or a “no-let-go” phenomenon from an electrical injury as the patient may have fallen from a height or been thrown away from the high-tension current. The “when, what, where, how, and who” details surrounding first aid should be determined. In all cases of thermal injury the history and the pattern of the burn seen must fit. If there is a discrepancy then noting this on the history can be very helpful much later on in cases of suspected neglect, abuse or even homicide (rare). A patient post electrical burn requiring cardiopulmonary resuscitation at the scene may have heart conduction defects requiring monitoring. A chemical burn may not be decontaminated adequately if first aid has not been applied appropriately. The burning process can continue and cause extension of the injury. The history should include Tetanus status. A complete head to toe examination of the patient is important to determine the burn depth, burn size and other associated injuries that may have been missed in the primary survey. Posterior surfaces require inspection and are often missed with health care providers not familiar with thermal injury. The Rule of Nine’s determines the burn severity for adults and the Lund Browder for pediatrics, see Fig. 1.1 The Rule of Nine’s gives each anatomic region a designation of 9%. For example, the chest as part of the anterior torso is 9% and in combination with the abdomen is 18%. In children, the head surface area represents a larger component of the total body surface area (TBSA). After the age of 12 months, 1% is taken off the head surface area for each year of age. A quick and practical method for determination of burn extent is to use the hand surface area (palm plus the fingers equals one percent of the body surface area) of the patient to represent the body surface area burned. This is particularly helpful in irregular or scattered surface area burns. All health care personnel involved with the resuscitation of the patient should take universal precautions. All patients requiring intubation should have a bronchoscopy performed as part of the initial workup. Not only will this provide quick evidence of proper ETT tube placement but also will add to the possible diagnosis of smoke inhalation injury grade and subsequent fluid requirements. Directed intravenous fluid resuscitation should occur for all patients with greater than 15–20% TBSA or larger. The Parkland Formula (4 mL/kg/%TBSA) should be calculated and utilized to guide resuscitative measures. TBSA calculations should utilize only partial thickness and full thickness injuries. The first half of the fluid volume is estimated to be given in the first 8 hours and the second half over the next 16 hours. The calculation is a guide and is modified to account for time from the burn and fluids that have already been received. Ringer’s lactate is the crystalloid solution of choice for resuscitation. Urine output is monitored hourly with a goal output of 0.5–1cc/kg/hour. Fig. 1. TBSA calculation. Under resuscitation could lead to renal failure and secondary effects of hypotension but over resuscitation can lead to extremity or abdominal compartment syndrome and cardiac failure. Extremity perfusion should be monitored hourly especially in patients with circumferential burns that are deep partial thickness or full thickness to determine the need for escharotomies. A high clinical suspicion for compartment syndrome should be maintained. Intra-abdominal pressure (IAP) by bladder transduction should be measured every 4 hours in high volume resuscitations. Wound irrigation with copious amounts of warm water or saline is important but should not delay transfer to a health care facility. In the absence of sufficient water for cooling, patients should be promptly covered with warm dry towels or sheets to limit air currents circulating over the tissue causing pain and hypothermia. The treatment of chemical and electrical burns will be discussed in a separate section. A gastric tube should be inserted for burns greater than 20% BSA to start early enteral feeding to meet the increased metabolic demands and prevent gastric dilatation in the patient. Laboratory investigations include CBC, electrolytes, BUN, CR, ABG, carboxyhemoglobin, glucose, ECG, and appropriate imaging. The patient should be continuously monitored and prepared for transfer to a specialized burn center. The American Burn Association recommends that all patients with the following criteria should be transferred to a Burn Center (Table 1) (http://www.ameriburn.org/BurnCenterReferralCriteria.pdf) Table 1. ABA burn center referral criteria. 1.Partial thickness burns greater than 10% TBSA. 2.Burns that involve the face, hands, feet, genitalia, perineum and major joints. 3.Third degree burns (full thickness) of any age group. 4.Electrical burns including lightening injury. 5.Chemical burns. 6.Inhalation injury. 7.Burn injury in patients with pre-existing medical disorders that could complicate management, prolong recovery, or affect mortality. 8.Any patient with burns and concomitant trauma (fractures) in which the burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, then the patient may be initially stabilized in a trauma center before transfer to a burn unit. Physician judgment is necessary in such situations and should be in concert with the regional medical control plan and triage protocols. 9.Burned children in hospitals without qualified personnel or equipment for the care of children. 10.Burn injury in patients who will require special social, emotional, or rehabilitative intervention. Three major processes can affect oxygenation in a burn patient: CO poisoning, direct thermal injury to the airway above the glottis and an inhalation injury. Indications for intubation include the following factors: • Smoke inhalation • Large burns >20% TBSA • Deep facial or neck burns • Closed range explosion • Steam Inhalation • Respiratory distress, oxygenation failure or ventilation failure CO Poisoning should be suspected in patients with decreased level of consciousness who were found in an enclosed space. CO impairs tissue oxygenation by preferentially binding to hemoglobin and displacing oxygen from the hemoglobin molecule. CO has an affinity for hemoglobin 240 times that of oxygen. CO also competitively inhibits the cells’ P450 cytochrome system and depresses cellular oxidative metabolism resulting in a shift towards anaerobic metabolism. This shifts the oxygen dissociation curve to the left resulting in a decreased unloading of bound oxygen at the tissue level. Physical signs of CO poisoning include headache, cherry red lips (50% of patients), arrhythmias and seizures. Levels of CO above 10% are clinically significant. Treatment for CO poisoning is humidified oxygen at 100% FiO2 by mask. The half-life of CO is 320 minutes on room air, and is reduced to 45 minutes on 100% O2. Direct thermal injury to the airway usually occurs above the level of the glottis. Direct injury is rare in the lower airway because of the heat dissipating capacity of the oro/hypopharynx and the reflex closure of the glottis. The exception is steam inhalation as it has 4,000 times the heat carrying capacity of air. Upper airway obstruction can occur rapidly in a burn patient with pharyngeal edema or a direct thermal injury. Intubation is important to protect the airway and ensure airway patency for transfer to a burn center. Inhalation injury is defined as a tracheobronchial mucosal injury secondary to inhaled toxins and particulate debris in smoke. These toxins include noxious chemicals such as aldehydes, sulfur oxides and phosphogens, which cause direct injury to the tracheobronchial mucosa. The presence of an inhalation injury is an independent risk factor for mortality in a burn patient. It has been shown to increase mortality by 30–40%.2 In the 4–12 hours after exposure, the tracheobronchial mucosa has increased capillary permeability resulting in transudation of fluid and protein into the lungs. The bronchial mucosa sloughs resulting in obstruction of the bronchi and alveoli. Severe bronchospasm ensues and mucous production increases. Inhalation injury should be considered if the flame burn occurred in a closed space, there was expectoration of carbonaceous sputum, greater than 10% carboxyhemoglobin, the patient was unconscious at the scene and with greater than 5 min of smoke exposure. On physical exam, singed nasal hairs, facial or oropharyngeal burns, hoarseness, decreased level of consciousness and signs of upper respiratory obstruction and distress are suggestive. A persistent metabolic acidosis despite what appears to be adequate fluid resuscitation is also suggestive of inhalation injury. Arterial blood gases may show a normal PaO2 and early chest x-rays are generally normal and non-predictive of the degree of smoke inhalation injury. The gold standard test for the diagnosis of inhalation injury is a fiber optic bronchoscopy. Physical findings to confirm the diagnosis include vocal cord edema, charring, mucosal sloughing, plugging from casts, and edema of the hypopharynx and upper tracheal mucosa. The inhalation injury should be evaluated and graded according to the scale designed by Endorf and Gamelli, see Table 2.3 Table 2. Grading of inhalation injury.
Burns, Cold Injury and Electrical Injury
Karen M. Cross and Joel S. Fish
Chapter Overview
Acute Burn Management
Primary survey
Secondary survey
History and physical exam
Treatment
Criteria for transfer to a burn unit and transport safety
Airway Management
Carbon Monoxide (CO)
Direct thermal injury
Inhalation injury
Grade O | No inhalation injury | Absence of carbonaceous deposits, erythema, edema or bronchorrhea or obstruction. |
Grade I | Mild Injury | Any or a combination of Minor or patchy areas of erythema, carbonaceous deposits in proximal and distal bronchi. |
Grade II | Moderate Injury | Any or a combination of Moderate degree of erythema, carbonaceous deposits, bronchorrhea with or without compromise of the bronchi. |
Grade III | Severe Injury | Any or a combination of Severe inflammation with friability, copious carbonaceous deposits, bronchorrhea, bronchial obstructions. |
Fluid Resuscitation and Edema Management
The goals of fluid resuscitation in a burn patient are to maintain tissue perfusion and organ function. In the early post burn period, hypovolemia is a result of decreased fluid in the intravascular space secondary to increased capillary permeability and an extravasation of protein and fluid into the interstitial space. Cardiac output is decreased secondary to myocardial depression and decreased pre-load. Hypotension and tachycardia are physical signs of burn shock that ensues.
The amount of edema formation post burn injury is dependent on the depth of burn injury, TBSA involvement, fluid resuscitation and the presence or absence of inhalation injury.4 Edema forms rapidly in a burn patient with peak edema at 12 hours post injury and resorption dependent on the above features. Fluid accumulation occurs in burned and non-burned tissue along with the organs.5 The accumulation of burn edema occurs in a biphasic pattern, as there is a rapid increase in interstitial fluid within the first hour post injury. Approximately 80% of total edema is present at 4 hours post injury. The second phase is marked by a gradual increase in fluid accumulation over the next 12–24 hours. Normally, fluid movement from the capillary to the interstitium is balanced by lymphatic clearance so that excess fluid does not accumulate. However, in burn injury the movement of fluid and protein into the extravascular space occurs rapidly and edema ensues.
The goals of resuscitation in a burn patient are to maintain tissue perfusion and organ function. Crystalloids (e.g., Ringer’s Lactate) are the fluids of choice as it is balanced, buffered and nearly isotonic with plasma. The major disadvantage of using Ringer’s Lactate alone is that one liter only achieves about 250cc of plasma volume and the rest ends up as interstitial fluid.
Immediate use of colloids for resuscitation is a controversial topic in the literature but there is evidence to suggest that colloids can decrease the crystalloid volume delivered, overall total fluid volume, and reduce the amount of edema formation. The institution of colloids might help prevent or minimize the devastating consequences of tissue edema. Colloid, 5% albumin, is generally given at 60–100ml/hour or 0.3–0.5ml/kg/%TBSA per hour. When used, colloid should be given within 8–12 hours post burn and in patients with > 50% TBSA or requiring more than 200mL/kg of resuscitation fluid. Albumin infusions can continue for 48 hours post burn injury. Serum albumin levels should be monitored beyond 48 hours and the albumin infusion titrated to these levels. Target serum albumin level is greater than 20g/L.
Hypertonic saline (3% TBSA) has been shown to have no survival advantage over crystalloid alone. The risk of hypernatremia is high and therefore this practice is not recommended for resuscitation.
Hexastarch and other starches are contra-indicated in burn resuscitation as the retained starch passes into the interstitium particularly the lung.
Resuscitation is monitored by systemic parameters such as urine output, blood pressure, and pulse and central venous pressure along with clinical examination of capillary refill, edema, and sensorium. Mean arterial pressure should be maintained above 60mmHg. Adult urine output should be maintained at 0.5 cc/kg/hour and children less than 30 kg at 1 cc/kg/hour. Base deficit can be utilized to determine the adequacy of resuscitation with levels less than 3 mmol/L considered adequate. Lactate is a measure of ischemia and levels should be maintained less than 2 mmol/L.
Over resuscitation results in excess edema accumulation, compromising local blood flow to tissue and organs. Patients with inhalation injuries, rhabdomyolysis, or large TBSA burns are at increased risk for large volume resuscitations (8 cc/kg/TBSA or 250 mL/kg). IAP monitoring is important in large volume resuscitation as fluid volume is directly proportional to IAP. IAP should be measured in high risk patients such as burn patients with circumferential burns to the torso, poor pulmonary compliance, BMI >30, prone position, associated trauma, and with a previous history of abdominal compartment syndrome. Intra-abdominal hypertension is defined as bladder pressures >12 mmHg (Normal 5–7 mmHg). Abdominal compartment syndrome is defined as elevation of IAP >20mmHg with new organ failure. New organ failure is defined but not limited to: Oliguria, mechanical ventilation or oxygenation failure (decrease in tidal volume and/or increase in airway pressures, hypoxemia), increased serum lactate, and hypotension. Abdominal compartment syndrome has a high mortality rate and should be treated aggressively. Sedation and paralysis of the patient, escharotomies of the chest and abdomen, close titration of IV fluids, and diuresis can improve end organ failure. If conservative strategies fail then an urgent decompressive laparotomy is performed.
The Parkland formula underestimates fluid resuscitation in children, electrical burns, inhalation injury, delayed resuscitation, alcoholics, and full thickness burns. Under resuscitation results in hypovolemia, ischemia to tissue and organs, shock, and multi-organ failure. Oliguria is one of the signs of under resuscitation; however, it is important to rule out other causes such as ACS or rhabdomyolysis. High voltage electrical injuries or patients with rhabdomyolysis are at increased risk of myoglobinuria. Myoglobin is directly cytotoxic to kidney tubules and cast formation occurs from epithelium sloughing in the distal convoluted tubule causing acute renal failure. Alkalinizing the urine with sodium bicarbonate (40 mEq/1L Ringer’s lactate) to keep the pH around 6.5 is helpful in solubilization of myoglobin crystals in the tubules. Fluids should be increased to keep urine output 1–1.5 cc/kg/hour. Diuresis with mannitol or furosemide may be used as an adjunct to alkalinization and fluids.
Burn Wound Management
General
Burn wounds are classified according to the depth of injury. This classification is used to determine the treatment required for each of the burn types. Burn types are divided into superficial (1st degree), partial thickness (2nd degree) and full thickness injuries (3rd degree). Clinically, superficial wounds are pink, with brisk capillary refill, and hair follicles remain attached to the dermis. They tend to be dry and painful. Healing time is less than 7 days.
Partial Thickness injuries are divided into superficial or deep injuries. Superficial partial thickness burns are pink, form blisters, have brisk capillary refill, and hair follicles remain attached. They tend to be moist and painful and can regenerate in less than 3 weeks. Deep partial thickness injuries are mottled, pink-white in color, with sluggish cap refill. These wounds are moist, hair follicles are not viable and they detach from the dermis with minimal pain. These wounds are unlikely to regenerate in less than 3 weeks if at all. Full thickness injuries are white in color, with no capillary refill, dry, and leathery. The hair follicles detach and there is no pain. Fourth degree burns involve full necrosis of the skin, muscle, tendon and bone.1
In 1953, Jackson described the zones of injury within the burn wound. He was the first to suggest that the burn wound is more than an anatomic determination of depth but represented physiologic zones that were dynamic and could change over time. The zone of coagulation is a central area of necrosis. The zone of hyperemia is an area of vasodilation and increased blood flow. Between these two zones exists the zone of stasis or “progression” zone. This is a dynamic region with a mixture of patent and occluded vessels along with viable and non-viable cells.6 Resuscitation efforts and antimicrobial dressings are designed to preserve the zone of stasis and prevent conversion to a zone of necrosis. If conversion occurs, then the zone of injury increases and adds to the TBSA that requires surgical excision and adds to patient mortality.
Wound management

Full access? Get Clinical Tree