Fig. 29.1
(a) Transducer position and corresponding sonogram for the interscalene approach to the brachial plexus. (b) Transducer position and corresponding sonogram for the supraclavicular approach to the brachial plexus. (c) The great vessels of the neck can be used as a readily identifiable sonoanatomical landmark by which the sternocleidomastoid and scalene muscles (and therefore the brachial plexus) can be located (The inset figure showed the position of the ultrasound probe and the direction of the needle insertion)
The ultrasound appearance of the plexus at the interscalene level can be described as multiple [3, 4] hypoechoic round or oval structures. The neural structures at the interscalene level have reduced connective tissue compared to the divisions; therefore, the targets for interscalene blockade are relatively hypoechoic. Proximal to the interscalene level, the roots of the brachial plexus can be identified adjacent to the transverse processes. The morphology of the cervical transverse processes determines cervical level and therefore the neural origins. The C6 transverse process has a prominent anterior tubercle, and the C7 transverse process has no anterior tubercle. Color Doppler is recommended to scan for vessels in the planned needle trajectory. The vertebral artery may be imaged close to the C7 transverse process deep to the scalene muscles. Other vessels imaged in the neck include the inferior thyroid, transverse cervical (and its descending dorsal scapular branch) and suprascapular arteries. The C5 transverse process has tubercles of even size producing a symmetrical “U” shape on the sonogram. The phrenic nerve can be imaged as a small hypoechoic structure anterior to the anterior scalene muscle only a few mm away from the brachial plexus [17].
Injection Technique: General Comments
For a single shot technique, sterile gloves should be worn and skin asepsis adhered to. For continuous catheter technique, we recommend a full aseptic technique and barrier precautions (gown, gloves, and facemask). Interscalene block is suitable for either in-plane or out-of-plane techniques. Standard strategies to improve in-plane needle imaging are important and particular vigilance must be taken to keep the needle tip in view.
Ultrasound-Guided Approaches
Single-Injection Techniques
The authors’ preferred needle trajectory is from lateral to medial (through the middle scalene muscle) using an in-plane technique (Fig. 29.1a). It is sometimes necessary to adopt a brief steep initial needle trajectory in order to pierce the prevertebral layer of the deep cervical fascia that overlies the middle scalene muscle. Once this “pop” has been felt, the needle should be flattened out and advanced toward the plexus. In the authors’ experience ultrasound guidance alone is adequate and nerve stimulator guidance is not usually required. The needle is advanced, and a second “pop” may be felt as the needle tip passes through the anterior border of the middle scalene muscle and the plexus. Incremental injection of 1–2 mL of local anesthetic can be used at this point to hydrodissect the plane between the muscles and plexus. Care should be taken to avoid local anesthetic being deposited inside the belly of the middle scalene muscle. Injection of local anesthetic on one side of the trunks at the C5–C7 level should be sufficient.
Continuous Catheter Techniques
The authors’ preferred needle trajectory is similar to single-injection techniques except the ultrasound transducer is rotated slightly and translated so that the needle entry point is positioned more cephalad and posterior taking the catheter skin entry point away from the surgical site. The needle trajectory now has a slight caudad angulation. Separating the needle skin entry point increases ease of needle visualization and also creates a tunnel for the catheter, reducing risk of dislodgement. Figure 29.2 demonstrates a patient positioned on their side for an interscalene catheter placement using a posterior in-plane approach. Figure 29.3a demonstrates the needle trajectory with needle at muscle–plexus interface and Fig. 29.3b the post-injection displacement of the middle scalene muscle. The sonogram in Fig. 29.3c shows the catheter following removal of needle. Note that the rotation of the probe may distort the image such that the trunks of the brachial plexus are less well demarcated and the sternocleidomastoid and middle scalene muscles appear elongated. The catheter tip position should be determined before commencing a local anesthetic infusion.
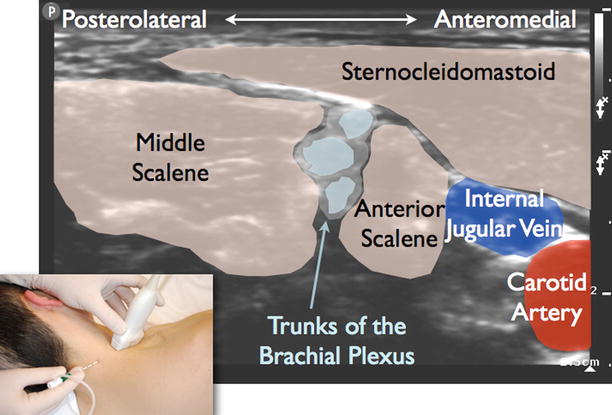
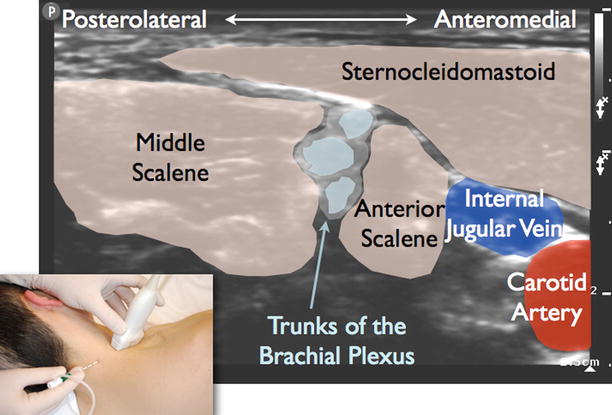
Fig. 29.2
When inserting a continuous interscalene catheter for shoulder surgery, it is desirable to maximize the distance between the needle insertion point and the surgical site (The inset figure showed the position of the ultrasound probe and the direction of the needle insertion)
Fig. 29.3
(a) Continuous interscalene catheter technique with needle tip located at the anterior border of the middle scalene muscle just posterior to the trunks of the brachial plexus. (b) Local anesthetic has been injected separating the trunks of the brachial plexus from the middle scalene muscle. (c) A catheter has been threaded beyond the brachial plexus and withdrawn and its position confirmed by injecting through the catheter confirming spread of injectate around the trunks of the plexus (The inset figures showed the ultrasound images corresponded to the stages of the procedure)
Local Anesthetic Dosage, Volume, and Spread
Dosage
The ED95 required to achieve postoperative analgesia for C7 interscalene brachial plexus anesthesia has been calculated to be 3.6 mL of ropivacaine 0.75 % [18]. In routine practice, 10–15 mL of local anesthetic such as ropivacaine 0.2–0.75 % is appropriate. The exact concentration will depend on patient factors, the purpose of the block (analgesia or anesthesia), and if a catheter technique is used. If a catheter is placed, the initial dose can be reduced and additional local anesthetic can be injected through the catheter. An infusion of ropivacaine 0.2 % 4–10 mL/h is used for postoperative analgesia.
Side Effects
Phrenic Nerve Block with Ipsilateral Hemidiaphragmatic Paralysis and Dyspnea
Phrenic nerve block occurs commonly following both interscalene and supraclavicular approaches to the brachial plexus. The proposed mechanism is that local anesthetic spreads across the anterior surface of the anterior scalene muscle and involves the phrenic nerve and/or there is cephalad spread toward C4. However, other mechanisms have been proposed including the existence of variations in the origin of the phrenic nerve from the brachial plexus itself [20, 21]. Usually phrenic nerve block is not of concern and management comprises patient reassurance. In patients with reduced pulmonary reserve, phrenic nerve block may be of concern; therefore strategies have been suggested to reduce the risk of phrenic nerve blockade. These strategies include dose reduction, using a more caudal target (C7), using ultrasound guidance, or avoiding interscalene block [22]. Following both interscalene and supraclavicular brachial plexus blockade, ultrasound guidance is associated with a reduced incidence of phrenic nerve paresis compared to nerve stimulator-guided techniques [23, 24].
Recurrent Laryngeal Nerve Block
This may present as hoarseness, occasionally stridor and a sensation of a lump in the throat. A case report has been published where it was thought that a deficient carotid sheath predisposed to recurrent laryngeal nerve block following continuous interscalene block [25].
Cervicothoracic Sympathetic Block
The cervicothoracic sympathetic trunk lies posterolaterally to the prevertebral fascia anterior to the longus colli muscle [26]. This is in close proximity to interscalene or supraclavicular brachial plexus block injection, hence involvement of the sympathetic trunk resulting in Horner’s syndrome.
Complications
Pneumothorax
Pneumothorax should be rare with ultrasound-guided interscalene block. Strategies have been suggested to reduce the risk of pneumothorax following ultrasound-guided supraclavicular blockade [27].
Contralateral Spread of Local Anesthetic (Epidural or Intrathecal)
Contralateral spread is a rare complication of interscalene brachial plexus blockade [28, 29]. There may be more than one mechanism responsible for contralateral spread including spread in the tissue planes deep to the prevertebral fascia [30]. The risk of contralateral spread may be increased with increased exposure to the total dosage of local anesthetic (initial bolus and subsequent boluses or infusion). This complication should be taken into account when utilizing these techniques especially in the ambulatory setting.
Catheter Misplacement
Catheter location can be confirmed with a test dose and potentially ultrasound guidance.
Cervical Spinal Cord Injury
The risks associated with performing a procedure close to the neuraxis are clear with interscalene blockade. Permanent neurological injury has been reported following injection of local anesthetic into the cervical spinal cord when an interscalene block was performed under general anesthesia [31].
Vascular Injection
Injection of local anesthetic into the vertebral artery or branches of the thyrocervical trunk can lead rapidly to local anesthetic toxicity.
Nerve Injury
Postoperative nerve injury regardless of etiology is of concern to patients and health-care providers. The reader should be aware that the methods used to capture, define, and report neurologic outcomes vary considerably. A single-center study reported the incidence of postoperative neurologic symptoms including those following interscalene block greater than 6 months duration was 0.9 per 1,000 blocks (95 % confidence interval, 0.5–1.7) [13]. Observational studies consistently report that postoperative neurologic dysfunction may be related to patient and surgical factors and that the incidence of serious permanent neuropathy directly related to peripheral regional anesthesia is rare. Neurologic complications include brachial plexopathy or injury to the dorsal scapular or long thoracic nerve. These nerves pass through or close to the middle scalene muscle and therefore ultrasound-guided interscalene block with a needle trajectory through this muscle, potentially introduces a new risk. Permanent phrenic nerve palsy is also a recognized although likely rare complication of interscalene brachial plexus block [32]. Distal mononeuropathies (involving the median and ulnar nerve) can occur following shoulder surgery and interscalene block, and these complications should be carefully evaluated taking into account all possible causes. Neurologic deficits in the C5–C6 distribution are more likely to be block related, compared to deficits in the ulnar distribution [9].
Documentation
The following documentation is recommended following interscalene blockade: (1) needle type, length, and gauge; (2) aseptic precautions, (3) anatomical, structures imaged; (4) monitoring techniques, verbal contact with a lightly sedated responsive patient, ultrasound guidance, nerve stimulation, injection pressure monitoring; (5) in-plane versus out-of-plane technique; (6) spread of local anesthetic; (7) local anesthetic dosage; and (8) complications.
Supraclavicular Block
Definition
Supraclavicular brachial plexus block involves injecting local anesthetic around the divisions of the brachial plexus deep to the prevertebral fascia posterolateral to the subclavian artery.
Background
Supraclavicular brachial plexus block was described in the early twentieth century by Kulenkampff and Persy [33] and was initially popular providing more effective anesthesia than other approaches to the brachial plexus. However, literature reviews and case series suggest an incidence of pneumothorax ranging from 0.5 to 6 % [34] and its popularity reduced [35]. Pneumothorax was the main deterrent to choosing this approach to the brachial plexus. More recently however, due to the popularity of ultrasound-guided regional anesthesia, with the potential to image the needle, brachial plexus, and pleura, the supraclavicular approach to the brachial plexus has increased in popularity as evidenced by case series [36], description of techniques [37], controlled clinical trials [38], and registries reports [11].
Anatomy
The anterior scalene muscle ends as a narrow tendon to insert on the scalene tubercle of the inner border of the first rib. Therefore, at this level, the anterior scalene muscle has a different morphology compared to at the interscalene level. In contrast, the middle scalene muscle inserts into a relatively larger area of the upper surface of the first rib (quadrangular area) and the muscle is relatively fleshy at the supraclavicular level. The prevertebral fascia over the brachial plexus at this level is well formed and distinct. The omohyoid muscle descends from the hyoid bone passes beneath the sternocleidomastoid over the carotid sheath to lie in the posterior triangle. The cylindrically shaped inferior belly of the omohyoid is often imaged and it passes almost horizontally above the level of the clavicle. The posterior triangle of the neck near the supraclavicular brachial plexus contains prominent vascular structures. These vessels include the dorsal scapular and suprascapular arteries (branches of the thyrocervical trunk or subclavian artery) often close to the planned needle trajectory or plexus and in some instances the vessels bisect the plexus [5].
Indications
Surgical
Supraclavicular brachial plexus block is indicated for surgery on the shoulder and entire upper extremity. Potentially supraclavicular block may miss the suprascapular nerve (C5 origin from the upper trunk) and supraclavicular nerve (C4 origin) from the cervical plexus, both important for innervation of the shoulder. Supraclavicular block may be “ulnar sparing” if local anesthetic fails to reach the anterior division of the inferior trunk due to its deep anteromedial location between the subclavian artery and the first rib. However a properly executed supraclavicular block has the potential to anesthetize the entire upper limb. It is suitable for surgical anesthesia or postoperative analgesia.
Evidence and Safety
Supraclavicular block is considered a reliable, fast-onset approach to the brachial plexus, and the term spinal of the arm reinforces this concept. However, randomized controlled trials have demonstrated that the supraclavicular approach has similar [38] or reduced [39, 40] efficacy compared to other approaches to the brachial plexus from below the clavicle. Controlled clinical trials also demonstrate that the rate of ulnar nerve sensory block is reduced following ultrasound-guided supraclavicular block compared to other approaches from below the clavicle [40, 41] and that the volume required for sensory blockade is not that different to the volume required using techniques not employing ultrasound guidance [42]. The supraclavicular block has been subject to large-scale studies investigating quality and safety [11, 36, 43].

Full access? Get Clinical Tree