Brachial Plexus Blocks
A. Interscalene Block
Anthony R. Brown
injected with repeated aspiration for blood every 5 mL to be distributed around the brachial plexus (Fig. 7-3).
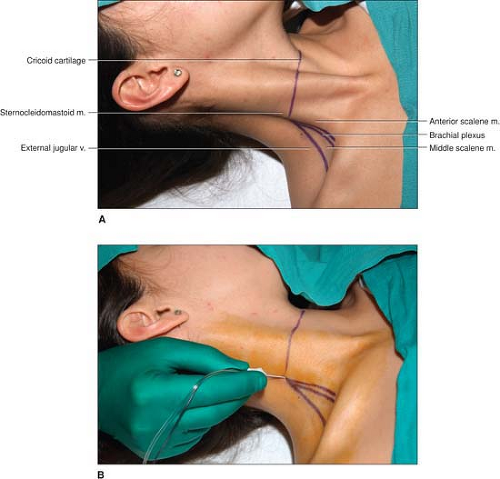
 Figure 7-1. The cricoid cartilage, the clavicular head of the sternocleidomastoid muscle, and the anterior and middle scalene muscles with the interscalene groove in between. |
Testing the Motor Block: (a) Inability to elevate the arm (the “deltoid sign”). (b) The “money sign,” in which the patient rubs the thumb against the index and middle fingers indicating the onset of paresthesia or numbness in the distribution of C6 and C7.
Testing the Sensory Block: Loss of sensation over the upper lateral aspect of the upper arm in the distribution of the C6 dermatome.
Sedation should be minimal, its purpose to allay anxiety without inhibiting the ability of the patient to communicate.
In a limited number of patients, the clavicular head of the sternocleidomastoid muscle is either not present or exists as an indistinct band. In these situations, the interscalene groove is situated 3 cm lateral to the lateral border of the main belly of the sternocleidomastoid muscle at the level of the cricoid cartilage. This “3-cm mark” is a useful aid in obese individuals as well. Additional landmarks include the external jugular vein and the pulsation of the subclavian artery as it crosses over the first rib between the anterior and middle scalene muscles at the lower end of the interscalene groove.
Patient discomfort is reduced by superficially infiltrating the skin with lidocaine using a 26-gauge needle.
To facilitate the insertion of the insulated needle, the skin can first be punctured with an 18-gauge needle.
Insertion of the insulated needle with the bevel facing the sheath increases the likelihood of feeling the tactile sensation of “popping through the sheath.”
Diaphragmatic movement is indicative of stimulation of the phrenic nerve and of needle placement medial/anterior to the interscalene groove. The needle should be withdrawn and redirected in a more lateral/posterior direction. In contrast, a suprascapular or trapezius muscle contraction is indicative of needle placement lateral to the interscalene groove. The needle should be withdrawn and redirected in a more medial/anterior direction.
Positioning of the needle to maintain a motor response at 0.3 to 0.5 mA is associated with a high success rate.
It is essential that the caudal direction of the needle be maintained (Fig. 7-4). Insertion of the needle in a neutral/horizontal direction (i.e., midway between caudal
and cephalad) or in a cephalad direction facilitates neuraxial positioning of the needle as well as the vertebral artery injection of local anesthetic.
Figure 7-3. The local anesthetic is slowly injected with repeated aspiration for blood every 5 mL to be distributed around the brachial plexus.
A triangular-shaped swelling of the apex at the point of needle insertion and the base at the lower end of the interscalene groove may be noted, especially in thin individuals, as the injection progresses and is indicative of correct needle placement. In contrast, a circular swelling around the point of needle insertion is more likely indicative of injection into the subcutaneous tissues (i.e., superficial to the brachial plexus sheath).
“Pressure paresthesia,” which is described as a dull ache following the rapid injection of 2 to 3 mL of local anesthetic, should be differentiated from the severe pain produced by an intraneural injection. This “pressure paresthesia” appears to be more commonly encountered with an interscalene block than with other peripheral nerve blocks and may be referred to the shoulder or more distally.
This block is not indicated alone for a surgery involving an area around the axilla (e.g., inferior capsular shift). In addition, variations in the extent of T2 innervation may result in inadequate anesthesia of the anterior and posterior arthroscopic portal sites. These limitations can be overcome by local infiltration to the appropriate sites.
An interscalene block is not indicated alone for surgery to the medial aspect of the upper extremity, as nerve roots C8 and T1 are not consistently blocked with this approach to the brachial plexus.
Side effects are commonly associated with an interscalene block. A 100% incidence of phrenic nerve blockade (due to the phrenic nerve’s C3-5 derivation) occurs, resulting in paresis of the ipsilateral diaphragm. This results in a 25% to 30% reduction in pulmonary function volumes. Caution is therefore advised in patients with significantly reduced lung function. The patient should be reassured that hoarseness (vasodilation of the larynx and arytenoids or blockade of the recurrent laryngeal nerve) and Horner syndrome (cervical sympathetic nerve block) are benign and transient.
Serious complications associated with the performance of this block include epidural, subdural, and spinal injections and even injections directly into the spinal cord; arterial (vertebral artery) and venous intravascular injections; as well as pneumothorax.
Suggested Readings
Benumof JL. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia. Anesthesiology 2000;93:1541–1544.
Borgeat A, Ekatodramis G, Kalberer F, et al. Acute and nonacute complications associated with interscalene block and shoulder surgery. Anesthesiology 2001;95:875–880.
Brown A. Regional anesthesia for shoulder surgery. Tech Reg Anesth Pain Manag 1999;3:64–78.
Brown AR. The use of a “reverse” axis (axillary-interscalene) block in a patient presenting with fractures of the left shoulder and elbow. Anesth Analg 2001;93:1618–1620.
Casati A, Fanelli G, Aldegheri G, et al. Interscalene brachial plexus anaesthesia with 0.5%, 0.75% or 1% ropivacaine: a double-blind comparison with 2% mepivacaine. Br J Anaesth 1999;83: 872–875.
Klein S, Greengrass R, Steele S, et al. A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg 1998;87:1316–1319.
Roch J, Sharrock N, Neudachin L. Interscalene brachial plexus block for shoulder surgery: a proximal paresthesia is effective. Anesth Analg 1992;75:386–388.
Silverstein W, Saiyed M, Brown A. Interscalene block with a nerve stimulator: a deltoid motor response is a satisfactory endpoint for successful block. Reg Anesth Pain Manag 2000;25:356–359.
Urmey W. Interscalene block. Tech Reg Anesth Pain Manag 1999;3:207–211.
Urmey W, McDonald M. Hemidiaphragmatic paresis during interscalene brachial plexus block: effects on pulmonary function and chest wall mechanics. Anesth Analg 1992;74:352–357.
Winnie A. Interscalene brachial plexus block. Anesth Analg 1970;49:455–466.

Full access? Get Clinical Tree