CHAPTER 8
Botulinum Toxins
BACKGROUND
Botulinum toxins are neurotoxins produced by the gram-positive, spore-forming, anaerobic bacteria, Clostridium botulinum, as well as C butyricum, C baratii, and C argentinense.1,2 These toxins are the most deadly human neurotoxins known. Clinically, botulism can occur following ingestion of contaminated food or from a wound infection. The clinical signs of botulism include limb paralysis, facial weakness, ophthalmoplegia, dysarthria, dysphagia, dyspnea progressing to respiratory arrest, constipation progressing to ileus, and urinary retention.3 C botulinum produces 7 antigenically (immunologically) distinct neurotoxins: A, B, C1, D, E, F, and G.
• Varied mechanisms of action of botulinum neurotoxin (BoNT) subtype are believed to be due to its ability to inhibit multiple neurotransmitters from presynaptic vesicles. Specific proteins involved in this process are affected by different toxins and thus different strains of toxin do not necessarily work via the same mechanism.
• Only types A and B toxin are currently routinely used in clinical practice.
• Currently, there are 3 types of botulinum toxin type A commercially available in the United States including onabotulinum toxin A (Botox), abobotulinum toxin A (Dysport), and incobotulinum toxin A (Xeomin).
• Rimabotulinum toxin B (Myobloc) is the only botulinum toxin type B currently available in the United States.
• Each toxin has been developed with different dosing units and they are not interchangeable—this is clinically important to remember. Synaptosomal-associated protein (SNAP 25) is inactivated by botulinum toxin type A and vesicle associated membrane protein (VAMP) is inactivated by botulinum toxin type B.
• Its effect on motor function through inhibition of release of acetylcholine has been well documented. Cleavage of either one of these proteins results in inhibition of acetylcholine release, disruption of neuromuscular transmission, and paralysis of the muscle.
• Most important recent scientific discovery is of SNAP 25 on motor and sensory neurons.
• Several animal studies demonstrating the toxin’s inhibition of substance P, calcitonin-gene related peptide (CGRP), glutamate, bradykinin, ATP, and purinergic receptors.
• Additional animal studies have suggested a clinically relevant central analgesic effect of type A toxin as well.
The only FDA-approved specific pain indication for any current commercially available botulinum toxin is chronic migraine for onabotulinum toxin A (Botox).4 The “off-label” use of botulinum toxin for the treatment of other chronic painful conditions has been reported for cervical dystonia–associated neck pain, chronic low back pain, and chronic lateral epicondylitis. Jabbari and Machado have recently published a review of the use of botulinum toxin for refractory pain based on the evidence according to the AAN evidence rating approach. The reader can review these references for additional information regarding the use of botulinum toxins for chronic pain.
BOTULINUM TOXIN FOR THE TREATMENT OF CHRONIC MIGRAINE
The most evidence for treatment with botulinum toxin is for the specific condition, chronic migraine. The importance of defining this group has become vital for proper patient selection. The FDA has approved the use of onabotulinum toxin A (Botox) for the treatment of chronic migraine only, and not tension type or episodic migraine.
Chronic migraine has been defined as:
• A headache syndrome for more than 3 months
• At least 15 or more headache days per month
• The headache experienced for at least 4 hours
• The headache experienced for at least 8 months
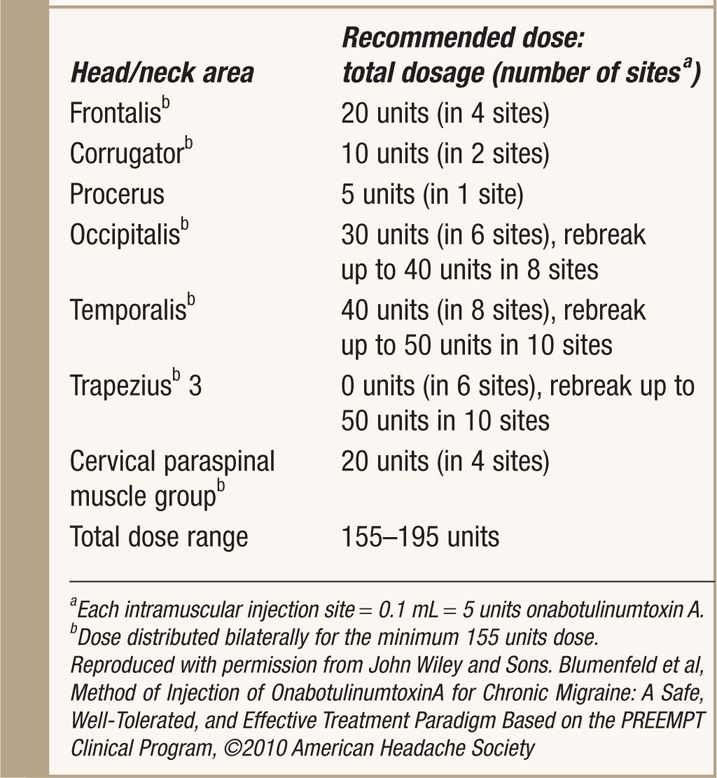
A randomized placebo controlled study examined the use of 100 units of onabotulinum toxin in fixed injection sites including the glabella, frontalis, temporalis, trapezius, and suboccipital regions in 41 patients with chronic migraine. Onabotulinum toxin A resulted in fewer migraine episodes 4 weeks after injection with both reduced headache days and a reduced headache index (composite measure of both headache frequency and intensity) at 16 weeks. Two much larger studies, PREEMPT 1 and PREEMPT 2 each evaluating approximately 700 patients consisted of a 24-week blinded period followed by an extended open label arm. In contrast to the smaller study, which excluded chronic headache associated with medication overuse, the PREEMPT trials included these patients. The primary outcome measure for PREEMPT 1, the number of headache episodes, was not met but in PREEMPT 2, the primary outcome measure, the number of headache days, was met. The change in headache days for treated patients in PREEMPT 2 was 9 days vs. 6.7 days for placebo treated patients (p<0.001). PREEMPT 1 did meet its secondary outcomes including number of migraine days. The FDA approved onabotulinum toxin A for the treatment of chronic migraine in October, 2010, noting that it felt that a reduction in headache days was more meaningful than a reduction in absolute number of headaches. The injection paradigm used in the PREEMPT trials is seen in Table 8-1. Many consider the availability of this treatment to be a great advance in the ability to treat chronic migraine. Published studies and our own experience would suggest that other headache syndromes, for example, episodic migraine, or tension-type headache are not clearly responsive to onabotulinum toxin A (Botox) injections.
TABLE 8-1. Onabotulinumtoxin A Dosing for Chronic Migraine by Muscle Using the PREEMPT Injection Paradigm
BASIC CONCERNS AND CONTRAINDICATIONS
Preprocedure Considerations
• Informed consent and appropriate explanation of the procedure including the potential benefits as well as risks.
• We have performed with procedure safely in individuals on antiplatelet or anticoagulant therapy only after checking with the physician prescribing such treatment.
• The patient can be seated during the procedure.
• This procedure is contraindicated with a known allergy or hypersensitivity to onabotulinum toxin A (Botox).
• Fluoroscopy is not required nor recommended for this procedure.
Equipment
• Onabotulinum toxin A (Botox) is supplied in single-use 100 units or 200 units per vial.
• Four 1 cc syringes
• Two 3 cc syringes
• 20 gauge 1.5 in needle for reconstitution
• 30 gauge ½ -1 needle for injection
Botox must be reconstituted before using as toxin in the vial is vacuum dried.
The manufacturer of Botox recommends reconstituting the toxin with sterile, preservative free 0.9% sodium chloride USP; however, some injectors have described successfully reconstitution with 1% preservative free lidocaine. The dilution instructions for Botox vials are seen in Table 8-2. After drawing up the appropriate amount of diluent into the correct size syringe, it should be slowly injected into the vial and then gently mixed by gentle rotation of the vial. The Botox should be administered within 24 hours after constitution and it can be stored after reconstitution in a refrigerator during this 24-hour period (2°-8°C).

Full access? Get Clinical Tree






