Key Clinical Questions
How are blast-induced injuries classified?
What organ systems are typically affected in blast-induced polytrauma?
Are there strategies to predict which patient might experience delayed onset of primary blast injuries?
What are current management strategies for specific primary blast injuries?
How are blast-induced traumatic brain injuries classified?
How does blast-induced traumatic brain injury (TBI) differ from other types of traumatic brain injuries?
How can secondary insults to TBIs be avoided?
What are the current diagnostic and management strategies for mild, moderate, and severe TBI?
Introduction and Epidemiology
The incidence of explosive blast injuries is on the rise. From 1996 to 2006, it is estimated that blast-related events have risen fourfold. Although there have been a number of explosive blast events worldwide, the actual number of mass casualty blast events occurring on United States soil have been relatively few. In 1995, a large explosive device composed of fuel oil and fertilizer was detonated in front of the Alfred P. Murrah Federal Building in Oklahoma, which resulted in 518 injuries and 168 deaths. More recently, the 2001 World Trade Center terrorist attack has resulted in more focus on homeland security and disaster preparation for these events. A civilian physician may have to respond to domestic terror events such as bombings in subways, trains, public gatherings, and nightclubs. The National Counterterrorism Center reported in 2007 that approximately 14,000 terrorist attacks have occurred worldwide, resulting in about 44,000 injuries and more than 22,000 deaths. This represented a 20% to 30% increase since 2006.
Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) in Afghanistan have greatly increased our knowledge and experience in treating blast injuries. A recent study of the Joint Theater Trauma Registry (JTTR) revealed that explosive blasts accounted for almost 80% of all combat casualties from October 2001 through January 2005. The most common explosive weapon employed in OIE/OEF is the improvised explosive device (IED), which broadly describes any makeshift incendiary device constructed to injure, incapacitate, harass, or distract. Most IEDs utilize conventional military weapons (ie, artillery shells, plastic explosives, etc.) with various detonating triggers (ie, pressure plate, cellular phone, remote control) and are employed almost anywhere (ie, roadside, suicide bomber, vehicle-borne). Typical injuries seen from an IED blast have concentrated mainly on extremity and head injuries. This is likely due to advanced body armor systems currently used that afford good protection from blast injuries in the torso region.
Pathophysiology
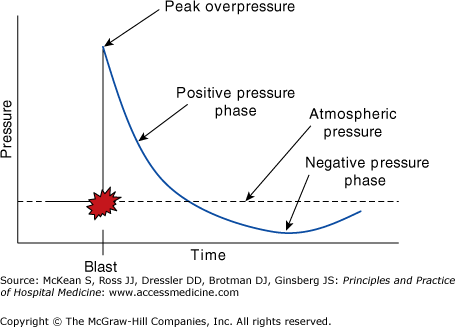
The complex physics of an explosive blast can result in a myriad of injuries on multiple victims. An explosion results in sudden and near instantaneous expansion of gas that results in a shockwave also known as a blast wave. As this blast wave travels, it begins to lose its pressure and velocity with distance and time (Figure 268-1). A blast wave is made of two components: a shockwave of high pressure, followed closely by a blast wind. Blast winds can be strong enough to propel people or objects, thus resulting in secondary injury. As the explosive shockwaves dissipate, a “negative-pressure” phase occurs as a result of the void created by dissipated air. These rapid pressure fluctuations have a destructive effect on the human body, particularly in organs at the air-tissue or air-fluid interface. These include organs such as the lungs and bowel. Two main types of energy are created by a blast that enter the body, specifically stress waves and shear waves. Stress waves are longitudinal pressure forces that result in a spalling effect occurring at air-tissue interfaces, whereas shearing waves are transverse pressure forces that result in movement along tissue planes and possible disruption along attachment sites.
Blast injuries are traditionally classified into four categories: primary, secondary, tertiary, and quaternary (Table 268-1). Primary blast injuries occur as a result of the overpressure forces from the blast shockwave itself, thus representing true barotrauma to the body. Organs that are air-filled or contain air-fluid interfaces are typical of primary blast injuries. These include the lungs, ears, intestines, and colon. Secondary blast injuries are typically penetrating in nature and a result of ballistic trauma from fragments of the explosive device itself or other objects propelled into the body as a result of blast overpressure or blast winds. Tertiary blast injuries describe injuries sustained as a result of being thrown into stationary objects as a result of the peak overpressure or blast wind. It also includes injuries sustained from building or structural collapse, resulting in crush injuries. Quaternary blast injuries include all other forms of injury not falling into the first three classes, which include burns, toxic substance exposures, inhalation injuries, and radiation injuries. There is some debate over the use of a fifth classification known as quinary blast injuries, which are described mainly as having a hyper-inflammatory state sometimes seen in blast patients developing sometime after initial insult. Some authors have attributed this to the exposure of bacteria or radiation material from a blast and thus at times classify these injuries as quaternary.
| Category | Definition | Example Injury |
|---|---|---|
| Primary | Injuries produced as a direct effect from blast wave and pressure changes |
|
| Secondary | Injuries from explosive fragments or other objects propelled by overpressure and blast winds |
|
| Tertiary | Injuries produced from being thrown into a stationary object or from collapse of buildings and structures |
|
| Quaternary | Other explosion-related injuries, illnesses, or diseases |
|
| “Quinary” | Delayed/remote hyperinflammatory state induced after an explosive blast or exposure to radiation or bacteria |
|
Two important factors affect the magnitude of injury from an explosive blast. The first is the distance a person is from an explosion. The closer a person is to the explosion, the greater the blast overpressure is experienced. Individuals who are positioned further away from a blast will probably not experience the consequences of primary blast injuries due to the degradation of the pressure forces created by the blast over time. A second factor that amplifies the magnitude of a blast pressure is if detonation occurs within an enclosed space. The pressure forces generated from open-space detonations dissipate over unlimited space. In an enclosed space, however, the overpressure waves become amplified as they reflect off walls and solid surfaces, resulting in increased force. Immediate death from primary blast injuries (ie, blast lung) occurs more often with enclosed space blasts rather than open air blasts. This is supported from recent JTTR data (2004–2006) from OIF/OEF, which revealed the incidence of primary blast injuries at only 12.2%, of which 75% were tympanic membrane rupture. Blast overpressure was the cause of death in only 1.5% cases, which underscores the fact that IED blasts typically occur in open spaces and that most injuries and deaths are due to fragments.
Does This Patient Have a Blast-Induced Traumatic Brain Injury or Polytrauma?
Explosive blasts are a rare mechanism of traumatic brain injury (TBI) in the United States. Most TBIs occurring in the U.S. are a result of direct blunt-force trauma from falls and motor vehicle crashes. Data from the Centers for Disease Control and Prevention show an annual incidence of emergency department visits and hospital admissions for TBI to be 403 per 100,000 and 85 per 100,000 respectively. The cost for direct TBI medical care is estimated at more than $56 billion per year. Current operations in Iraq and Afghanistan have yielded significant experience in the understanding and management of blast-induced TBI. The incidence of head injuries has not substantially increased in these wars compared with others. A major difference, however, is the high survival of combat-injured soldiers including those injured from TBI, compared to previous wars. Much of this success has been attributed to advanced body armor systems. Conservative estimates for returning U.S. service members indicate that approximately 20% of the deployed force potentially suffered some form of TBI.
Traumatic brain injury has classically been categorized based on severity of symptoms: mild, moderate, and severe. Patients with mild TBI usually have a Glasgow Coma Scale at time of medical evaluation (GCS, Table 268-2) of 14 to 15 and experience brief if any loss of consciousness (LOC). Typical complaints include headaches, confusion, and amnesia. Mild TBI is frequently referred to as a “concussion” in lay-person terms. Following an acute period, most patients with mild TBI may continue to experience nonspecific symptoms such as headache, dizziness, anxiety, difficulty with concentration, depression, and insomnia lasting from a few weeks up to a year. This is known as the “postconcussive” syndrome. Patients with moderate TBI on initial medical evaluation will have a GCS of 9 to 13 and usually experience a longer period of unconsciousness.
| Best Motor Response (M) | Best Verbal Response (V) | Best Eye Opening (E) | |||
|---|---|---|---|---|---|
| Follows commands | 6 | ||||
| Localizes pain | 5 | Oriented, alert | 5 | ||
| Withdraws from pain | 4 | Confused, appropriate | 4 | Opens eyes spontaneously | 4 |
| Flexor posturing | 3 | Disoriented, inappropriate | 3 | Opens eyes to voice | 3 |
| Extensor posturing | 2 | Incomprehensible sounds | 2 | Opens eyes to pain | 2 |
| No response | 1 | No response | 1 | No response | 1 |
Neurologic deficits become apparent with this level of TBI and typically warrant computed tomography studies as well as hospital admission for observation. These patients are more likely to have abnormalities found on neuroimaging studies and may require specialty consultation. Patients with severe TBI will have a GCS score of 8 or less and significant neurologic deficits on physical exam. These patients routinely have some abnormality present on neuro-imaging (ie, intracranial hemorrhage, skull fracture, cerebral edema, etc.) and require intubation for airway protection as well as admission to an intensive care unit for further monitoring and critical care. Mortality is closely tied to the severity of TBI with mild TBI patients having better outcomes and reduced mortality compared with severe TBI patients. Mortality for patients admitted with a presenting GCS < 13 is approximately 30%. This number rises to greater than 50% mortality for patients presenting with a GCS of 8 or less. Prognostic factors of poor TBI outcomes include age 65 and older, penetrating mechanism of injury, and bilaterally fixed pupils on initial presentation. The actual injury inflicted on the brain has been described in two distinct phases: primary and secondary,

Full access? Get Clinical Tree