43 Bedside Monitoring of Pulmonary Function
 Pulse Oximetry
Pulse Oximetry
Pulse oximetry is a microprocessor-based instrument that incorporates both oximetry and plethysmography to provide continuous noninvasive monitoring of the oxygen saturation of arterial blood (SpO2). Often considered the “fifth vital sign,” it is one of the most important technologic advances for monitoring patients during anesthesia, in the intensive care unit (ICU), on the general ward, in the emergency department, and during a wide variety of procedures.1–3 The pulse oximeter probe is embedded into either a clip or an adhesive wrap and consists of two light-emitting diodes on one side, with a light-detecting photodiode on the opposite side. Either a finger or an earlobe serves as the sample “cuvette.” The tissue bed is transilluminated, and the forward-scattered light is measured. Pulse oximetry targets the signal arising from the arterial bed as light absorbance fluctuates with changing blood volume. Arterial blood flow causes signal changes in light absorption (the pulsatile component called photoplethysmography) that can be distinguished from venous and capillary blood in the surrounding tissues (the baseline, or direct current, component; Figure 43-1).
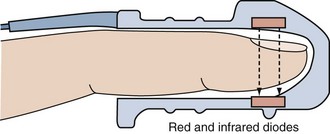
Figure 43-1 Schematic depiction of the pulse oximeter light absorption signal.
(Adapted with permission from Phillips Medical Systems, Carlsbad, California.)
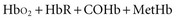
Oximetry uses spectrophotometry to determine SaO2. According to the Beer-Lambert law, the concentration of a substance can be determined by its ability to transmit light.4 Oxygenated hemoglobin (HbO2) and deoxygenated or “reduced” hemoglobin (HbR) species absorb light differently, so that the ratio of their absorbencies can be used to calculate saturation. In addition, there are two minor hemoglobin (Hb) species: carboxyhemoglobin (COHb) and methemoglobin (MetHb). Fractional SaO2 is the proportion of oxygenated hemoglobin relative to the four hemoglobin species:
Measuring fractional hemoglobin requires a co-oximeter that incorporates four wavelengths to distinguish each species (Figure 43-2). In contrast, oxygen saturation as determined by pulse oximeter (SpO2) uses two wavelengths, so that it measures functional SaO2:
Accuracy and Precision
Because pulse oximeters themselves cannot be calibrated, their accuracy is highly variable and dependent on both the calibration curve programmed into the monitor and the quality of signal processing.5,6 The ratio of absorbencies is calibrated empirically against SaO2 measured by co-oximetry in normal volunteers subjected to various levels of oxygenation. Pulse oximeters are calibrated against measured SaO2 down to 70% (saturations below this level are determined by extrapolation).5 The resulting calibration curve is stored in the monitor’s microprocessor to calculate SpO2.6
The accuracy of the calibration curve depends on laboratory testing conditions (co-oximeter used, range of oxygenation studied, and characteristics of sample subjects). Most manufacturers report an accuracy of ±2% at an SaO2 greater than 70% and ±3% when the SaO2 is 50% to 70%.2 In normal subjects tested at an SaO2 between 99% and 83%, pulse oximetry has a bias and precision that are within 3% of co-oximetry.7 However, under hypoxic conditions (SaO2 78% to 55%), when the monitor must rely on extrapolated values, bias increases (8%) and precision deteriorates (5%).7 Likewise, in critically ill patients, pulse oximeters historically perform well when the SaO2 is greater than 90% (bias of 1.7%; precision of ±1.2%), but accuracy diminishes at an SaO2 below 90% (bias of 5.1%; precision of ±2.7%)8 (Figure 43-3). Technologic advances over the past decade have apparently improved this performance; a recent study comparing pulse oximetry to co-oximetry reported a bias of 0.19% and a precision of ±2.22% over an SaO2 range of 60% to 100%.9
Dynamic Response
Because pulse oximeters detect very small optical signals (and must reject a variety of artifacts), data must be averaged over several seconds, thus affecting response time.5 Pulse oximeters may register a near-normal SpO2 when the actual SaO2 is less than 70%.5 A prolonged lag time is more common with finger probes than ear probes5,10,11 and is attributed to hypoxia-related peripheral vasoconstriction.5 Bradycardia also is associated with a prolonged response time.11
Sources of Error
Motion artifact and low perfusion are the most common sources of SpO2 inaccuracies, because the photoplethysmographic pulse signal is very low in these settings compared with the total absorption signal.12,13 The combination of motion artifact and low perfusion substantially lowers SpO2 accuracy compared with either artifact alone.14 Causes of motion artifact include shivering, twitching, agitation, intraaortic balloon pump assistance, and patient transport.15,16 Signs of motion artifact include a false or erratic pulse rate reading or an abnormal plethysmographic waveform. Peripheral hypoperfusion from hypothermia, low cardiac output, or vasoconstrictive drugs may increase bias, reduce precision, and prolong the detection time for a hypoxic event.16 Newer technologies have helped reduce the incidence of these problems but they have not been eliminated as a source of error. Relocation of the probe may be required to obtain a more accurate signal.
Despite recent technologic advances, there still are a number of factors that may affect the accuracy of the pulse oximeter. Table 43-1 lists the most common factors.
TABLE 43-1 Common Factors Affecting Pulse Oximetry Measurements
| Factor | Effect |
|---|---|
| Carboxyhemoglobin (COHb) | Slight reduction of the assessment of oxygen saturation (SaO2) by pulse oximetry (SpO2) (i.e., overestimates the fraction of hemoglobin available for O2 transport) |
| Methemoglobin (MetHb) | At high levels of MetHb, SpO2 approaches 85%, independent of actual SaO2 |
| Methylene blue | Transient, marked decrease in SpO2 lasting up to several minutes; possible secondary effects as a result of effects on hemodynamics |
| Anemia | If SaO2 is normal, no effect; during hypoxemia with Hb values less than 14.5 g/dL, progressive underestimation of actual SaO2 |
| Ambient light interference | Bright light, particularly if flicker frequency is close to a harmonic of the light-emitting diode switching frequency, can falsely elevate the SpO2 reading |
| Blood flow | Reduced amplitude of pulsations can hinder obtaining a reading or cause a falsely low reading |
| Motion | Movement, especially shivering, may depress the SpO2 reading |
| Nail polish | Slight decrease in SpO2 reading, with greatest effect using blue nail polish, or no change |
| Sensor contact | “Optical shunting” of light from source to detector directly or by reflection from skin results in falsely low SpO2 reading |
| Skin pigmentation | Small errors or no significant effect reported; deep pigmentation can result in reduced signal |
| Tape | Transparent tape between sensor and skin has little effect; falsely low SpO2 has been reported when smeared adhesive is in the optical path |
| Vasodilation | Slight decrease |
| Venous pulsation | Artifactual decrease in SpO2 |
Dyshemoglobins and Vascular Dyes
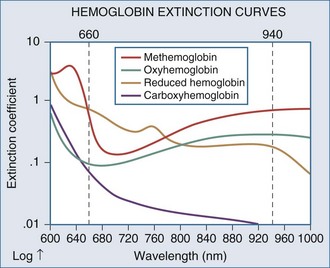
Significant amounts of COHb or MetHb can cause errors in SpO2. Carboxyhemoglobin and HbO2 absorb equivalent amounts of red light, so carbon monoxide poisoning results in a falsely elevated SpO2 because the pulse oximeter reports total Hb saturation not just HbO2 saturation. In the setting of carbon monoxide poisoning, the amount of COHb is elevated, resulting in a falsely high SpO2. The patient, however, could be experiencing profound hypoxemia. In contrast, MetHb causes substantial absorption of both red and infrared light, so the ratio approaches 1 (estimated SpO2 of 85%).4 Significant MetHb causes falsely low SpO2 values when the actual SaO2 is greater than 85% and falsely high values when the SaO2 is less than 85%.4 Administration of methylene blue or indocyanine green dyes for diagnostic tests causes a false, transient (1- to 2-minute) drop in SpO2 to as low as 65%.17,18
Nail Polish and Skin Pigmentation
Both dark skin pigmentation and dark nail polish interfere with absorption of the wavelengths used by pulse oximetry. Pulse oximeters thus have greater bias and less precision in black patients.8 Whereas an SpO2 of 92% is sufficient to predict adequate oxygenation in white patients, a saturation of 95% is required in black patients.8 Dark nail polish can falsely lower SpO2, whereas red polish tends not to affect accuracy.19 However, with newer technology, the negative effects of nail polish are lessened. A recent study showed that there was an effect of dark nail polish on the pulse oximetry reading, but it was not clinically relevant.20 When nail polish cannot be removed, mounting the oximeter probe sideways on the finger yields an accurate reading.21
Ambient Light, Anemia, and Hyperbilirubinemia
Although pulse oximeters compensate for the presence of ambient light, the sensor should be shielded from intense light sources with an opaque material. Falsely low SpO2 readings occur when even minor gaps exist between the probe and skin, allowing reflected light off the skin surface to “shunt” directly to the photodiode.22 Xenon surgical lamps and fluorescent lighting can cause a falsely low SpO2.23 Under conditions of anemia (Hb 8 g/dL) and severe hypoxia (SaO2 54%), SpO2 bias is markedly increased (−14%).24 Hyperbilirubinemia does not affect SpO2 directly.25 However, carbon monoxide is a byproduct of heme metabolism, and icteric patients tend to have higher levels of COHb,25 so SpO2 may be falsely elevated.
Reflectance Pulse Oximetry
Reflectance pulse oximetry was designed to counter signal-detection problems associated with finger probes during hypoperfusion. The reflectance sensor is designed for placement on the forehead just above the orbital area, where superficial blood flow is abundant and less susceptible to vasconstriction.26 Whereas traditional probes work by transilluminating a tissue bed and measuring the forward-scattered light on the opposite side of the finger or earlobe, reflectance probes are constructed with the light-emitting diodes and the photodetector located on the same side. The photodetector measures the back-scattered light from the skin.26 In addition, more liberal placement sites for reflectance pulse oximetry has allowed fetal monitoring during labor.27 Intraesophageal SpO2 monitoring is currently under investigation.28 Anasarca, excessive head movement, and difficulty in securing the probe site are some of the problems encountered with reflectance pulse oximetry.29 Light “shunting” from poor skin contact and direct sensor placement over a superficial artery are associated with artifacts.30 Reflectance pulse oximetry is also limited by poor signal-to-noise ratio and variability among sites in the arrangement of blood vessels and tissue blood volume.30 However, recent studies have shown reflectance pulse oximetry to be as effective as finger sensors in many situations.31–34
Technologic Advances
Recent advances in signal analysis and processing have markedly improved SpO2 accuracy during low perfusion and reduced the problem of motion artifact.16,35 According to recent independent testing, these advances occur with pulse oximeters made by several manufacturers.36 Durban and Rostow reported that new pulse oximeter technology can accurately detect SaO2 in 92% of the cases in which traditional SpO2 monitoring failed owing to low perfusion and motion artifact37 (Box 43-1).
Box 43-1
Aarc Clinical Practice Guideline: Pulse Oximetry
Indications
Precautions
Assessment of Need
Assessment of Outcome
 SpO2 results should reflect the patient’s clinical condition (i.e., validate the basis for ordering the test).
SpO2 results should reflect the patient’s clinical condition (i.e., validate the basis for ordering the test).From AARC clinical practice guideline: pulse oximetry. Respir Care 1992;37:891-7.
 Capnometry
Capnometry
Capnometry consists of the measurement and numeric display of expired carbon dioxide (CO2) at the patient’s airway opening.38 When a waveform plotting CO2 against time or volume is also displayed, it is referred to as capnography, and the waveform is referred to as a capnogram.38 Capnometry is most commonly used on patients receiving mechanical ventilation and works by passing infrared light through a sample chamber to a detector on the opposite side. CO2 absorbs infrared light at a peak wavelength of approximately 4.27 µm.38,39 More infrared light passing through the sample chamber (i.e., less CO2) causes a larger signal in the detector relative to the infrared light passing through a reference cell. The sample chamber is either connected directly to the Y-adapter of the ventilator circuit (mainstream), or by a sampling line at the Y-adapter that continuously aspirates gas into a sampling chamber located inside the monitor (sidestream).
Clinical Applications
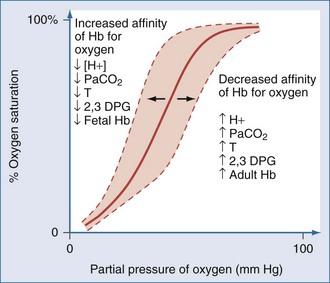
Capnometric determination of the partial pressure of CO2 in end-tidal exhaled gas (PETCO2) is used as a surrogate for the partial pressure of CO2 in arterial blood (PaCO2) during mechanical ventilation40,41 (Figure 43-4). Although widely available today, the utilization of PETCO2 to represent PaCO2 in ICUs remains unclear. While perhaps not an exact match for PaCO2, PETCO2 does provide a valuable trending tool. Also, with newer technologies, the accuracy of PETCO2 measurements is improving. In a recent study, McSwain et al. showed strong correlations between PETCO2 and PaCO2 across a wide range of dead-space conditions.42 Capnometry is used for a variety of purposes, such as the diagnosis of pulmonary embolism, determination of lung recruitment response to positive end-expiratory pressure (PEEP), detection of intrinsic PEEP, evaluation of weaning, indirect marker of elevated dead-space ventilation, assessment of cardiopulmonary resuscitation, indirect determination of cardiac output through partial CO2 rebreathing, verification of endotracheal cannulation, detection of airway accidents, and even determination of feeding tube placement.43–55 Guidelines for the use of capnometry/capnography are outlined by the American Association for Respiratory Care (Box 43-2).
Box 43-2
Aarc Clinical Practice Guideline: Capnography/Capnometry During Mechanical Ventilation
Indications
 Monitoring severity of pulmonary disease and evaluating response to therapy, especially therapy intended to improve the ratio of dead space to tidal volume (VD/VT) and the matching of ventilation to perfusion (V/Q) and, possibly, to increase coronary blood flow.
Monitoring severity of pulmonary disease and evaluating response to therapy, especially therapy intended to improve the ratio of dead space to tidal volume (VD/VT) and the matching of ventilation to perfusion (V/Q) and, possibly, to increase coronary blood flow. Evaluation of the efficiency of mechanical ventilatory support by determination of the difference between PaCO2 and PETCO2.
Evaluation of the efficiency of mechanical ventilatory support by determination of the difference between PaCO2 and PETCO2. Estimation of effective (nonshunted) pulmonary capillary blood flow by a partial rebreathing method.
Estimation of effective (nonshunted) pulmonary capillary blood flow by a partial rebreathing method.From AARC clinical practice guideline: capnography/capnometry during mechanical ventilation. Respir Care 2003;48:534-9.
Precautions and Possible Complications
Assessment of Need
Assessment of Outcome
PaCO2-PETCO2 Gradient
Normal subjects have a PaCO2-PETCO2 gradient of 4 to 5 mm Hg.40,43,47,56–60 In critically ill patients, the PaCO2-PETCO2 gradient can be markedly elevated, with a tendency toward wider gradients in obstructive lung diseases (7-16 mm Hg) than in acute lung injury or cardiogenic pulmonary edema (4-12 mm Hg).46,47,61–63 A strong correlation between ΔPETCO2 and ΔPaCO2 (r = 0.82), along with minor bias and reasonable precision between PETCO2 and PaCO2, suggests that arterial blood gas monitoring may not be needed to assess ventilation unless the ΔPETCO2 exceeds 5 mm Hg.48 Yet several studies found that the ΔPETCO2 often falsely predicts the degree and direction of ΔPaCO2.58–6063 Therefore, despite PETCO2 monitoring, routine arterial blood gas analysis is still required in critically ill patients.
Several factors determine the PaCO2-PETCO2 gradient. Whereas PaCO2 reflects the mean partial pressure of CO2 in alveolar gas (PaCO2), PETCO2 approximates the peak PaCO2.64 During expiration, lung regions with high ventilation-to-perfusion ratios dilute the mixed CO2 concentration so that PETCO2 is usually lower than PaCO2.65 However, when CO2 production is elevated (or expiration is prolonged), PETCO2 more closely resembles mixed venous PCO2, as a higher amount of CO2 diffuses into a progressively smaller lung volume.64 Thus, the PaCO2-PETCO2 gradient can be affected by changes in respiratory rate and tidal volume (VT) due to alterations in expiratory time and by CO2 production and mixed venous CO2 content.64 In fact, it is not uncommon for PETCO2 to exceed PaCO2.65 Inotropic or vasoactive drugs may affect the PaCO2-PETCO2 gradient in an unpredictable manner, either by increasing cardiac output and pulmonary perfusion (thereby reducing alveolar dead space) or by reducing pulmonary vascular resistance and magnifying intrapulmonary shunt by countering hypoxic pulmonary vasoconstriction.58
Mechanical factors can cause either inconsistencies or inaccuracies in PETCO2. The sample tubing length and aspirating flow rates used in sidestream capnometers affect the time required to measure changes in tidal CO2 concentration.66 At respiratory frequencies above 30, capnometers tend to underreport the true PETCO2.67 This may occur because of gas mixing between adjacent breaths during transport down the sampling line and in the analysis chamber.67 This problem can be avoided with mainstream analyzers, which provide near-instantaneous CO2 measurement (<250 msec).68
PaCO2-PETCO2 Gradient, Positive End-Expiratory Pressure, and Lung Recruitment
PEEP recruits collapsed alveoli, improves ventilation-perfusion matching, and reduces alveolar dead space, although excessive levels cause overdistention and increased alveolar dead space.69 Because the PaCO2-PETCO2 gradient correlates strongly with the physiologic dead space–to–tidal volume ratio (VD/VT), it may be useful in titrating PEEP in patients with acute lung injury (ALI) or acute respiratory distress syndrome (ARDS).49,50 An animal model of ARDS found that the stepwise application of PEEP progressively reduced the PaCO2-PETCO2 gradient and coincided with maximal or near-maximal improvements in oxygenation.61 However, PEEP applied beyond the lowest PaCO2-PETCO2 gradient caused a secondary rise in the gradient, along with decreased cardiac output. Although a subsequent trial was unable to reproduce these findings in humans, another study found that the PaCO2-PETCO2 gradient narrowed (14 to 8 mm Hg) and oxygenation improved when PEEP was set at the lower inflection point of the pressure-volume curve.45,62 When PEEP was set 5 cm H2O above the lower inflection point, the PaCO2-PETCO2 gradient rose to 11 mm Hg, and cardiac output trended downward. In patients without a lower inflection point, the PaCO2-PETCO2 gradient did not change in response to PEEP. Thus, in a subset of ARDS patients, the PaCO2-PETCO2 gradient may be an effective way to titrate PEEP.

Full access? Get Clinical Tree