Overview of Cardiac Arrest
Cardiac disease is the most common cause of death in the United States, with estimates ranging between 300,000 and 500,000 deaths annually. The American Heart Association (AHA) estimates that there are approximately 295,000 out-of-hospital cardiac arrests each year. As few as one fourth of these patients will have an attempted resuscitation. Only 3–8% of prehospital arrests will survive to discharge and have a reasonable functional recovery. Sudden cardiac death is often associated with an underlying history of coronary artery disease, which is seen in 80% of patients. Other causes include massive pulmonary embolism, renal failure, hypoglycemia, thyrotoxicosis, trauma, illicit drugs, and medications. The most common rhythms associated with cardiac arrest are ventricular arrhythmias (ventricular fibrillation [VF] and ventricular tachycardia [VT]). Asystole and pulseless electrical activity (PEA) are the next most common rhythms, at the time of first intervention.
The two most important factors for survival in the undifferentiated adult cardiac arrest victim are minimizing the elapsed time from patient collapse and the onset of effective cardiopulmonary resuscitation (CPR) and rapid defibrillation. Unfortunately, as many as 85% of arrests occur at home and not in a public place where there may be access to a defibrillator. Studies with patients in VF have demonstrated that for every minute that passes without intervention, the odds of survival decreases by 7–10% (decreased to 3–4% with effective CPR). Other factors related to a positive outcome include witnessed cardiac arrest and early use of advanced life support (ALS). Factors associated with poor prognosis include dyspnea as the presenting complaint, malignancy or sepsis as the underlying cause of cardiac arrest, coexistence of pneumonia, prolonged anoxia, presence of hypotension prior to cardiac arrest, and increasing age.
A patient who is not successfully resuscitated in the field is unlikely to be resuscitated in the emergency department. The risks of transporting a patient who remains in cardiac arrest after ALS procedures have been performed in the field may outweigh the likelihood of a successful resuscitation with good neurologic outcome. Medical directors should consider protocols to determine death and termination of resuscitative efforts in the field.
A resuscitation team has many pivotal participants in a cardiac arrest: the first responder, emergency medical service (EMS) personnel, the emergency department resuscitation team leader, emergency department resuscitation team members, and ancillary personnel. A successful resuscitation depends on a functional team. The responsibilities and expectations for each member must be identified prior to a resuscitation. Attempting to assign these roles after a resuscitation has already begun will simply add confusion to an already chaotic situation.
The composition of the resuscitation team is based largely on resource availability and institutional preferences. There must be a team leader who is responsible for the overall direction of the resuscitation. One member of the team is responsible for airway management. Another member will be necessary to provide support for this function, such as applying cricoid pressure, suctioning, or assisting in bag ventilation. Multiple team members may be required to provide chest compressions. The team leader must ensure that these providers do not become fatigued, by rotating the team members every 5 minutes. Vascular access must be obtained, and the team member performing this role can also administer medications. If a medication dispenser (eg, Pyxis) is being used, it is helpful to designate one person to manage it. Finally, it is helpful to have a recorder to record events, provide cues, track laboratory results, and communicate with areas outside of the resuscitation area. It is also important that the team leader control the number of people in the resuscitation area. Those individuals who are not part of the resuscitation may distract other members of the team.
Care providers are often trained as individuals, even though they most often respond as an integrated team. Utilization of team behaviors can minimize the number of errors, duplication of efforts, and loss of information that can occur during a resuscitation. Maintaining situational awareness is the key to being an essential team member. Reinforcing situational awareness in others emphasizes the team construct. Some mechanisms to enhance cross-monitoring include call outs and check backs. Call outs involve information that must be shared with the entire team (eg, calling out vital signs). Check backs are means to avoid order errors—the recipient of the order repeats the order verbatim, and then the orderer confirms that order verbatim. These techniques sustain dynamic situational awareness and allow for an organized, integrated team approach to comprehensive resuscitative care. Many universities and other institutions now have simulation centers that can be utilized to more effectively train health care providers for resuscitations in realistic settings, both as individuals and in team settings.
To allow family members to be present during a resuscitation or invasive procedure has been a subject of great debate. The majority of family members who have been surveyed indicate they would like to be present at the resuscitation. This is true for both adult and pediatric patient populations. The families often state that by being present they are able to provide emotional and spiritual support. The family’s presence may also provide closure and facilitate grieving. Opponents of family presence argue that there may be disruption of code team functions and the event may cause lasting psychological damage to the witnessing family members. Neither of these concerns has been supported by the literature.
Adult Basic Life Support
The AHA first proposed the phrase “the chain of survival” to describe the interrelated series of interventions that must be in place to maximize functional survival from sudden cardiac death. Any failure to implement a single link in the chain will lead to a decrease in survival. As depicted by the AHA, there are four links in the chain of survival: rapid access to medical care, early basic life support (BLS), early defibrillation, and early advanced cardiac life support (ACLS). Since that time, efforts have been made to expand this chain to include prevention prior to the event and secondary prevention of cardiac arrest. This includes lifestyle modifications (see below) and medical interventions such as statins for hypercholesterolemia, better control of diabetes, and the placement of implantable cardioverter defibrillators.
As most cardiac arrests occur in the absence of trained medical personnel, it is imperative that we identify those patients at risk and decrease the likelihood of a cardiac event. Early prevention involves both primary prevention, including lifestyle modification (exercise and smoking cessation), and secondary prevention, including medical therapy. In addition, the patient and family should be educated on the signs and symptoms of chest pain related to cardiac ischemia. Patients with known cardiac disease should attempt to treat the pain with sublingual nitroglycerin. If, after taking the nitroglycerin, there is no relief, the patient should call the emergency number for his or her area. Patients without known disease should contact the emergency number if unremitting chest pain is present for more than 5 minutes. In the hospital setting, an early, organized response to chest pain, dyspnea, and abnormal vital signs can decrease the number of cardiac arrests.
As previously discussed, the need for immediate CPR and defibrillation following cardiac arrest cannot be overstated. On finding the unresponsive patient, a lone rescuer should immediately activate the EMS system and if available obtain an automated external defibrillator (AED). They should then provide adequate CPR. If two or more rescuers are present, CPR should be initiated immediately by one while the other activates EMS. As opposed to a lay provider, a lone health care worker may alter this sequence. If the event is likely asphyxial in origin, the provider may give five cycles of CPR before activating EMS. In the hospital setting, initiate the hospital’s emergency response or “code” system. Early access into the system is imperative to minimize the time delay until defibrillation.
On finding an unresponsive patient and activating the EMS system, return to the patient to provide BLS until further help arrives. Assume a position alongside the patient’s thorax so that rescue breathing and chest compressions can be done without repositioning one’s body. Position the patient on a hard surface to allow for efficient chest compressions. Anticipate the arrival of a defibrillator, which is usually positioned on the left side, next to the patient’s ear. Remember the importance of provider safety. If the provider is injured, it will obviously impair his or her ability to provide BLS and will add further strain to limited EMS resources.
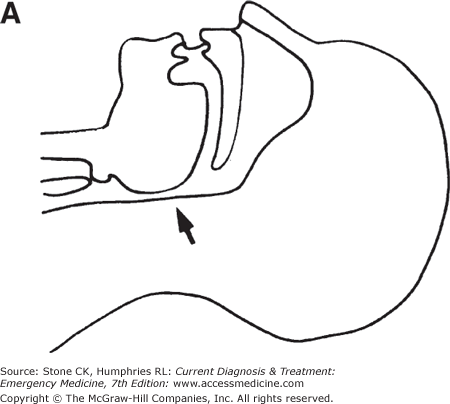
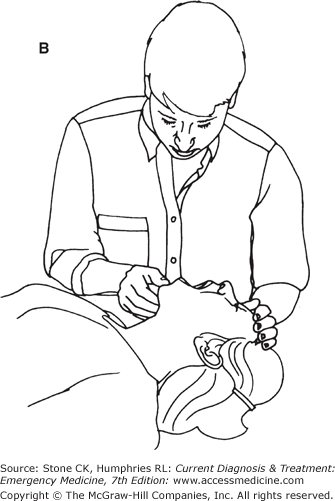
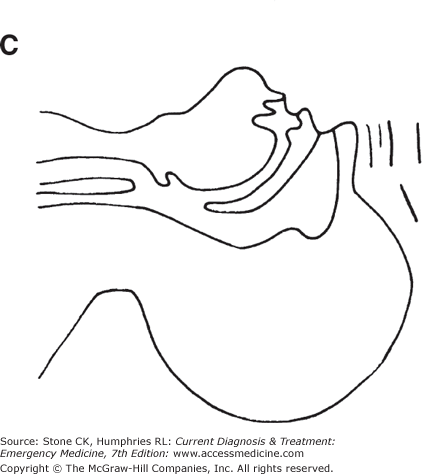
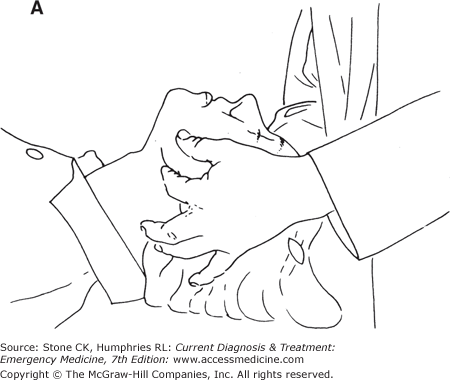
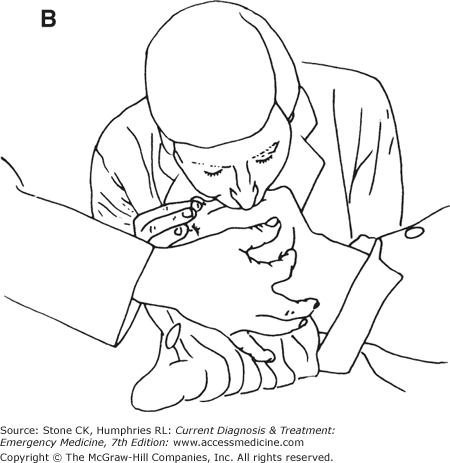
The first step of BLS is opening the patient’s airway. This may be achieved using either the head tilt–chin lift or the jaw-thrust method. It is recommended that lay rescuers use the head tilt–chin lift method due to concern that the jaw thrust is more difficult to perform and may not be as effective in opening the airway. To perform the head tilt–chin lift, place one hand firmly on the patient’s forehead and apply firm downward, backward pressure to tilt the head. Hook the fingers of the other hand under the bony part of the chin, lifting up the chin (Figure 9–1). If a health care provider is the rescuer and suspects C-spine injury, the jaw thrust is the method of choice to reduce movement of the neck. This maneuver is performed by using the index and middle fingers to grasp the angles of the mandible and lifting with both hands. The head is maintained in neutral position (Figure 9–2).
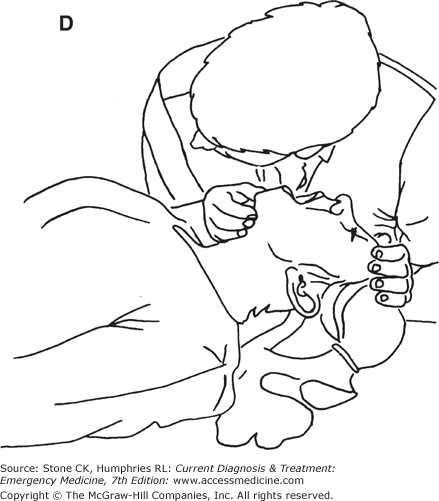
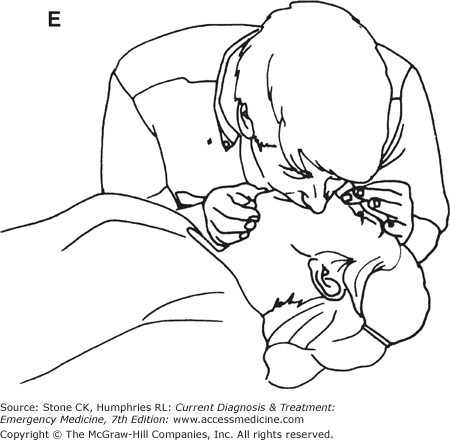
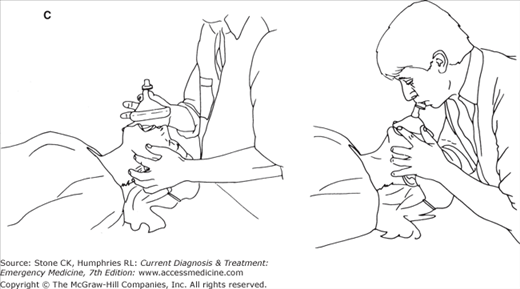
Figure 9–1.
Opening the Airway and Providing Ventilation. A: Obstruction of airway by posterior displacement of tongue (arrow) in resting, supine position. B and C: Relief of lingual airway obstruction in supine position by forward displacement of mandible (head tilt–chin lift method). D: Rescuer checks for spontaneous breathing by listening and feeling for exhaled air while looking for chest movement. E: Mouth-to-mouth ventilation. While maintaining head tilt–chin lift, the rescuer uses his or her fingers to seal the victim’s nose shut; rescuer takes a deep breath, seals mouth over victim’s mouth, and exhales, watching for chest movement. Look, listen, and feel for passive exhalation.
After opening the patient’s airway, breathing is assessed. This is done by leaning over the patient’s open mouth and looking down at the chest for any rise or fall of breathing. Place an ear near the patient’s mouth, listening for breathing or feeling the flow of air over the cheek. This should take no more than 10 seconds. In the absence of adequate breathing (agonal respirations are inadequate), perform mouth-to-mouth, mouth-to-mask, or bag–mask ventilation. Health care professionals should be familiar with all of these techniques. A mask with a one-way valve should be readily available in all health care settings to minimize the risk of contamination from the patient’s oral secretions. A bag–mask should be available in all critical care areas and on crash carts.
Maintain the airway by using the head tilt–chin lift method. Pinch the patient’s nose shut. Seal your lips around the patient’s mouth. Give two slow breaths over 2 seconds initially. There should be good chest rise and fall. If not, reposition the patient’s airway and attempt to ventilate again. If there is still no movement of air, presume that the patient has a foreign body airway obstruction (FBAO) and attempt to clear it (see below).
A clear mask with or without a one-way valve (often called a pocket mask) can be used as an adjunct to mouth-to-mouth ventilation. Ventilations are provided in the same way as for mouth to mouth. It is often easier and more effective for the inexperienced provider to adequately ventilate the patient with the pocket mask than with the bag–mask. When possible, the mask should be attached to supplemental oxygen. There are two techniques to achieve an effective seal with the mask.
Used when there is more than one provider. The provider ventilating the patient is positioned at the head of the bed. The mask is applied in one of the following two ways: with the thumbs and thenar eminences providing a seal, while the fingers are used to perform jaw thrust, or with the thumbs and index fingers providing a seal, while the remaining fingers provide a jaw thrust.
Used when there is only one provider, the lateral technique allows the provider to perform one-person CPR. With the provider at the patient’s side, a head tilt–chin lift is applied. The hand closer to the top of the patient’s head performs a head tilt while creating a seal on the upper part of the mask with index finger and thumb. The lower hand performs a chin lift with the fingers while creating a seal on the lower part of the mask with the thumb and thenar eminence.
When two providers are available to manage the patient’s airway, the mask is applied as with the cephalic technique of the pocket mask. Ventilations are then administered by the second provider squeezing the bag over 2 seconds and then releasing for 3 seconds. If only one provider is available for airway management, he or she must provide an adequate seal with one hand, using the index finger and thumb while providing a chin lift with the other three fingers. The other hand is used to squeeze the bag–mask. Optimizing the head tilt by positioning towels underneath the patient’s shoulders may help, especially if the patient is obese. Ventilation can be improved by squeezing the bag against the provider’s body. Whenever possible, use supplemental oxygen to provide up to a 100% concentration.
Cricoid pressure (Sellick maneuver) is the posterior displacement of the cricoid cartilage to close off the esophagus. This minimizes gastric insufflation associated with ventilation, as well as preventing reflux of gastric contents into the upper airway and lungs. This should be done only in the unconscious patient. The cricoid cartilage is found by first locating the thyroid cartilage with the index finger and then moving down the neck over the cricothyroid membrane. The first cartilage ring below the membrane is the cricoid cartilage. Moderate pressure (5–10 lb) is applied, pressing the cartilage with the thumb and index finger posteriorly toward the cervical spine.
Circulation is assessed by palpation of the carotid pulse. The pulse is located in the groove lateral to the trachea. Check the pulse for no more than 10 seconds. If a pulse is present, rescue breathing can continue with one breath every 5–6 seconds. If a pulse is absent, start chest compressions. This is essential for providing blood flow during CPR. To perform chest compressions, identify the lower sternum in the center of the chest, between the nipples. The heel of the hand should be in this position, and place the second hand over the first so that they are overlapped and parallel. Compressions should depress the sternum 1.5–2.0 in, and then allow the chest to return to normal position. Chest recoil allows venous return to the heart. Compressions are given at 100/min. The compression–ventilation ratio in adults should be 30:2, for both single rescuer and dual rescuer CPR. This results in minimal interruption of compressions and blood flow. Once a definitive airway is established, ventilations and compressions can be performed asynchronously.
Recent recommendations published by the AHA recommend lay rescuers (non-health care providers) provide chest compression only CPR. This stems from research showing no survival advantage from ventilations during bystander-provided CPR compared to chest compressions only. Additionally, without interruptions to chest compressions, more blood flow is delivered to vital organs, and mouth-to-mouth resuscitation is thought to be one of the major psychological obstacles to would-be rescuers during a bystander-witnessed arrest.
While uncommon, FBAO is a preventable cause of death. Identifying a patient with an FBAO may be as simple as recognizing the conscious patient with difficulty breathing, coughing, or the universal “I’m choking” sign, with fingers clutching around the throat, but it can be much more difficult to detect in the unconscious/altered level of consciousness patient. In the conscious patient, ask if he or she is choking. If the patient has a strong cough, is not cyanotic, does not have labored breathing or retractions, and can speak, then a partial obstruction with good air exchange exists. Observe the patient, but do not intervene initially. Allow the patient to attempt to clear the obstruction by himself or herself. If the patient has a weak cough, is cyanotic, has labored breathing, stridor, or has difficulty speaking, then a partial obstruction with poor air exchange exists. Prompt intervention is indicated. If the airway is obstructed completely, the patient is unable to speak or cough and may become cyanotic. Rapid intervention is essential.
The abdominal thrust (Heimlich maneuver) is used in the conscious choking patient. While standing behind the patient, position the fist with the thumb facing up over the umbilicus. Roll the fist so that the thumb is against the abdominal wall. Grasp the fist with the other hand. Apply sharp upward thrusts until the foreign body is cleared or the patient collapses and becomes unconscious. In the unconscious patient, position him or her on the floor. Perform a tongue–jaw lift by grasping the jaw and tongue with one hand and observe the airway. If a solid obstruction is visually identified, use the other hand to perform a finger sweep. Attempt to ventilate. If the first attempt does not succeed, reposition the airway and attempt to ventilate again. If the second attempt fails, perform the Heimlich maneuver by straddling the patient. Place the heel of one hand in the same location as that used for the standing abdominal thrust. Place the other hand over the top of the first. Provide five sharp upward thrusts. Repeat the sequence until the obstruction is relieved or alternative means of establishing the airway are available (eg, Magill forceps, surgical or needle cricothyroidotomy).