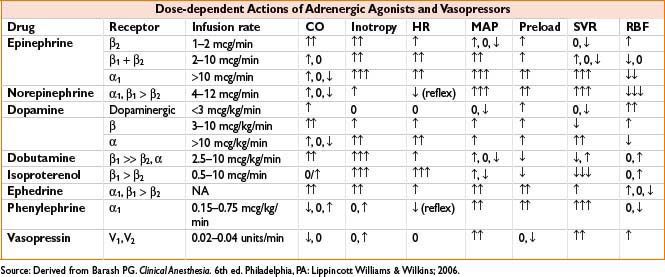
ADRENERGIC AGONISTS
General comments: Act on α, β, or dopaminergic receptors (see the table below). May cause tachycardia, hypertension, arrhythmias, myocardial ischemia, and tissue necrosis with extravasation (administer centrally, treat with phentolamine infiltration). Ensure adequate circulating volume; do not use vasopressors for treatment of hypovolemia.
Dobutamine (Dobutrex)
Indications: Heart failure
Dose: Infusion prep: 500 mg in 250 mL D5W or NS = 2,000 mcg/mL (2 mg/mL) Adult: 2 mcg/kg/min, titrate 2–20 mcg/kg/min, max 40 mcg/kg/min; Peds: 5–20 mcg/kg/min
Onset: 12 min
Duration: <10 min
Mechanism: Predominantly β1-adrenergic agonist
Clearance: Hepatic metabolism, renal excretion
Comments: Strong inotrope, ↓ SVR in lower doses. BP effect is dependent on preload (volume status) and presence of “recruitable” inotropy (used for stress echo). Useful in CHF and MI with low-output state; ↓ tachyarrhythmias than dopamine. Can increase ventricular rate in atrial fibrillation. May develop tolerance after 3 d. Do not mix with sodium bicarbonate.
Dopamine (Intropin)
Indications: Hypotension, acute heart failure
Dose: Infusion prep: 400 mg in 250 mL D5W = 1,600 mcg/mL; low dose 2–5 mcg/kg/min, medium dose 5–15 mcg/kg/min, high dose 20–50 mcg/kg/min
Mechanism: Dose-dependent differential dopaminergic, α- and β-adrenergic agonist
Clearance: Monoamine oxidase (MAO)/catechol-O-methyltransferase (COMT) metabolism
Onset: 5 min
Duration: 10 min
Comments: Contraindicated in pheochromocytoma or ventricular fibrillation, caution with peripheral artery disease. Improved renal blood flow/GFR at lower doses but does not prevent renal dysfunction or death (Ann Intern Med. 2005 Apr 5;142(7):510–24). β activity predominates at doses 3–10 mcg/kg/min and mixed α- and β-adrenergic effects at ≥10 mcg/kg/min, although traditional dose–response effects not strongly reproducible. Do not mix with sodium bicarbonate.
Ephedrine (Generic)
Indications: Short-term treatment of hypotension, e.g., after induction in patient with normal catecholamine stores.
Dose: Bolus only
Adult: 5–10 mg IV PRN, typically to max 50 mg or 0.1 mg/kg; 25–50 mg SC/IM q4–6h prn. Peds: 0.2–0.3 mg/kg/dose
Mechanism: Indirect α- and β-adrenergic stimulation via norepinephrine release at sympathetic nerve endings.
Clearance: Mostly renal elimination (unchanged)
Duration: 3–10 min
Comments: Increases blood pressure by ↑ cardiac output, peripheral vasoconstriction. Tachyphylaxis with repeat dosing due to norepinephrine depletion. May cause CNS stimulation, decrease in uterine activity, and mild bronchodilation. Avoid in patients taking MAO inhibitors, closed-angle glaucoma.
Epinephrine (Adrenaline)
Indications: (1) Cardiac arrest, (2) bronchospasm, anaphylaxis, (3) heart failure, hypotension; (4) severe bradycardia
Dose: Infusion prep: 4 mg in 250 mL D5W or NS = 16 mcg/mL
Adult: (1) 1 mg IV/IO q3–5min during resuscitation, if no IV/IO consider endotracheal dose of 2 mg; infuse 0.1–0.5 mcg/kg/min for post-arrest care; (2) 0.1–0.5 mg SC q10–15min, or 0.3 mg IM (1:1,000), or 0.1–0.25 mg IV slow bolus; (3) 5–10 mcg bolus; 0.02–0.3 mcg/kg/min; (4) bolus 10–20 mcg IV; infuse 1–4 mcg/min IV Peds: (1) 1st dose 0.01 mg/kg IV/IO; subsequent doses 0.1–0.2 mg/kg IV/IO q3–5min; intratracheal: 0.1 mg/kg of 1:10,000 solution; (2) 0.01 mcg/kg SC (1:1,000 aqueous) q15min to q4h prn; for anaphylaxis give 0.01 mcg/kg q15min × 2 doses then q4h prn; (3) 0.1–1 mcg/kg/min, max 1.5 mcg/kg/min; (4) 0.01 mg/kg IV/IO or 0.1 mg/kg via ETT
Neonates: (1) 0.01–0.03 mg/kg IV/IO q3–5min; intratracheal: 0.1 mg/kg of 1:10,000 solution
Mechanism: α1- and nonselective β-adrenergic agonist
Clearance: MAO/COMT metabolism
Duration: 5–10 min
Comments: β-adrenergic effects predominate at lower doses (may cause paradoxical hypotension), ↑ in relative α1 at higher doses. Cardiac dysrhythmias common, potentiated by halothane. May cause ↑ lipolysis, glycogenolysis, pulmonary edema, lactate, and hyperglycemia due to inhibition of insulin release. Reduces splanchnic circulation; high/prolonged doses may have cardiotoxic effect. Reserve 1 mg IV bolus for cardiac arrest to avoid significant hypertensive response.
Isoproterenol (Isuprel)
Indications: Indicated for heart block, shock, bronchospasm during anesthesia. Also used for ventricular arrhythmias with AV block, β-blocker overdose, 3rd degree AV block awaiting pacemaker. No longer recommended for cardiac arrest.
Dose: Infusion prep 1 mg in 250 mL = 4 mcg/mL
Adult: AV nodal block: 5 mcg/min IV titrate up to 20 mcg/min (not weigh based); Shock: 0.5–5 μg/min IV. Peds: Start 0.02–0.1 mcg/kg/min; titrate to effect 0.05–2 mcg/kg/min
Mechanism: Nonselective β-adrenergic agonist
Clearance: Hepatic and pulmonary metabolism via MAO/COMT; 40–50% renal excretion (unchanged)
Duration: 8–50 min
Comments: Potent positive chronotrope and inotrope; systemic > pulmonary vasodilation. Increases myocardial O2 demand; causes less hyperglycemia than epinephrine. Useful in cardiac failure with bradycardia or asthma; caution in shock due to redistribution of perfusion to nonessential areas. Avoid in digitalis intoxication, preexisting tachyarrhythmias; caution with MAOI/tricyclics. May cause hypotension with large doses, CNS excitation, pulmonary edema, dysrhythmias.
Phenylephrine (Neosynephrine)
Indication: Hypotension. Also used for SVT, tetralogy of Fallot “spells,” hypotension induced by neuraxial block, outflow tract obstruction in obstructive hypertrophic cardiomyopathy.
Dose: Bolus: 50–100 mcg IV; 2–3 mg SC/IM q1–2h; infusion prep 40 mg in 250 mL = 160 mcg/mL; infuse 0.2–1 mcg/kg/min or 20–180 mcg/min. Peds: Bolus 0.5–10 mcg/kg IV infuse 0.1–0.5 mcg/kg/min
Mechanism: Potent direct α1-adrenergic agonist
Duration: <5 min
Clearance: Hepatic and intestinal wall metabolism; renal elimination
Comments: Produces venous and arterial vasoconstriction, variable effect on CO (depends on preload/afterload and cause of hypotension). Bolus used for correction of sudden severe hypotension. May cause reflex bradycardia, microcirculatory constriction, uterine contraction or vasoconstriction, ↓ cardiac output in ischemic heart disease. Caution with MAOI/tricyclics; contraindicated in closed-angle glaucoma.
Norepinephrine (Levarterenol, Levophed)
Indications: Hypotension, especially in septic shock
Dose: Infusion prep 4 mg in 250 mL NS or D5W = 16 mcg/mL; Adult: Infuse 0.02–0.3 mcg/kg/min = 20–300 ng/kg/min or 4–12 mcg/min; Peds: 0.05–0.1 mcg/kg/min to max 2 mcg/kg/min
Mechanism: Synthetic preparation of naturally occurring neurotransmitter; precursor to epinephrine. Potent α-adrenergic, modest β-adrenergic agonist. Relative α-potency ↑ with doses >4–5 mcg/min.
Onset: 1–2 min
Duration: 1–2 min
Clearance: MAO/COMT metabolism
Comments: Peripheral vasoconstriction, ↑ systolic, diastolic, pulse pressure; positive inotropy; coronary vasodilation; minimal chronotropic effect; variable effect on splanchnic perfusion. May cause ↑ uterine contractility, constricted microcirculation, arrhythmias (especially with hypoxia, hypercarbia). First-line in septic shock (ensure adequate blood volume); avoid in ischemic cardiogenic shock due to ↓ myocardial O2 economy. Prolonged infusion may have cardiotoxic effect. Use extreme caution in MAOI/tricyclic antidepressants.
Vasopressin (Antidiuretic Hormone [ADH], Pitressin)
Indications: (1) Diabetes insipidus, abdominal distension, (2) vasodilatory/catecholamine-resistant shock, upper GI hemorrhage, (3) pulseless ventricular tachycardia or ventricular fibrillation
Dose: Infusion prep 100 units in 100 mL NS = 1 unit/mL
Adult: (1) 5–10 units IM/SC or intranasal q6–12h prn; (2) 0.02–0.04 units/min IV infusion; (3) 40 unit IV/IO/ET bolus (single dose)
Mechanism: Synthetic analogue of endogenous ADH; V1 receptors: Smooth muscle constriction; vasoconstriction of splanchnic, coronary, muscular, and cutaneous vasculature; V2 receptors: ↑ urine osmolality, ↓ urine volume
Clearance: Hepatic and renal metabolism; renal elimination
Duration: 10–20 min
Comments: Potential intestinal or skin ischemia. May cause oliguria, water intoxication, pulmonary edema; abdominal cramps (from ↑ peristalsis); anaphylaxis; contraction of gallbladder, urinary bladder, or uterus; vertigo or nausea. Patients with coronary artery disease are often treated with concurrent nitroglycerin. Do not abruptly discontinue IV infusion.
PHOSPHODIESTERASE INHIBITORS
General Comments: Improve myocardial contractility due to ↑ cyclic adenosine monophosphate, calcium flux, and calcium sensitivity of contractile proteins; cause systemic and pulmonary vasodilation. Inotropic effect does not rely on β-adrenergic stimulation and therefore not affected by β-blockade/downregulation.
Amrinone (Inocor, Inamrinone)
Indications: Indicated for tx of low cardiac output states, heart failure, and as adjunct in pulmonary hypertension.
Dose: Adult/Peds: Load 0.75 mg/kg IV bolus over 2–3 min, then infuse 5–15 mcg/kg/min. Infusion prep 100 mg in 250 mL in crystalloid without dextrose = 0.4 mg/mL; max dose: 10 mg/kg/24 hrs. Neonates: Load 0.75 mg/kg IV bolus over 2–3 min, then infuse 3–5 mcg/kg/min
Onset: Immediate (peak at 5 min)
Duration: 0.5–2 hrs, 8 hrs with multiple doses
Mechanism: Inhibits myocardial cAMP phosphodiesterase (PDE III)
Clearance: Variable hepatic metabolism; renal/fecal excretion. Reduce dose 50–75% in ESRD
Comments: Mild inotropy with strong vasodilation. May cause hypotension, thrombocytopenia (long-term use), and anaphylaxis (contains sulfites).
Milrinone (Primacor)
Indications: Indicated for congestive heart failure
Dose: Infusion prep 20 mg in 100 mL = 200 mcg/mL. Adult: Load: 50–75 mcg/kg IV over 10 min; infusion: 0.375–0.75 mcg/kg/min titrate to effect. Peds: Load: 50 mcg/kg IV over 10 min, followed by infusion of 0.5–1 mcg/kg/min and titrate to effect
Onset: 5–15 min
Duration: 3–5 hrs
Mechanism: Inhibits myocardial cAMP phosphodiesterase (PDE III)
Clearance: Renal excretion (83%), hepatic metabolism (12%)
Comments: Amrinone derivative with 20 × inotropic potency. May ↑ arrhythmias, outflow tract obstruction in IHSS. Associated with hypotension (caution with load), headaches. Not recommended for acute MI. May improve diastolic relaxation (lusitropy).
ADRENERGIC ANTAGONISTS
α-blockers
General comments: Cause peripheral vasodilation, used in treatment of hypertension, pheochromocytoma, hypertrophic prostate. Associated with orthostatic and ↑ hypovolemic hypotension; treat overdoses with norepinephrine, not epinephrine (“epinephrine reversal” with ↑↑ hypotension due to unopposed β activity).
Phenoxybenzamine (Dibenzyline)
Indications: Preoperative “chemical sympathectomy” in pheochromocytoma
Dose: Adult: 10–40 mg/d PO (start at 10 mg/d and increase by 10 mg/d q4d prn). Usual dose 20–40 mg bid–tid. Peds: 0.2 mg/kg PO qd, max 10 mg; increase by 0.2 mg/kg to typical maintenance of 0.4–1.2 mg/kg/d q6–8h
Onset: Several hours
Duration: Several days
Mechanism: Nonselective, noncompetitive, irreversible α-blockade; α1 >> α2
Clearance: Hepatic metabolism, renal/biliary excretion
Comments: Long duration of action (may require ↑↑ doses of vasopressors after pheochromocytoma resection). May cause severe orthostatic hypotension and reflex tachycardia. Use largely replaced by phentolamine.
Phentolamine (Regitine, OraVerse)
Indications: (1) Hypertension from catecholamine excess in pheochromocytoma; (2) α-adrenergic drug extravasation. Also used for reversal of soft-tissue local (dental) anesthesia.
Dose: Adult: (1) 1–5 mg IV (5 mg for diagnosis); may be used as infusion during resection (2) 5–10 mg in 10 mL of NS infiltrated into affected area; Peds: (1) 0.05–0.1 mg/kg/dose IV/IM 1–2 hrs preprocedure q2–4h to max 5 mg; (0.05–0.1 mg/kg/dose IV/IM × 1 for diagnostic purposes); (2) 0.1–0.2 mg/kg diluted in 10 mL NS infiltrated into area of extravasation
Onset: 2 min (IV)
Duration: 10–15 min (IV)
Mechanism: Nonselective, competitive α-antagonist; relaxation of vascular smooth muscle
Clearance: Unknown metabolism, 13% excreted unchanged in urine
Comments: May cause marked hypotension, reflex tachycardia, cerebrovascular spasm, dysrhythmias, diarrhea.
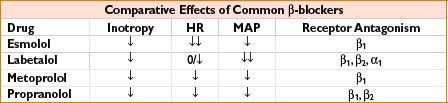
β-BLOCKERS
General comments: Common in perioperative practice, do not hold home dose for surgery. Perioperative use (titration to HR 60–70, avoid hypotension) may ↓ MI in high-risk patients; use of fixed doses for MI prevention associated with ↑ stroke (Circulation 2009;120(21):2123–2151.). Wide range of indications including HTN, arrhythmias, ischemic heart disease, chronic CHF, migraine prophylaxis. Vary in duration of action and receptor selectivity. May cause bradycardia, AV conduction delays, hypotension, bronchospasm; may mask symptoms of hypoglycemia. Contraindicated in uncompensated CHF, cardiogenic shock, severe bradycardia, heart block > first degree; caution in COPD/asthma. Abrupt withdrawal can precipitate rebound angina.
Labetalol (Normodyne, Trandate)
Indications: Hypertension, angina
Dose: Adult: IV: 5–20 mg increments or 1–2 mg/kg at 5–10 min intervals, to 40–80 mg/dose. Max total 300 mg; 200–400 mg PO q12h. Infusion: 2–150 mg/hr, or 0.05 mcg/kg/min, titrate to effect. Peds: 0.12–1 mg/kg/dose q10min PRN to max 10 mg/dose, infusion 0.4–1 mg/kg/hr, max 3 mg/kg/hr
Mechanism: Selective α1-adrenergic blockade with nonselective β-adrenergic blockade. Ratio of α/β-blockade 1:7 (IV), 1:3 (PO)
Clearance: Hepatic metabolism; renal elimination
Onset: 1–2 min
Duration: 2–8 hrs
Comments: Mixed antagonism unique among common IV drugs. Effective ↓ systemic blood pressure without reflex tachycardia. May cause orthostatic hypotension, skin tingling. Crosses placenta, no effect on uterine blood flow. Avoid in CHF.
Metoprolol (Lopressor, Toprol XL extended release)
Indications: Indicated for hypertension, acute MI, angina, stable CHF. Also used in tachyarrhythmias, hypertrophic cardiomyopathy, hyperthyroid.
Dose: 2.5–5 mg IV boluses q2min, prn, up to 15 mg. 50–200 mg PO q8–24h
Onset: IV 1–5 min (peak at 20 min)
Duration: 5–8 hrs, dose dependent
Mechanism: β1-adrenergic blockade (β2-adrenergic antagonism at high doses)
Clearance: Hepatic metabolism (CYP2D6, absent in 8% Caucasians), renal elimination
Comments: May cause clinically significant bronchoconstriction (with doses >100 mg/d), dizziness, fatigue, insomnia. Crosses the placenta and blood–brain barrier.
Esmolol (Brevibloc)
Indications: (1) Supraventricular tachycardia, (2) intraoperative tachycardia and/or hypertension
Dose: Infusion prep 2,500 mg in 250 mL = 10 mg/mL; rate 25–300 mcg/kg/min. Adult: Immediate control: 80 mg (∼1 mg/kg) over 30 sec followed by 150 mcg/kg/min. Gradual control: 0.5 mg/kg load over 1 min followed by 50 mcg/kg/min; repeat load (max 3 doses) and titrate infusion q4min. Peds: Load 0.1–0.5 mg/kg IV over 1 min; infusion start at 50 mcg/kg/min, titrate to effect, max 300 mcg/kg/min
Onset: 1 min
Duration: 10–30 min after infusion
Mechanism: Selective β1-blockade
Clearance: Degraded by RBC esterases; renal elimination of acid metabolite
Comments: Ultrashort acting, blunts response to intubation, may decrease seizures in ECT
Propranolol (Inderal)
Indications: Hypertension, angina, migraine prophylaxis, pheochromocytoma, hypertrophic subaortic stenosis, supraventricular arrhythmia, portal hypertension, tremor. Also used for esophageal varices, tetralogy of Fallot cyanotic spells, thyrotoxicosis.
Dose: Adult: Test dose of 0.25–0.5 mg IV, then titrate up by 0.5 mg/min to effect. PO: 10–40 mg q6–8h, prn; 1–3 mg slow IV; 1 mg/dose IV q5min to max 5 mg. Peds: 0.15–0.25 mg/kg/d slow IV, repeat prn; 0.01–0.1 mg/kg slow IV
Onset: 2–10 min
Duration: 6–10 hrs
Mechanism: Nonspecific β-adrenergic blockade
Clearance: Hepatic metabolism; renal elimination
Comments: Effective dose highly variable. Membrane stabilizing/antiarrhythmic effect at ↑ doses. Crosses placenta and blood–brain barrier. Shifts oxyhemoglobin dissociation curve to the right.
α AGONISTS
Clonidine (Catapres)
Indications: Hypertension. Multiple other uses including opiate and nicotine withdrawal, potentiation of local anesthetic analgesic effect.
Dose: 5–25 mcg/kg/d PO div q6h. Start: 5–10 mcg/kg/d div q6h; max: 0.9 mg/d; info: increase gradually q5–7d; transdermal: 1 patch/wk. Start: 0.1 mg/24 hrs patch, titrate q1–2wk; max: 0.6 mg/24 hrs (using two 0.3 mg/24 hr patches). Info: If switching from PO, continue PO × 1–2 d
Onset: 30–60 min (PO), 2–3 d (transdermal)
Duration: 8 hrs (single PO dose)
Mechanism: α2-adrenergic agonist (↓ central sympathetic outflow)
Clearance: Hepatic metabolism; excretion renal 65%, biliary 20%
Comments: May cause rebound hypertension (18–72 hrs after discontinuation), dry mouth, drowsiness, dizziness, constipation, sedation, weakness.
Methyldopa (Aldomet)
Indications: Hypertension; used for hypertension in pregnancy
Dose: 250–500 mg PO bid (increase q2d prn; max 3 g/d); 250–1,000 mg IV infused over 30–60 min q6h (max 4 g/d)
Onset: 3–6 hrs (PO), 4–6 hrs (IV)
Duration: 12–24 hrs (PO), 10–16 hrs (IV)
Mechanism: Stimulates α2-adrenergic receptors (centrally acting antihypertensive) via active metabolites
Clearance: Metabolized by central adrenergic neurons and liver; primarily urine excretion
Comments: Other agents preferred due to slow onset; causes Na/H2O retention, avoid in liver and end-stage renal disease, pheochromocytoma.
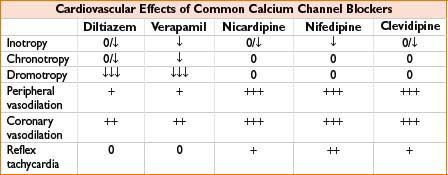
CALCIUM CHANNEL BLOCKERS (CCB)
General comments: Produce varying degrees of coronary and systemic vasodilation, ↓ HR (chronotropy), ↓ myocardial contractility (inotropy), ↓ cardiac conduction velocity (dromotropy). Coadministration with β- blockade ↑ risk of heart block. Contraindicated in sick sinus syndrome, 2nd or 3rd degree AV block (unless with functioning pacemaker).
Diltiazem (Cardizem)
Indications: Supraventricular tachycardia, atrial fibrillation/flutter, angina
Dose: Infusion prep 100 mg in 100 mL = 1 mg/mL; load 2.5–25 mg (or 0.25 mg/kg) over 2 min, may rebolus 0.35 mg/kg in 15 min if no effect; infuse 2–15 mg/hr for <24 hrs. PO: 30–120 mg PO q6–8h
Onset: 2–3 min
Duration: 1–3 hrs (bolus), up to 10 hrs (infusion)
Mechanism: Benzothiazepine CCB; prolongs AV nodal conduction, dilates coronary > peripheral arterioles
Clearance: Hepatic metabolism
Comments: Little effect on normal heart rates. Minimal inotropic effect. No effect on WPW accessory pathway. Caution with β-blockers and in wide QRS complex of unknown etiology, WPW, short PR interval. Rare LFT elevation.
Verapamil (Isoptin, Calan)
Indications: Angina, supraventricular tachycardia, atrial fibrillation or flutter, hypertension
Dose: Adult: 2.5–10 mg IV over ≥2 min. If no response in 30 min, repeat 5–10 mg (150 mcg/kg). Peds: 0–1 yr: 0.1–0.2 mg/kg IV; 1–15 yrs: 0.1–0.3 mg/kg IV. Repeat once if no response in 30 min
Onset: 1–5 min (peak 10 min)
Duration: 0.5–6 hrs
Mechanism: Phenylalkylamine CCB, prolongs AV nodal conduction. Negative inotrope and chronotrope; systemic and coronary vasodilator
Clearance: Hepatic metabolism; renal elimination (active metabolite has 20% potency)
Comments: May increase ventricular response to atrial fibrillation or flutter in patients with accessory tracts. Associated with more hypotension than diltiazem, especially with volatile anesthetics. Increases digoxin levels, potentiates neuromuscular blockade (may make neostigmine reversal difficult).
Nicardipine (Cardene)
Indications: Short-term IV treatment of hypertension
Dose: Infusion prep: 20 mg in 200 mL = 0.1 mg/mL; 5–15 mg/hr; start at 5 mg/hr and titrate ↑ q 5–10 min
Onset: 1–3 min
Duration of action: 10–30 min after bolus dose
Mechanism: Dihydropyridine CCB, selective relaxation of arterial resistance vessels with minimal ↓ chronotropy /dromotropy
Clearance: Hepatic metabolism, renal/biliary excretion
Comments: Associated with headache, less reflex tachycardia than nifedipine. Contraindicated in advanced aortic stenosis, decompensated heart failure. Increased cost relative to other short-acting potent antihypertensives.
Nifedipine (Procardia)
Indications: Angina, hypertension. Also used for vascular spasm after SAH, preterm labor, Raynaud’s
Dose: 10–30 mg PO tid–qid; 10 mg SL
Onset: 20 min PO, 2–3 min SL
Duration: 8 hrs
Mechanism: Dihydropyridine CCB, relaxes vascular smooth muscle causing systemic and coronary vasodilation; mild negative inotrope
Clearance: Hepatic metabolism (reduced efficacy with select CYP450 inhibitors)
Comments: Not available IV due to instability. Contraindicated in cardiogenic shock; caution in recent MI, CHF, unstable angina. May decrease serum glucose in diabetics. More coronary vasodilation than nitroglycerin, antianginal effect also from ↓ myocardial oxygen demand.
Clevidipine (Cleviprex)
Indications: Short-term IV treatment of hypertension
Dose: Adult: Initiate infusion at 1–2 mg/hr; double dose at 1.5–5 min intervals as needed (max 16 mg/hr)
Onset: 1–4 min
Duration: 5–15 min after infusion
Mechanism: Dihydropyridine CCB, selective relaxation of arterial resistance vessels and ↓ inotropy with minimal ↓ chronotropy /dromotropy
Clearance: Ester hydrolysis in plasma
Comments: Ultrashort acting. Formulated in lipid emulsion without preservatives (supports bacterial growth). Associated with reflex tachycardia, atrial fibrillation, acute renal failure. Monitor for rebound hypertension after discontinuation. Contraindicated in severe aortic stenosis, heart failure. Increased cost relative to other short-acting potent antihypertensives.
VASODILATORS
Fenoldopam (Corlopam)
Indications: Short-term management (<48 hrs) of severe hypertension
Infusion: Infusion prep: 10 mg in 250 mL = 40 mcg/mL; 0.1–1.6 mcg/kg/min. Titrate q15min. Do not bolus.
Mechanism: Dopamine (D1) receptor agonist causing rapid vasodilation of coronary, renal, mesenteric, and peripheral arteries
Clearance: Hepatic metabolism; 90% renal excretion
Onset: 5 min
Duration: 1–4 hrs after infusion
Comments: Promotes natriuresis and diuresis, maintains renal blood flow. Possible renal protective effect. May cause hypokalemia, dizziness, flushing, reflex tachycardia. Contains sulfites. Caution with glaucoma (may ↑ IOP).
Hydralazine (Apresoline)
Indications: Indicated for hypertension, pregnancy-induced hypertension, congestive heart failure
Dose: Adult: 5–20 mg IV q4h or prn. Max 40 mg/dose. PO available. Pregnancy-induced hypertension 5–10 mg IV q20–30min prn. Peds: 0.1–0.2 mg/kg/dose q4–6h, max 40 mg/dose
Mechanism: Unclear, causes direct ↓ vascular smooth muscle tone (arterial > venous)
Clearance: Extensive hepatic metabolism; renal elimination
Onset: 5–20 min (IV), peak ≥20 min
Duration: 2–6 hrs (IV)
Comments: May cause hypotension (diastolic > systolic), reflex tachycardia, systemic lupus erythematosus syndrome, thrombophlebitis. Potent cerebral vasodilator, maintains renal, splanchnic blood flow.
Isosorbide Dinitrate (Isordil)
Indications: Angina
Dose: 2.5–5 mg SL, may repeat q5–10min; not to exceed 3 doses in 15–30 min
Maintenance: 40–80 mg PO bid–tid
Onset: Slower than nitroglycerin (SL)
Duration: 4–6 hrs
Mechanism: Smooth muscle relaxation (NO donor)
Clearance: Nearly 100% hepatic metabolism; renal elimination
Comments: Reduces preload, afterload, myocardial O2 demand. Tolerance may develop. May cause hypotension, tachycardia, occasional bradycardia, methemoglobinemia. Avoid within 24 hrs of phosphodiesterase inhibitors (e.g., sildenafil).
Nitroglycerin (Tridil, Glycerol Trinitrate, Nitrostat, Nitrol, Nitro-Bid, Nitrolingual)
Indications: Angina, myocardial ischemia or infarction. Also used for hypertension, congestive heart failure, esophageal spasm, induced intraoperative hypotension, transient uterine relaxation (bolus).
Dose: Infusion prep: 50 mg in 250 mL D5W or NS = 200 mcg/mL; IV infusion initially at 5 mcg/min. Titrate every 3–5 min by 10 mcg/min to max 200 mcg/min or 1–3 mcg/kg/min; SL: 0.15–0.6 mg/dose q5min to max 3 doses in 15 min. Topical: 2% ointment, 0.5–2.5 inches q6–8h, max 5 inches q4h
Mechanism: Metabolized to NO (similar to nitroprusside) → smooth muscle relaxation in venules >> arterioles, causing systemic, coronary, and pulmonary vasodilatation; bronchodilation; biliary, gastrointestinal, and genitourinary tract relaxation
Clearance: Nearly complete hepatic metabolism; renal elimination
Onset: 1–2 min
Duration: 3–5 min
Comments: Potent venodilator, causes ↑ venous capacitance, ↓ cardiac preload, ↓ myocardial O2 demand. Causes coronary vasodilation, headache, absorption into IV tubing, potentiation of pancuronium. Tolerance may be avoided with 10–12 hrs nitrate-free period. May cause methemoglobinemia at very high doses. May diminish platelet aggregation, antagonize heparin. Avoid within 24 hrs of phosphodiesterase inhibitors (e.g., sildenafil).
Nitroprusside Sodium (Nipride, Nitropress)
Indications: Hypertension, induced intraoperative hypotension, acute congestive heart failure
Dose: Infusion prep 50 mg in 250 mL D5W or NS = 200 mcg/mL; infusion initially at 0.25–0.5 mcg/kg/min, then titrated to effect q3–5min (max 10 mcg/kg/min). Lower doses often adequate during general anesthesia
Onset: 30–60 sec (peak 1–2 min)
Duration: 1–5 min
Mechanism: Direct NO donor → activates guanylyl cyclase → ↑cGMP → potent vascular smooth muscle relaxation (arterial > venous)
Clearance: RBC and tissue metabolism; renal elimination of thiocyanate metabolite
Comments: Useful for immediate onset, rapid titration. Decreases preload and afterload. May cause reflex tachycardia, inhibition of hypoxic pulmonary vasoconstriction, excessive hypotension (especially with β-blockers); invasive BP monitoring recommended. Cyanide toxicity (product of initial degradation) is associated with tolerance of drug, ↑ mixed venous PaO2, metabolic acidosis → rx with sodium nitrate, sodium thiosulfate, or amyl nitrate. Thiocyanate toxicity (accumulates in renal failure) is associated with nausea, hypoxia, psychosis, weakness, thyroid dysfunction. Methemoglobinemia may require rx with methylene blue. Contraindicated with ↑ ICP (increases CBP and abolishes autoregulation), hypovolemia, B12 deficiency. Avoid within 24 hrs of phosphodiesterase inhibitors (e.g., sildenafil). Protect from light.
ANTIARRHYTHMICS
Adenosine (Adenocard)
Indications: Paroxysmal supraventricular tachycardia. Also used in Wolff–Parkinson–White syndrome.
Dose: Adult: 6 mg rapid IV push, may repeat 12 mg ×2 within 1–2 min; Peds: 0.1–0.2 mg/kg rapid IV push, increase by 50 mcg/kg q2min to max 250 mcg/kg
Onset: 10–20 sec
Duration: <10 sec
Mechanism: Slows conduction through SA and AV node, interrupts AV reentry pathways
Clearance: Metabolized in blood and tissue
Comments: Administer centrally if possible, follow dose with saline flush (ultra-rapid metabolism). Contraindicated in wide complex tachycardia, 2nd and 3rd degree AV blocks and sick sinus syndrome without pacing. Transient AV blockade may allow diagnosis of atrial fib/flutter underlying SVT. May accelerate rate in WPW, atrial fib/flutter. Significant adverse reactions: Hypotension, bronchoconstriction. 3–6 sec asystole after administration common.
Amiodarone (Cordarone)
Indications: ACLS, malignant ventricular dysrhythmias. Also used for atrial fibrillation (especially acute onset), SVT.
Dose: Infusion prep: 1,200 mg in 250 mL D5W or NS = 4.8 mg/mL. PO available Adult: Pulseless arrhythmia: 300 mg IVP, may repeat 150 mg IVP in 3–5 min to max 2.2 g/24 hrs; Arrhythmia: Load 150 mg IV over 10 min, may repeat 150 mg q10min if needed. Maintenance: 1 mg/min × 6 hrs, then 0.5 mg/min × 18 hrs; may repeat bolus to max 15 mg/kg/d. Peds: 5 mg/kg IV/IO; load 5 mg/kg IV over 20–60 min, Maintenance infuse 5–10 mcg/kg/min
Mechanism: Complex; prolongs action potential phase 3; α- and β-adrenergic blockade, ↓ AV conduction and sinus node function, prolongs PR, QRS and QT intervals
Clearance: Hepatic metabolism, biliary excretion
Comments: Class III antiarrhythmic. Contraindicated in 2nd and 3rd degree heart blocks, severe sinus node disease or sinus bradycardia, cardiogenic shock, thyroid disease. May increase serum levels of digoxin, diltiazem, oral anticoagulants, phenytoin. May cause hypotension, bradycardia with rapid infusion. Long-term use associated with hepatic, pulmonary, thyroid toxicity.
Lidocaine (Xylocaine)
Indications: Ventricular tachycardia due to surgical manipulation, acute MI, digitalis toxicity
Dose: Infusion prep: 2 g in 250 mL D5W = 8 mg/mL. Adult: Load: 1–1.5 mg/kg IV over 2–3 min; 2nd dose 5–30 min after 1st dose, 0.5–1.5 mg/kg to total 3 mg/kg; maintenance: 15–30 mcg/kg/min IV (1–2 mg/min). Peds: Load: 0.5–1 mg/kg IV, may repeat ×2 doses; maintenance: 15–50 mcg/kg/min IV. 1 mg/kg IV
Onset: 45–90 sec
Duration: 10–20 min
Mechanism: Decreases conductance of sodium channels, ↓ ventricular excitability, ↑ stimulation threshold
Clearance: Hepatic metabolism to active/toxic metabolites; renal elimination (10% unchanged)
Comments: May cause dizziness, seizures, disorientation, heart block (with myocardial conduction defect), hypotension, asystole, tinnitus, unusual taste, vomiting. Crosses the placenta. Caution in patients with Wolff–Parkinson–White syndrome, intraventricular heart block, hypokalemia. No effect on SA node, generally no ↓ in arterial pressure or intropy.
Procainamide (Pronestyl)
Indications: Life-threatening ventricular arrhythmia. Also used for atrial fibrillation/flutter.
Dose: Adult: Load 20 mg/min IV, up to 17 mg/kg, until toxicity or desired effect occurs. Stop if ≥50% QRS widening or PR lengthening occurs; maintenance: 1–4 mg/min. Peds: Load: 3–6 mg/kg over 5 min, not to exceed 100 mg/dose; repeat q5–10min to maximum dose of 15 mg/kg; maintenance: 20–80 mcg/kg/min; max 2 g/24 hrs
Mechanism: Blocks sodium channels; decreases excitability, conduction velocity, automaticity, and membrane responsiveness with prolonged refractory period
Clearance: Hepatic conversion of 25% to active metabolite N-acetylprocainamide (NAPA), a class III antidysrhythmic; renal elimination (50–60% unchanged)
Comments: Class I antiarrhythmic. May cause ↑ ventricular response with atrial tachydysrhythmias unless receiving digitalis; asystole (with AV block); myocardial depression; CNS excitement; blood dyscrasia; lupus syndrome with +ANA; liver damage. Intravenous administration can cause hypotension from vasodilation, accentuated by general anesthesia. Avoid in torsades de pointes, 2nd/3rd degree or complete heart block (unless pacemaker present), lupus, myasthenia gravis. Decrease load by one-third in congestive heart failure or shock. Reduce doses in hepatic or renal impairment. Contains sulfite.
HEART FAILURE
Digoxin (Lanoxin)
Indications: Symptom improvement in heart failure, atrial fibrillation/flutter
Dose: Adult: Load 0.4–0.6 mg IV or 0.5–0.75 mg PO; maintenance 0.1–0.3 mg IV or 0.125–0.375 mg PO qd; Peds: Load (total daily doses usually divided into two or more doses); Neonates: 15–30 mcg/kg/d; Infants: 1 mo–2 yrs: 30–50 /kg/d; 2–5 yrs: 25–35 mcg/kg/d; Peds: 5–10 yrs: 15–30 mcg/kg/d; >10 yrs: 8–12 mcg/kg/d. Maintenance: 20–35% of loading dose (↓ in renal failure)
Mechanism: Increases myocardial contractility via inhibition of sodium/potassium ATPase leading to ↑ intracellular calcium; decrease chronotropy via ↓ conduction in AV node and Purkinje fibers.
Onset: 30 min (peak 2–6 hrs)
Duration: 3–4 d
Clearance: Hepatic metabolism, renal excretion (50–70% unchanged)
Comments: Suppresses SA node, positive inotrope, increases peripheral vascular resistance. Narrow therapeutic range (therapeutic level: 0.8–2.0 ng/mL). May cause gastrointestinal intolerance, blurred vision, ECG changes, or dysrhythmias. Toxicity potentiated by hypokalemia, hypomagnesemia, hypercalcemia. Use cautiously in Wolff–Parkinson–White syndrome and with defibrillation. Heart block potentiated by β-blockade and calcium channel blockade. Symptoms of toxicity include CNS depression, confusion, headache, anorexia, nausea, vomiting, visual changes, arrhythmias, and seizures. Reduces hospitalization but not mortality in CHF. (N Engl J Med. 1997;336:525–533)
Nesiritide (B-type natriuretic peptide, BNP, Natrecor)
Indications: Treatment of patients with acutely decompensated CHF with dyspnea at rest or minimal activity
Dose: Infusion prep 1.5 mg in 250 mL = 6 mcg/mL; load 2 mcg/kg over 1min; infuse 0.01 mcg/kg/min. May ↑ no more often than q3h (max 0.03 mcg/kg/min), bolus 1 mcg/kg before changing rate
Mechanism: Binds to guanylate cyclase receptor; stimulates cGMP production, resulting in vascular smooth muscle relaxation (similar to nitric oxide)
Onset: 60% effect in <15 min, peak effect <1 hr
Duration: 2–4 hrs (IV bolus)
Comments: Decreases pulmonary capillary wedge pressure and systemic arterial pressure in heart failure patients; ↑ renal blood flow and GFR. No effect on cardiac contractility. Multiple chemical incompatibilities. May cause hypotension (especially with ACE inhibitors), ventricular and atrial dysrhythmias, angina, bradycardia, tachycardia, azotemia. Use caution in renal disease. Contraindicated in cardiogenic shock, SBP <90, valvular stenosis, restrictive/obstructive cardiomyopathy.

Full access? Get Clinical Tree








