FIG. 30.1 Anatomy of the airway. (From Chabner D-E: Medical terminology: a short course, ed 7, St. Louis, 2015, Elsevier.)
While it is likely a thorough airway assessment is performed by the anesthesia provider on all patients during the preoperative period, a quick reassessment by the PACU nurse upon the patient’s arrival to the recovery room will identify any changes to the airway that may have occurred due to surgery, medications, or other procedures. Additionally, the PACU nurse may query the anesthesia provider during the transfer of care about any airway issues specific to the patient.
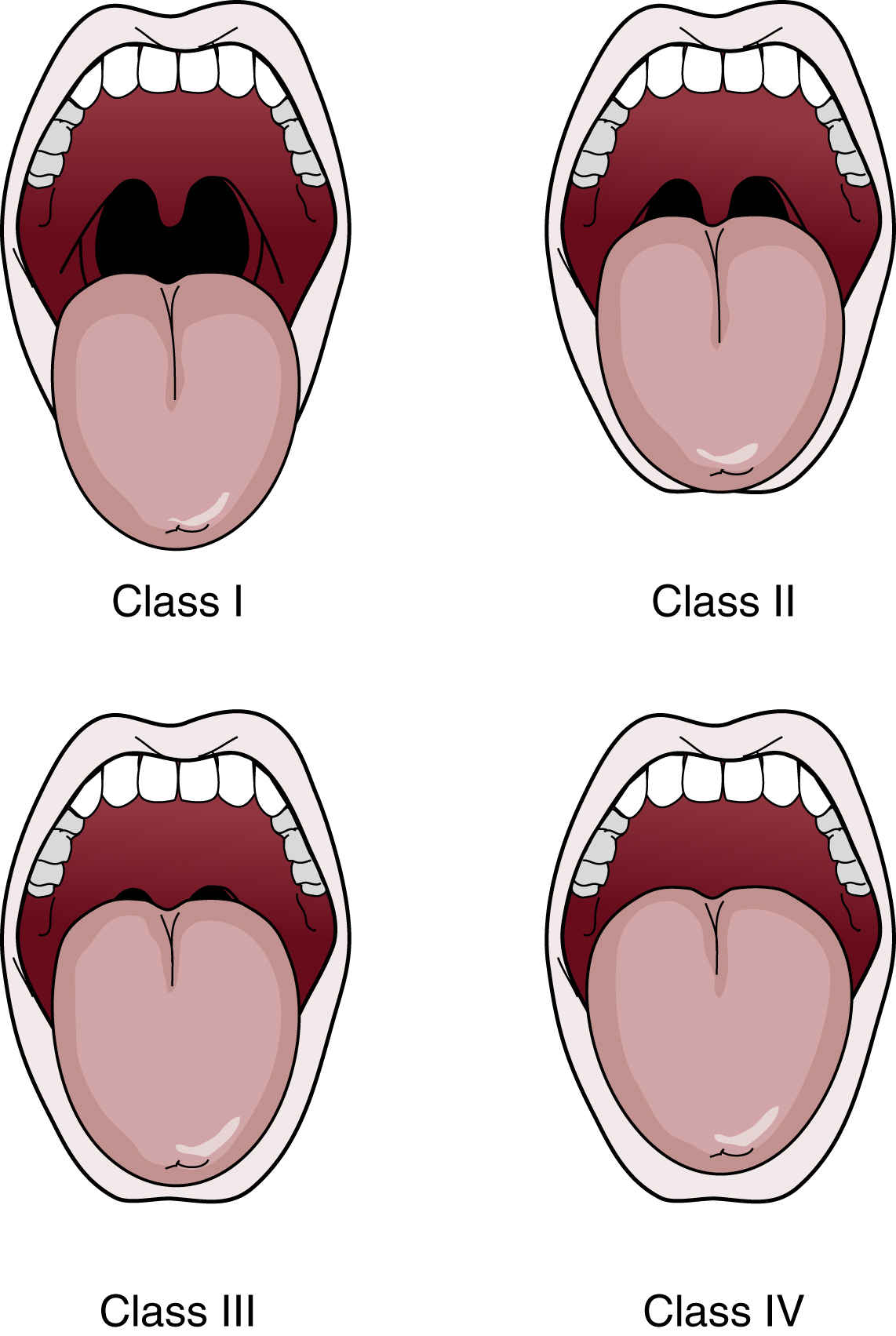
FIG. 30.2 Mallampati score findings. (From Phillips N: Berry & Kohn’s operating room technique, ed 13, St. Louis, 2017, Elsevier.)
Potential Airway Issues
A difficult airway should be anticipated in every patient until proven otherwise. With that, many patients are extubated in the recovery room and may experience issues with ventilation and oxygenation. There are many factors that contribute to the nurse’s inability to adequately oxygenate a patient during any phase of the surgical stay. A few of these are discussed in the following text.
Airway Obstruction
An airway obstruction refers to an obstruction of airflow into and/or out of the lungs. During the perioperative period, this is most commonly a symptom of sedation where soft tissue in the pharynx occludes the airway and patients struggle with inhalation. Generally speaking, obese patients and those who are pregnant or have sleep apnea are particularly vulnerable, but obstruction can occur in any airway. Airway obstruction is particularly disconcerting because it can quickly lead to hypoxia and cell death. Indications of airway obstruction in spontaneously ventilating patients include respiratory effort with little or no movement of air, retraction of the muscles of respiration, a rocking chest motion, abnormal or absent breath sounds, cyanosis, and other signs associated with hypoxemia and hypercarbia.3

FIG. 30.3 Opening of airway with head-chin-lift maneuver. (From Lewis SL, Dirksen SR, Heitkemper MM, et al.: Medical-surgical nursing: assessment and management of clinical problems, ed 9, St. Louis, MO, 2014, Elsevier.)
Upon recognizing an airway obstruction, the nurse should place the patient supine, position a pillow beneath the shoulders and head, and tilt the head backward, unless contraindicated, which extends the neck. If this change in position fails to clear the obstruction in a spontaneously breathing patient, the nurse should then lift the mandible upward (jaw thrust) using moderate pressure (Fig. 30.3). Often, this maneuver is all that is necessary for adequate spontaneous respiratory effort to be effective. If the airway obstruction does not clear, the oral cavity should be inspected for foreign material, and the oral pharynx may be suctioned if necessary. If large particles are present, the nurse should turn the patient’s head to the side and remove the particles manually, avoiding the finger sweep technique that could potentially worsen the obstruction.4 Nurses should review proper technique for the Heimlich maneuver in suspected cases of foreign body obstruction. An oropharyngeal or nasopharyngeal airway may also be used to relieve an airway obstruction of a patient with spontaneous ventilatory effort caused by soft tissue in the pharynx, as described later in this chapter.
Hypoventilation and Apnea
If spontaneous respiratory effort is absent or inadequate, basic life support (BLS) should be initiated. Hypoventilation and apnea refer to inadequate or absent spontaneous respiratory effort. Both represent a serious condition for patients as they are unable to oxygenate vital organs or rid the body of carbon dioxide, which can have deleterious effects. During the perioperative period, this too is commonly a result of sedation or residual anesthesia where medications have been used that either (1) raise the level of CO2 in the body necessary to initiate a breath or (2) paralyze muscles including those needed for respiration. Many other factors related to surgery and the patients themselves can also contribute to hypoventilation and apnea. Indications of hypoventilation and apnea include an observation of little to no respiratory effort, no movement of air in and out of the airway, and tachycardia. If unrecognized, hypoventilation and apnea can lead to bradycardia, cyanosis, and death.3 Upon recognizing insufficient ventilation, the nurse should initiate BLS. If the patient has a pulse, positive pressure ventilation must be initiated immediately. This is often accomplished with the use of a bag-valve-mask (BVM) device as described later in this chapter.
Loss of Airway Reflexes
Anesthesia as well as medications, certain surgical procedures, and patient conditions can adversely affect the protective reflexes of the airway. Under normal conditions, human beings are able to prevent substances such as food or drink, pharyngeal secretions, and stomach contents from entering the airway through mechanisms such as coughing, swallowing, and other complex physiologic mechanisms beyond the scope of this chapter. In deeply sedated, obtunded, or unconscious patients, these important reflexes can be less responsive or not responsive at all, leading to aspiration. Aspiration or the inhalation of acidic and bacterial-laden secretions and other undesirable substances into the lower airways can lead to airway obstruction, chemical pneumonitis (otherwise known as Mendelson’s syndrome), pneumonia, and difficulties with respiratory gas exchange. It is important to anticipate and monitor closely those patients with predisposing factors that could lead to a loss of protective airway reflexes to identify and address such issues early.
Laryngospasm
Partial or complete closure of the vocal cords can occur because of increased secretions or as a reflex caused by stimulation of the irritant receptors.5 Assessment of the airway during a laryngospasm reveals reduced or no breath sounds usually with an effort to breathe. If partial laryngospasm is present, the patient may make crowing sounds, especially on inspiration. Interventions include the administration of 100% oxygen under positive pressure with a BVM unit. If the patient’s lungs cannot be ventilated, the perianesthesia nurse should call for help and prepare for the administration of a short-acting paralytic such as succinylcholine and/or endotracheal intubation. See Chapter 29.
Mask Ventilation
Mask ventilation is often one of the first steps employed by nurses assisting patients with difficulty breathing during the perioperative period. Mask ventilation is the provision of air and oxygen via the use of a BVM device. The requirements for a properly functioning BVM unit are addressed in Box 30.1.3 For optimal airway management, the perianesthesia nurse should be competent in its use. The procedure of mask ventilation begins with the nurse positioned behind the patient’s head. The mask should be securely placed over the patient’s mouth and nose with the neck extended. The lower jaw should be lifted at its angle with the other fingers of the hand holding the mask. The thumb of that hand should be placed at the top of the mask. Moderate downward pressure on the mask provides compression over the bridge of the nose and reduces air leakage (Fig. 30.4). Two-person ventilation, where one nurse holds the mask on the patient’s face and another squeezes the bag, can be very effective in reducing the amount of pressure necessary to ventilate the lungs.
While the perianesthesia nurse ventilates the lungs, another qualified provider should auscultate the chest and assess the quality of breath sounds. If assistance is unavailable, the perianesthesia nurse should determine whether the chest rises with inspiration and falls with expiration and look for other signs of oxygenation.6 If breath sounds are not audible during auscultation or if there is any question about the effectiveness of ventilatory efforts, an appropriately sized oropharyngeal or nasopharyngeal airway may be inserted, and BVM ventilation should be resumed. These adjunct airway devices relieve an obstruction by providing a mechanical conduit for air to pass between the base of the tongue and the posterior oropharynx.3

FIG. 30.4 Holding of mask with one hand. (From Miller R, et al.: Miller’s anesthesia, ed 7, Philadelphia, PA, 2010, Elsevier.)
The oral airway can be noxious to conscious or lightly sedated patients and should be used with extreme caution in this population.7 The untoward consequences associated with inappropriate use of the oral airway include retching, vomiting, bradycardia, bleeding, damage to the teeth or tongue, and laryngospasm.5 It is important to choose the proper size oropharyngeal airway, which is determined by assessing the distance from the corner of the mouth to the angle of the jaw (Fig. 30.5). To place an oropharyngeal airway, the perianesthesia nurse should first open the patient’s mouth with the right hand and place a tongue blade toward the posterior aspect of the tongue with the left hand. Slight pressure should then be applied to draw the tongue forward. With the oropharyngeal airway held in the right hand, the nurse should slip the airway in over the tongue blade into the oropharynx. The airway should not be twisted or forced into place, and placement should be accomplished quickly with careful avoidance of trauma to the soft tissue and teeth.
Compared with the oropharyngeal airway, the nasopharyngeal airway is less rigid and less stimulating to the irritant receptors in the upper airway, especially in awake or lightly sedated patients.8 The nasopharyngeal airway should be lubricated with a water-soluble lubricant and gently passed with the right hand through the nare along the curvature of the nasopharynx into the oropharynx. The nasopharyngeal airway should never be forced. If resistance is encountered on placement, the contralateral nare should be considered unless otherwise indicated. When positioned properly, the nasopharyngeal airway should rest between the base of the tongue and the posterior pharyngeal wall.8 This airway should not be used in patients with nasal-septal deformities, a leakage of cerebrospinal fluid from the nose, or a coagulation disorder.5
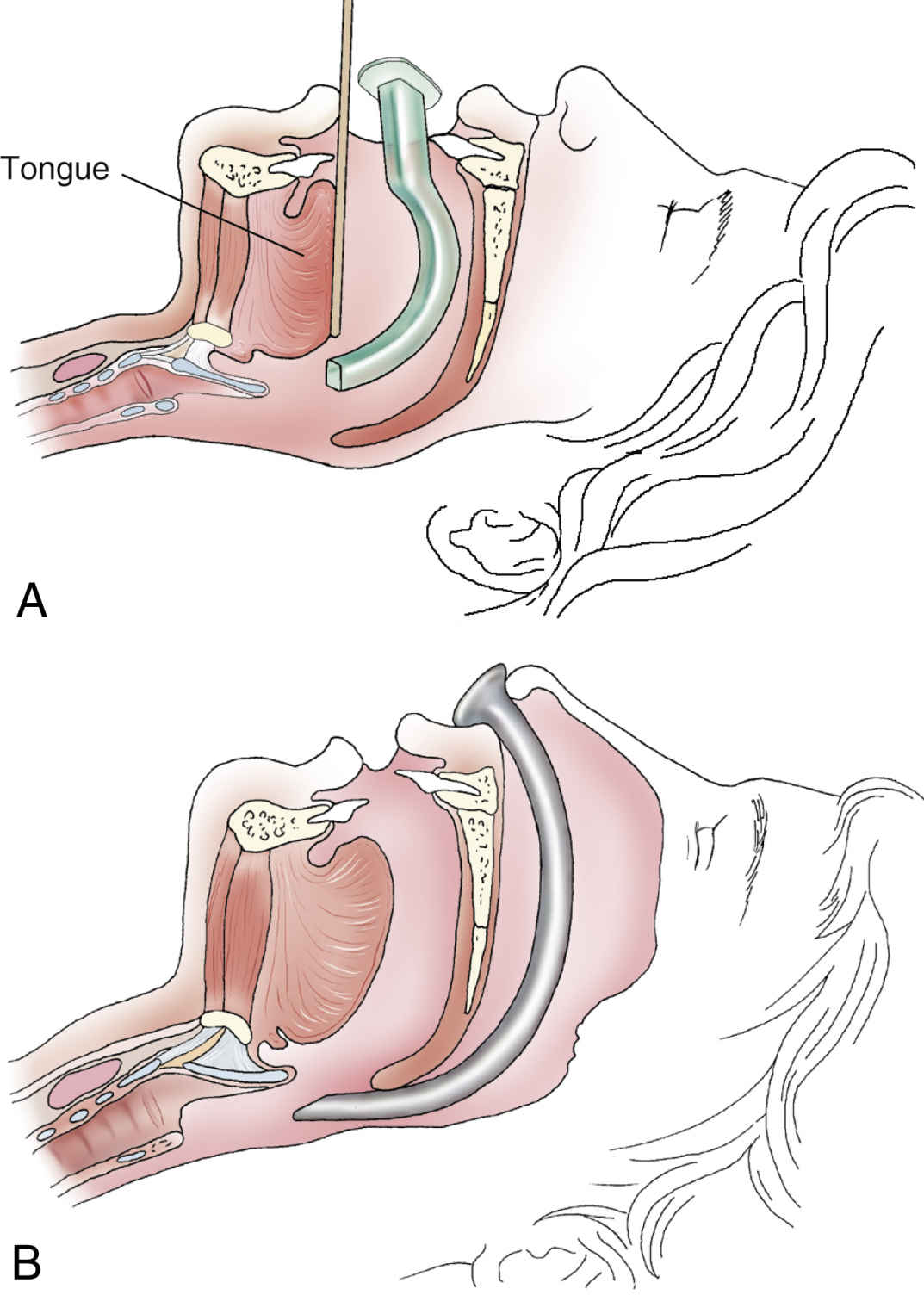
FIG. 30.5 Sizing of oral airway. The correct size oropharyngeal airway spans the space between the corner of the mouth to the angle of the jaw. (In Malamed SF: Medical emergencies in the dental office, ed 7, St. Louis, 2003, Elsevier. From McSwain NE, Paturas JL: The basic EMT: comprehensive prehospital patient care, ed 2, St. Louis, 2003, Elsevier.)
After the oropharyngeal or the nasopharyngeal airway has been placed properly, ventilation should be attempted. Assessment of ventilatory effort should be continuous. With insertion of the oropharyngeal airway, the airway obstruction often clears. In this instance, the patient should be given a breath via the BVM unit and assisted with any spontaneous ventilatory effort. If apnea persists, positive-pressure ventilation should be initiated via BVM with adequate tidal volumes. For a normal healthy adult, the perianesthesia nurse should consider tidal volumes of 8 to 12 mL/kg at a rate of 12 to 14 breaths/min as initial efforts. For prevention of oxygen delivery into the stomach, pressure created by positive pressure ventilation using the BVM should not exceed 25 cm H2O.5
Intubation of the Trachea
Airway experts agree that, in an airway crisis, mask ventilation is necessary and intubation of the trachea is a luxury. In most circumstances, excessive efforts to intubate a patient should not supplant mask ventilation that is adequately oxygenating the patient. Intubation does, however, provide a definitive airway, greatly minimizing the risk of aspiration, laryngospasm, and hypoxia that can accompany mask ventilation. Intubation of the trachea is a proficiency reserved for only those personnel with advanced airway management training and who are properly licensed and credentialed to intubate. All providers should be familiar with their state’s scope of professional practice as well as their hospitals’ policies regarding intubation privileges.
It is important that the perianesthesia nurse is knowledgeable about the technique for tracheal intubation regardless of his or her level of participation to work as part of a team managing a difficult airway. Endotracheal intubation indicates the placement of an endotracheal tube directly into the trachea. When the endotracheal tube is placed through the mouth, the method is called orotracheal intubation. When the endotracheal tube is placed through the nose, the method is called nasotracheal intubation. Indications for endotracheal intubation in the perioperative period include the inability of the patient to protect the airway, a mechanism to provide prolonged mechanical ventilation, hypoxia, and cardiac and respiratory arrest.9
Conditions present outside of the controlled environment of the operating room (OR) may be less than ideal for successful tracheal intubation. The patient’s position in the bed, excess upper airway secretions, lack of readily available equipment, and intact airway reflexes can contribute to the difficulty in performing this procedure in the preoperative or postoperative area.
Equipment for Endotracheal Intubation
Adult and pediatric intubation equipment should be readily available throughout the perioperative period at all times. This equipment should be inspected daily and after each use for proper functioning. For a list of the suggested airway management equipment and supplies, see Box 30.2. Table 30.1 shows the recommended sizes for endotracheal tubes given the patient demographic. The formula age/4 + 4 may be used as a guide when preparing endotracheal tubes for pediatric patients.10 For example, a size 5.0-mm endotracheal tube may be prepared for a 4-year-old child. Because of their importance, the laryngoscope and endotracheal tubes are discussed here in detail.








