8 Arterial Hypoxemia
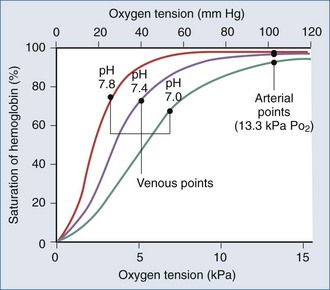
Arterial hypoxemia is defined as a partial pressure of oxygen in arterial blood (PaO2) less than 80 mm Hg while breathing room air. The PaO2 represents the amount of oxygen in physical solution, whereas the oxygen saturation represents the fractional amount of oxyhemoglobin relative to total hemoglobin concentration. Oxygen saturation varies with the PaO2 in a nonlinear relationship and is affected by temperature, partial pressure of carbon dioxide in arterial blood (PaCO2), pH, and 2,3-diphosphoglycerate concentration (Figure 8-1).
Falsely low saturations can be recorded if there is a poor waveform or if light absorption is decreased by dark blue or black nail polish. Patients with methemoglobinemia can have a falsely low oxygen saturation, whereas patients with carboxyhemoglobinemia can have a falsely elevated oxygen saturation, because the pulse oximeter cannot differentiate carboxyhemoglobin from oxyhemoglobin.1 Finally, because the oxygen-hemoglobin dissociation curve is affected by temperature, pH, partial pressure of carbon dioxide (PCO2), and 2,3-diphosphoglycerate concentration, patients can have a higher or lower saturation for a given PaO2.
Etiologies for hypoxemia are best understood if approached from a physiologic point of view rather than by referring to a list of possible differential diagnoses. Simply stated, hypoxemia results from an imbalance between pulmonary ventilation and pulmonary capillary blood flow.2
 Reduced Alveolar Oxygenation
Reduced Alveolar Oxygenation
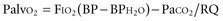
Alveolar oxygenation is defined by the equation:
where FIO2 is the concentration of inspired oxygen, BP is the barometric pressure, BPH2O is the partial pressure of water, and RQ is the respiratory quotient. The respiratory quotient represents the amount of oxygen consumed relative to the amount of carbon dioxide produced when nutrients are metabolized. RQ is generally assumed to be 0.8. Under normal conditions, where the FIO2 is 21%, BP is 760 mm Hg, BPH2O is 47 mm Hg, and PaCO2 is 40 mm Hg, the Palvo2 = 0.21(760 − 47) − 40/0.8 = 100 mm Hg. According to the equation, several factors may contribute to lower alveolar oxygenation. One is a reduction in barometric pressure, causing hypobaric hypoxemia that affects those climbing at high altitudes.3 The second factor is an increase in PaCO2, which can be explained by the relationship: PaCO2 = carbon dioxide production/respiratory rate (tidal volume − dead space). Accordingly, the PaCO2 increases with either an increase in production or a decrease in alveolar ventilation. Alveolar ventilation represents that portion of the minute ventilation undergoing blood-gas exchange and is represented by the product of respiratory rate and tidal volume minus dead space. Medications such as narcotics and sedatives that reduce the respiratory rate, and processes such as neuromotor weakness that reduce tidal volume, are common causes of hypercarbia.