UNIT II: CARDIOVASCULAR CONDITIONS
CHAPTER 7
Arrhythmia
Judy Cheng, PharmD, MPH, BCPS, CHFN, FCCP
An arrhythmia is defined as a disturbance of cardiac electrical conduction. The synchronous interaction between the electrical and the mechanical properties of the heart is important if the heart is to function properly and maintain adequate blood supply and perfusion to other vital body organs. The management of arrhythmias continues to evolve as results of many landmark studies are published.
With the original discovery of surface electrocardiography (ECG) and the availability of intracardiac recordings and programmed cardiac stimulation, there is considerable insight into cardiac electrophysiology. This technology has allowed for sophisticated classification of many arrhythmias.
Cardiac arrhythmias can be broadly classified into two groups: supraventricular (originating above the ventricle) and ventricular (originating from the ventricle) arrhythmias. Common supraventricular arrhythmias include atrial fibrillation, atrial flutter, paroxysmal supraventricular tachycardia (PSVT), sinus tachycardia, and bradycardia. Atrial fibrillation is probably the most common sustained cardiac arrhythmia encountered in primary care practice. The prevalence of atrial fibrillation increases with increasing age and the presence of structural heart disease. Atrial fibrillation is the major cause of stroke, especially in the elderly. Ventricular arrhythmias include premature ventricular contractions (PVCs), monomorphic and polymorphic (such as torsades de pointes) ventricular tachycardia (VT), and ventricular fibrillation (VF).
Multiple antiarrhythmic agents are available for management of these disorders. Unfortunately, many problems are associated with these agents, proarrhythmia being the most significant because it has a potential effect on patient mortality. Fortunately, technical advances have been made in the development of nondrug therapies. Some examples include radiofrequency ablation, the internal cardioverter/defibrillator, and pacemakers.
This chapter discusses the pathophysiology and management of arrhythmias in a primary care setting, with an emphasis on long-term management to prevent complications such as life-threatening ventricular arrhythmias, heart failure, or thromboembolic events.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
Cardiac Electrical Condition Pathway
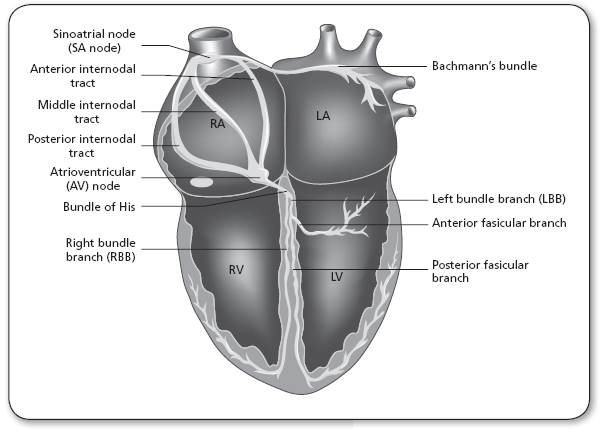
The heart is an organ that is capable of producing an intrinsic electrical rhythm and has automaticity. This rhythm may be modified by the autonomic nervous system (sympathetic and parasympathetic nervous systems). In normal cardiac conduction, the electrical activity begins in the sinoatrial (SA) node, known as the pacemaker of the heart. The SA node is located in the upper portion of the right atrium (Figure 7.1).
In adults, the SA node fires at a regular rate of 60 to 100 beats per minute (bpm), which is defined as the normal sinus rhythm (NSR). Following discharge of the SA node, the electrical impulse is conducted through the right atrium, to the left atrium, then to the atrioventricular (AV) node (Figure 7.1). The impulse continues to conduct through the AV node, with a momentary delay, then to the bundle branches. From the bundle branches, the electrical activity is carried to the ventricular muscle by networks of Purkinje fibers. In abnormal cardiac conduction, enhanced automaticity and formation of reentry circuits at certain foci of the heart (either SA node or other latent pacemakers) may lead to tachycardia.
Electrical impulses are capable of conduction through ion channels. The major ion channels include sodium and potassium channels (fast conduction channels), as well as calcium channels (slow conduction channels). They are labeled as fast and slow conduction channels based on the speed of ion influx and efflux. These conduction channels are distributed throughout the myocardium. However, the atrial and ventricular tissue has more sodium and potassium channels compared to calcium channels, and the SA node and the AV node have more calcium channels relative to sodium and potassium channels. Therefore, calcium channel blockers such as verapamil will demonstrate more pharmacological activity at the SA and the AV nodes, as these nodes are where more calcium channels are located. Class I and III antiarrhythmic agents, such as procainamide and amiodarone, are sodium channel blockers and potassium channel blockers, which demonstrate more pharmacological activity in the atrial and ventricular tissue.
FIGURE 7.1
The electrical conduction pathway of the heart.
LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle.
Electrocardiogram
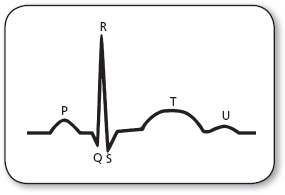
The ECG complexes reflect the cardiac electrical activity. Waveforms on the ECG represent electrical conduction of the heart, the P wave represents atrial depolarization, the QRS complex represents ventricular depolarization, and the T wave represents ventricular repolarization (Figure 7.2). The atrial contraction follows the P wave and the ventricular contraction follows the QRS complex. Three key intervals play an important part in ECG interpretation. The PR interval, normally 0.12 to 0.20 seconds in duration, represents the travel of electrical impulse from the SA node through the AV node. A prolongation of the PR interval indicates a delay in AV nodal conduction, known as first-degree heart block. The QRS interval, normally <0.12 seconds in duration, represents the time required for the ventricle to depolarize. Prolongation of the QRS interval may indicate ventricular hypertrophy (it takes longer for a thicker piece of muscle to depolarize) or a defect in the conduction of the Purkinje fibers. The QT interval, normally 0.4 seconds or less, represents the time necessary for ventricular depolarization and repolarization. Prolongation of the QT interval (>0.5 seconds) indicates prolongation of the relative refractory period. During this phenomenon, the ventricles are especially vulnerable to extra stimuli. This increases the risk of developing life-threatening arrhythmias such as torsades de pointes.
Pathophysiology
The mechanisms of tachyarrhythmias (both supraventricular and ventricular) have been classified into two general categories: those resulting from an abnormal impulse generation and those resulting from an abnormal impulse conduction or reentrant tachycardia.
Automatic tachycardias depend on spontaneous impulse generation in latent pacemakers, which compete with the SA node for dominance of cardiac rhythm. If the rate of spontaneous impulse generation of the abnormally automatic tissue exceeds that of the SA node, then an automatic tachycardia may result. Trigger automaticity is also a possible mechanism for abnormal impulse generation. Trigger automaticity is the transient membrane depolarization that occurs during repolarization (early after-depolarization) or after depolarization (delayed after-depolarization) but before repolarization.
Reentry tachycardia involves indefinite propagation of the impulse and continued activation of previously refractory tissue. Three conduction requirements must be fulfilled for the formation of a viable reentrant focus: There must exist two pathways for impulse conduction with an area of unidirectional block (prolonged refractoriness) and slow conductions in the other pathway.
Classification of Cardiac Arrhythmias |
SUPRAVENTRICULAR |
Premature atrial contraction Atrial fibrillation Atrial flutter Paroxysmal supraventricular tachycardia (Wolff–Parkinson–White syndrome, Lown–Ganong–Levine syndrome) Sinus bradycardia |
VENTRICULAR |
Premature ventricular contractions Ventricular tachycardia Ventricular fibrillation Torsades de pointes |
A critically timed premature beat initiates reentry. The premature impulse enters both conduction pathways but encounters refractory tissue in one of the pathways at the area of the unidirectional block. The impulse subsides because it is still refractory from the sinus impulse. Although it fails to propagate in one pathway, the impulse will still proceed in a forward (antegrade) direction through the other pathway because of this pathway’s relatively shorter refractory period. The impulse may then proceed through the loop of tissue and reenter the area of the unidirectional block in a backward (retrograde) direction. Because the antegrade pathway has slow conduction properties, the area of unidirectional block has time to recover its excitability. The impulse can proceed retrograde through this (previously refractory) tissue and continue around the loop of tissue. The reentrant focus may excite surrounding tissue at a rate greater than that of the SA node, and a clinical tachycardia results.
Different precipitating factors of automaticity and reentry may lead to different types of bradyarrhythmias or tachyarrhythmias. Bradycardia is usually due to sick sinus or AV nodal conduction delay or blockade. Classifications of cardiac arrhythmias are summarized in Table 7.1. Pathophysiology of some of the more clinically significant arrhythmias is discussed in greater detail later in this chapter.
 SUPRAVENTRICULAR ARRHYTHMIA
SUPRAVENTRICULAR ARRHYTHMIA
Atrial Fibrillation and Atrial Flutter
In atrial fibrillation, reentry circuits are formed when the atrium is being stretched or disturbed. They take over the SA node and become multiple independent pacemakers of the heart. All of these pacemakers beating independently result in an overall atrial rate of 400 to 600 bpm. In atrial flutter, the mechanism is similar except that there is one instead of multiple reentry circuits.
Paroxysmal Supraventricular Tachycardia
PSVTs include those arrhythmias caused by AV nodal reentry, SA nodal reentry, and intra-atrial reentry. AV nodal reentry is by far the most common form of PSVT. Lown–Ganong–Levine (LGL) syndrome is an example of AV nodal reentry PSVT. Wolff–Parkinson–White (WPW) syndrome is another type of PSVT that involves both the AV node (slow conduction pathway) and an extra nodal AV connection (accessory fast conduction pathway). PSVT types that involve an accessory pathway may be the more common orthodromic (down AV node, up accessory pathway, which usually presents with a narrow/normal QRS interval on ECG), or the less common antidromic (down accessory pathway, up AV node, usually with a wide QRS interval on ECG).
 VENTRICULAR ARRHYTHMIAS
VENTRICULAR ARRHYTHMIAS
Ventricular Tachycardia
VT is defined as three or more repetitive PVCs, occurring at a rate >100 bpm. VT can be subdivided into two major types: monomorphic VT, which has a consistent QRS morphology; and polymorphic VT, which has varying QRS morphology. VT may occur acutely as a result of metabolic abnormalities; electrolyte abnormalities such as hypokalemia or ischemia; organic heart disease such as heart failure or left ventricular aneurysm; or drug toxicities such as digoxin overdose. VT, if sustained for a prolonged period of time, can lead to hemodynamic collapse. Immediate treatment is required.
Torsades de Pointes
Torsades de pointes is a rapid form of polymorphic VT associated with delayed ventricular repolarization (prolonged QT intervals). Table 7.2 lists the common causes of torsades de pointes.
Ventricular Fibrillation
VF is an electrical anarchy of the ventricle, resulting in no blood pressure or cardiac output. VF is a medical emergency that requires advanced cardiac life support measures. VF is often preceded by VT. VF occurs most commonly in patients with ischemic heart disease, WPW, and (less commonly) mitral valve prolapse.
PHYSICAL CONDITIONS |
Congenital long QT syndrome Myocarditis Ischemia Severe bradycardia due to AV block, heart rate <50 bpm Hypokalemia Hypomagnesemia Hypothyroidism Cardiomyopathy Subarachnoid hemorrhage |
DRUGS |
Antiarrhythmic agents Class IA (procainamide, quinidine) Class IC (flecainide, propafenone) Class III (amiodarone, sotalol, ibutilide) Psychotropic agents Phenothiazines Tricyclic antidepressants Haloperidol Toxins Organophosphate insecticides Arsenic Antihistamines Terfenadine Astemizole Antibiotics Pentamidine Macrolide Fluoroquinolones |
AV, atrioventricular.
 EPIDEMIOLOGY
EPIDEMIOLOGY
The most common type of arrhythmia, other than atrial and ventricular premature contraction (which most people will experience during their lifetime), is atrial fibrillation. It is estimated that by the year 2050, 16 millions Americans will have atrial fibrillation (Lloyd-Jones et al., 2004). Heart failure and rheumatic heart disease were the most powerful predictive precursors for atrial fibrillation, with relative risk in excess of sixfold. Hypertension, a history of cerebrovascular disease, diabetes, and left ventricular hypertrophy were also found to be significantly associated with atrial fibrillation.
The clinical importance of atrial fibrillation, other than its difficult-to-tolerate signs and symptoms, such as palpitations, dizziness, and fatigue, is its relation to a mortality rate double that of control subjects. Much of the morbidity and mortality related to atrial fibrillation is caused by stroke (Wolf et al., 1991). This is because atrial fibrillation creates turbulent flow in the cardiac chambers, promoting the formation of thrombi. Such thrombi, when dislodged from the cardiac chambers, may eventually lodge in another organ and lead to a thromboembolic event. Other morbidity and mortality related to atrial fibrillation include heart failure. Without thromboprophylaxis, the risk of ischemic stroke in patients with nonrheumatic atrial fibrillation is approximately 5% per year (Wolf et al., 1991). For ventricular arrhythmias, the incidence of sudden cardiac death varied from <200,000 to 450,000 annually based on whether the patients also have coronary heart disease (Zipes et al., 2006).
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
Supraventricular Arrhythmias
PREMATURE ATRIAL COMPLEXES
A premature atrial complex (PAC) is an electrical impulse originating in the atria outside of the SA node. PACs often occur without apparent cause or symptoms.
Commonly recognized clinical causes include the use of stimulants such as caffeine, tobacco, or alcohol. The ECG criteria are:
 Rhythm: irregular
Rhythm: irregular
 P waves: different in morphology from those of sinus mode origin
P waves: different in morphology from those of sinus mode origin
PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA
PSVT is a clinical syndrome characterized by repeated episodes of atrial tachycardia with an abrupt onset (preceded frequently by a premature atrial contraction), lasting from a few seconds to many hours. They usually end abruptly and often can be terminated by vagal maneuvers. Possible causes of PSVT include physical and psychological stress, hypoxia, hypokalemia, and excessive use of caffeine or other stimulants. Primary cardiac causes include myocardial infarction (MI), congenital heart disease, and cardiomyopathy. Other causes include digitalis toxicity and chronic pulmonary disease. Patients may feel a sudden rapid palpitation and severe anxiety. Heart failure, angina, and shock may occur as a result of a decreased cardiac output and an increased need for myocardial oxygen, if the tachyarrhythmia is persistent.
The ECG criteria are:
 Rate: The atrial rate is usually 160 to 240 bpm
Rate: The atrial rate is usually 160 to 240 bpm
 Rhythm: Regular. The ventricular rate is most often regular with 1:1 AV conduction when the atrial rate is <200. When atrial rates are above 200, 2:1 AV block is common. Higher-grade block may also occur
Rhythm: Regular. The ventricular rate is most often regular with 1:1 AV conduction when the atrial rate is <200. When atrial rates are above 200, 2:1 AV block is common. Higher-grade block may also occur
 P wave: P waves may be difficult to identify because they can be buried in the preceding T wave. However, when visualized, their morphology is different from the sinus P waves
P wave: P waves may be difficult to identify because they can be buried in the preceding T wave. However, when visualized, their morphology is different from the sinus P waves
LGL Syndrome • LGL, one type of PSVT, is usually benign unless debilitating tachyarrhythmias occur. ECG criteria are normal except that PR intervals are abnormally short but constant.
WPW Syndrome • WPW occurs mostly in younger patients (20–35 years old). It usually requires no intervention unless debilitating tachyarrhythmias occur.
ECG criteria are:
 Rate and rhythm: Within normal limits; however, WPW can predispose to abrupt episodes of PSVT, atrial fibrillation, or atrial flutter with rates up to 300 bpm
Rate and rhythm: Within normal limits; however, WPW can predispose to abrupt episodes of PSVT, atrial fibrillation, or atrial flutter with rates up to 300 bpm
 PR interval: Short
PR interval: Short
 QRS interval: Duration is prolonged. Beginning of the waveform is slurred (delta wave)
QRS interval: Duration is prolonged. Beginning of the waveform is slurred (delta wave)
ATRIAL FIBRILLATION/ATRIAL FLUTTER
Atrial fibrillation is a type of supraventricular arrhythmia defined as an extremely rapid and disorganized atrial activation (400–600 atrial bpm). This occurs when other ectopic foci in the atrium take over the role of the sinus node as the pacemaker. Such disorganized atrial contractions lead to a supraventricular impulse penetrating the AV conduction system in variable degrees, resulting in a totally irregular, often rapid ventricular rate. Because the AV node is composed of mostly slow conduction channels compared to the atrial tissue, which is composed of mostly fast conduction channels, most of the supraventricular impulses are not conducted through the AV node. Therefore, although the atrial rates usually vary between 400 and 600 bpm, the ventricle responds at a considerably slower rate (120–180 bpm).
Atrial fibrillation is now believed to occur under certain distinct clinical circumstances:
 As a secondary arrhythmia in the absence of structural heart disease but in the presence of systemic abnormalities that predispose the patient to atrial fibrillation
As a secondary arrhythmia in the absence of structural heart disease but in the presence of systemic abnormalities that predispose the patient to atrial fibrillation
 As a secondary arrhythmia associated with cardiac diseases that affect the atria
As a secondary arrhythmia associated with cardiac diseases that affect the atria
 As an idiopathic primary arrhythmia (lone atrial fibrillation)
As an idiopathic primary arrhythmia (lone atrial fibrillation)
The etiology of atrial fibrillation is categorized in Table 7.3 (Benjamin et al., 1994).
Any situation that leads to an increase in atrial mass, atrial dilatation (in fluid overload states), myocardial injury (in coronary artery disease), increased vagal tone, or any other disturbance to the atria (open heart surgery) increases the risk of developing atrial fibrillation.
Atrial flutter is another form of supraventricular arrhythmia. Atrial flutter occurs less frequently than atrial fibrillation but has similar precipitating factors, consequences, and approach to treatment. This arrhythmia is characterized by rapid but regular atrial activation (250–350 bpm). The ventricular rate is determined by AV nodal conduction and is some dividend of the atrial rate. For example, for an atrial rate of 300 bpm, the ventricular rate would be 100 bpm for a 3:1 AV conduction, 150 bpm for a 2:1 AV conduction, and 300 bpm for a 1:1 AV conduction. Atrial flutter usually occurs in conjunction with atrial fibrillation; in this situation, the ventricular rate will be irregular.
Etiologies of Atrial Fibrillation |
SYSTEMIC ABNORMALITY |
Hyperthyroidism Pulmonary disease (asthma, chronic obstructive pulmonary disease, pneumonia, pulmonary emboli) Cerebrovascular disease Fluid overload state Electrolyte abnormality Febrile illness Trauma and stress Alcohol Drugs: theophylline, caffeine |
CARDIAC DISEASES |
Cardiomyopathy Rheumatic or nonrheumatic valvular disease Tumor, lipomatous hypertrophy Atrial septal defect Coronary artery disease Pericarditis Cardiothoracic surgery |
OTHER CAUSES |
Hypertension Increased vagal tone |
Symptoms of atrial fibrillation and atrial flutter are similar. Patients often present complaining of palpitation, dizziness, fatigue, and dyspnea, especially if they have a rapid ventricular rate. Patients with a relatively slower ventricular rate may be asymptomatic. A prolonged uncontrolled ventricular rate may lead to cardiac decompensation or heart failure. Atrial fibrillation is usually categorized as paroxysmal or chronic and the management approaches are different. Atrial flutter, in contrast, is an unstable rhythm and rarely remains chronic.
ECG criteria for atrial fibrillation are:
 Rate: Atrial rate usually >400 bpm. Ventricular rates usually range from 100 to 150 bpm but can be <100 bpm
Rate: Atrial rate usually >400 bpm. Ventricular rates usually range from 100 to 150 bpm but can be <100 bpm
 Rhythm: Irregularly irregular
Rhythm: Irregularly irregular
 P wave: No P wave
P wave: No P wave
ECG criteria for atrial flutter are:
 Rate: Atrial rate is rapid and around 250 to 350 bpm. Ventricular rate depends on degree of AV block (usually between half to one quarter of the atrial rate
Rate: Atrial rate is rapid and around 250 to 350 bpm. Ventricular rate depends on degree of AV block (usually between half to one quarter of the atrial rate
 Rhythm: Regular
Rhythm: Regular
 P wave: Saw-toothed, referred to as “flutter wave”
P wave: Saw-toothed, referred to as “flutter wave”
BRADYARRHYTHMIAS AND HEART BLOCK
Bradyarrhythmia usually refers to sinus bradycardia. Sinus bradycardia is an arrhythmia where the sinus rate is below 60 bpm and all impulses come from the SA node. The morphology of the ECG is normal except a demonstration of a very slow ventricular rate. Sinus bradycardia is usually observed in athletes, most likely due to their increase in vagal tone. It is also noted during sleep, elevation of intracranial pressure, and situations with increased vagal tone such as straining of stool, vomiting, intubation, sick sinus syndrome, and hypothyroidism. Certain medications, such as beta-blockers, calcium channel blockers, and adenosine, may also induce sinus bradycardia.
Heart block or AV block is defined as a delay or interruption in the transmission of an impulse from the atria to the ventricles due to an anatomical or functional impairment in the conduction system. The conduction disturbance can be transient or permanent. Common causes of heart block can include increased vagal tone, fibrosis of the conduction system, ischemic heart disease, or drug induction (e.g., by digitalis, calcium channel blockers, beta-blockers). The commonly used terminology includes first-degree (slowed conduction without loss of AV synchrony, reflected in the ECG by a prolonged PR interval), second-degree (intermittent loss of AV conduction, often in a regular pattern, e.g., 2:1, 3:2, or higher degrees of block), and third-degree or complete AV block. Second-degree heart block can be divided into Types 1 and 2. Type 1 second-degree heart block (or Wenkebach block) is specifically characterized by increasing delay of AV nodal conduction until a P wave fails to conduct through the AV node. This is seen as progressive PR interval prolongation with each beat until a P wave is not conducted. There is an irregular RR interval as well. In Type 2 second-degree heart block, the PR interval may be normal or prolonged; however, it is constant in length, unlike Wenckebach block in which the PR interval progressively lengthens until a P wave is not conducted.
ECG criteria for bradycardia are:
 Rate: <60 bpm
Rate: <60 bpm
 Rhythm: Regular
Rhythm: Regular
ECG criteria for first-degree heart block are:
 Rate: May be normal or slow
Rate: May be normal or slow
 Rhythm: Regular
Rhythm: Regular
 PR interval: Prolonged
PR interval: Prolonged
ECG criteria for second-degree heart block are:
 Rate: May be normal or slow
Rate: May be normal or slow
 Rhythm: Irregular
Rhythm: Irregular
 PR interval:
PR interval:
 Type 1: progressive PR interval prolongation with each beat until a P wave is not conducted
Type 1: progressive PR interval prolongation with each beat until a P wave is not conducted
 Type 2: PR interval may be normal or prolonged; occasional P wave not conducted
Type 2: PR interval may be normal or prolonged; occasional P wave not conducted
ECG criteria for third-degree heart block are:
 Rate: May be normal or slow
Rate: May be normal or slow
 Rhythm: Irregular
Rhythm: Irregular
 PR interval: Normal or prolonged. Atrial-ventricular dissociation
PR interval: Normal or prolonged. Atrial-ventricular dissociation
Ventricular Arrhythmias
PREMATURE VENTRICULAR CONTRACTIONS
PVCs are ectopic ventricular beats that occur earlier than the normally expected beat and are often followed by a compensatory pause. PVCs may be uniform, arising from the same ectopic focus (unifocal); or multiform (multifocal), arising from two or more different ventricular sites. Patients experiencing PVCs may be asymptomatic or may complain of “skipping beats.” Depending on a patient’s ventricular function and the duration and frequency of the PVCs, a decrease in cardiac output may result. PVCs are more dangerous if they occur in the presence of heart disease. Possible causes of PVCs include digitalis toxicity, hypokalemia, hypocalcemia, and the use of caffeine and other stimulants.
The ECG criterion is a QRS interval that is wide and bizarre in morphology. Although most PVCs are benign, certain forms of PVCs may be predictive of potentially serious arrhythmic events (e.g., sustained VT). Potentially dangerous PVCs include:
 Couplets, triplets, or more PVCs in a row
Couplets, triplets, or more PVCs in a row
 Bigeminy (every other beat is a PVC) and trigeminy (every third beat is a PVC)
Bigeminy (every other beat is a PVC) and trigeminy (every third beat is a PVC)
 Multifocal PVCs (PVCs with different morphologies)
Multifocal PVCs (PVCs with different morphologies)
 More than six PVCs in a minute
More than six PVCs in a minute
 R-on-T phenomenon: The PVC falls on the preceding beat’s T wave. This type of PVC can lead to VT and VF
R-on-T phenomenon: The PVC falls on the preceding beat’s T wave. This type of PVC can lead to VT and VF

Full access? Get Clinical Tree