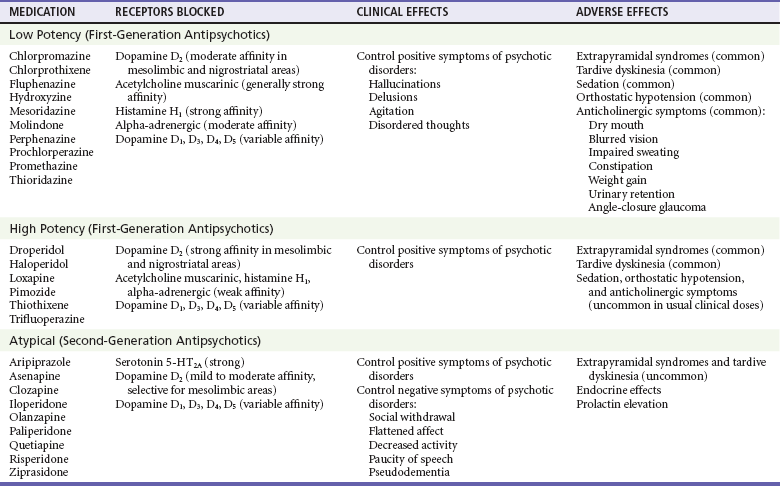
Chapter 161 The first antipsychotic, chlorpromazine, was used for the treatment of psychosis in France in 1951 and in the United States in 1954. Antipsychotic use has expanded significantly since then. The historic term neuroleptic, used with antipsychotic medication, is no longer appropriate because newer agents cause less sedation. The term antipsychotic is now preferred. In 2009, U.S. poison control centers reported more than 4700 exposures to phenothiazines and 43,000 exposures to atypical antipsychotics, resulting in 0 and 8 deaths, respectively.1 Antipsychotic medications are used to treat agitation and psychosis caused by schizophrenia, mania, acute idiopathic psychosis, substance-induced psychosis, and dementia. The antipsychotic medications are divided into three broad categories on the basis of their receptor profiles, clinical effects, and adverse effects (Table 161-1). All antipsychotic medications effectively treat the positive symptoms of psychotic disorders; they reduce hallucinations, control agitation, and aid in restructuring of disordered thinking. In general, the low-potency first-generation antipsychotics (FGAs) are the most sedating. Movement disorders, including extrapyramidal symptoms (EPS) and tardive dyskinesia (TD), are significant problems with both low-potency and high-potency FGAs. In addition to producing less sedation and fewer movement disorders, the atypical or second-generation antipsychotics (SGAs) assist with the negative symptoms of psychotic disorders, such as flat affect, avolition, social withdrawal, and impoverished thought and speech.2 Although neuroleptic malignant syndrome (NMS) occurs with all agents, it occurs least with SGAs. Antipsychotic drugs block dopamine receptors in several areas of the brain, including the cerebral cortex, basal ganglia, limbic system, hypothalamus, and chemoreceptor trigger zone. All antipsychotic agents reduce the positive symptoms of schizophrenia by blocking the dopamine D2 receptor subtype in the mesolimbic region of the brain. However, blockade of D2 receptors in the nigrostriatal brain region produces undesired EPS. In addition, blockade of D2 receptors in the mesocortical brain region impairs cognition and worsens the negative symptoms of schizophrenia. SGAs block both D2 and serotonin 5-HT2A receptors. Because these agents have lower affinity for dopamine receptor antagonism and more selective binding of D2 receptors in the mesolimbic versus nigrostriatal areas of the brain, SGAs should have a lower rate of EPS and TD. The serotonin receptor antagonism is thought to reduce EPS effects and to improve the negative symptoms of schizophrenia.3,4 However, studies have found no significant difference in reported rates of EPS and TD between perphenazine (a FGA) and several SGAs.5,6 Antipsychotic medications also block other receptor types (see Table 161-1). EPS can be immediate or delayed after initiation of drug therapy. The acute EPS include dystonia, akathisia, and parkinsonism, which are caused by blockade of nigrostriatal D2 receptors and reduced by blockade of muscarinic receptors. The propensity for antipsychotics to produce EPS is inversely proportional to the agents’ muscarinic receptor antagonism.4 The delayed-onset syndromes, including TD and tardive dystonia, develop after prolonged use of antipsychotic medications and are thought to occur from chronic dopamine receptor blockade in the nigrostriatal area leading to D2 receptor upregulation and hypersensitivity to dopamine.7–9 The pathophysiologic mechanism of NMS, an idiosyncratic reaction to antipsychotic medication, is unknown but thought to be neuroregulatory dysfunction secondary to D2 receptor blockade in the nigrostriatum and hypothalamus, leading to rigidity and hyperthermia, respectively.10 NMS is not associated with ryanodine receptor (RYR) gene mutations, which are associated with malignant hyperthermia. Antipsychotic medications produce cardiovascular side effects, most commonly orthostatic hypotension with reflexive tachycardia due to alpha-adrenergic blockade. Many agents cause conduction delays, predominantly QT prolongation, resulting in prolonged repolarization and potentially torsades de pointes (TdP).11 The degree of prolongation varies between antipsychotic agents, increasing with dose and with concomitant use of other drugs that prolong the QT interval.12,13 The phenothiazines, particularly thioridazine and mesoridazine, have the greatest risk of cardiac toxicity. QT prolongation has also been reported with the butyrophenones haloperidol and droperidol.12,14 The atypical antipsychotics produce less cardiotoxicity than the traditional agents do, although most can cause repolarization abnormalities in therapeutic doses and overdose.12,15,16 Ultimately, a correlation between QT prolongation and dysrhythmias or TdP has not been established,3 but antipsychotics are associated with an increased risk of sudden death, particularly with heart disease and in elderly patients.17,18 However, psychotic disorders themselves are associated with an increased risk of sudden death. Clozapine produces agranulocytosis in 1 or 2% of treated patients; however, this has been reduced to 0.4% after strict adherence to labeling requirements.19 Although the mechanism of agranulocytosis is unknown, research supports an immunogenic cause and direct cytotoxic effect on human bone marrow mesenchymal stromal cells.20 Seizure rarely occurs with antipsychotic drugs, but clozapine has the highest seizure incidence. Drug dosing and the patient’s seizure risk profile influence seizure susceptibility.21 FGAs and SGAs have been associated with weight gain, glycemic dysregulation, and dyslipidemia. The cause is not fully understood but partly blamed on the pharmacodynamic profile of these agents.22 Atypical antipsychotic overdose is similar to that of traditional antipsychotics. Overdoses are characterized by CNS depression and tachycardia.23–30 Miosis may be present, potentially mimicking opioid toxicity.31 Extremity twitching is common. With the exception of clozapine, seizures rarely occur in overdose. Acute EPS have been reported, especially for risperidone overdose.32 Acute dystonia is manifested as intermittent, involuntary motor tics or spasms of antagonistic muscle groups that most often involve the facial, neck, back, or limb muscles. This results in trismus, facial grimacing, dysarthria, tongue and lip distortion, torticollis, or oculogyric crisis. Dystonic reactions usually develop within the first several doses of treatment or after a large increase in dosage.33 Laryngeal dystonia is a rare but life-threatening form of dystonia that is manifested as stridor, difficulty in breathing, or choking sensation.5,34 Increased risk of death due to choking has been documented in schizophrenia patients.35 Akathisia is a subjective feeling of restlessness associated with objective motor restlessness, including repetitive foot shuffling, truncal rocking, or pacing. The subjective distress may precipitate aggressive behavior.5,36 Akathisia usually develops within the first few days of treatment, but 40% of patients given 10 mg of intravenous prochlorperazine developed akathisia within 1 hour.37 A parkinsonian syndrome of bradykinesia, masked facies, shuffling gait, muscle rigidity, and resting tremor frequently develops during the first month of treatment; 90% of cases occur within 3 months of treatment. Perioral tremor (rabbit syndrome), in which the lip and nose movements resemble those of a rabbit, can also develop after prolonged therapy.5 TD is a chronic movement disorder induced by prolonged use of antipsychotic medication. Typical signs of TD include quick, involuntary movements of the face (blinking, grimaces, tongue movements, and chewing), extremities, or trunk. Twenty percent of patients treated with long-term traditional antipsychotics are affected. TD is difficult to treat and is frequently permanent. Anticholinergic agents may worsen TD; reduction of the antipsychotic dose or a change to an alternative agent should be considered.5,38 TD improves in some patients switched to clozapine; amantadine improved symptoms compared with placebo in a small study.39,40
Antipsychotics
Perspective
Principles of Disease
Anatomy and Physiology
Pathophysiology
Clinical Features
Acute Extrapyramidal Syndromes
Tardive Dyskinesia

Full access? Get Clinical Tree