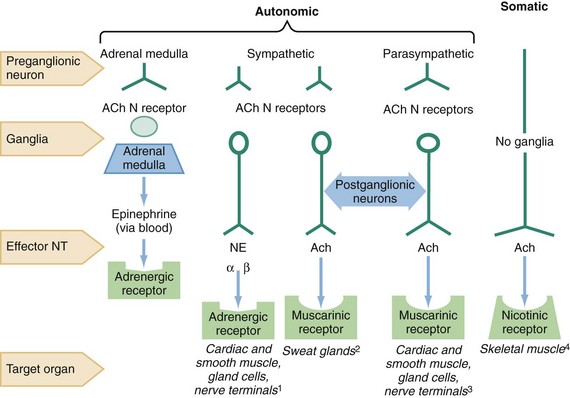
Chapter 150 Anticholinergic agents are divided into three main groups: antimuscarinics, affecting the muscarinic acetylcholine (ACh) receptors; neuromuscular blockers, blocking nicotinic ACh receptors; and ganglionic blockers, affecting ACh sympathetic and parasympathetic nicotinic ganglia (Fig. 150-1). This chapter refers only to antimuscarinic agents, and the terms anticholinergic and antimuscarinic are used interchangeably. The prototypical anticholinergic agents are the naturally occurring belladonna alkaloids—atropine (racemic mixture of D– and L-hyoscyamine), scopolamine (L-hyoscine), and hyoscyamine—found in many plant members of the Solanaceae family. Atropine is the major alkaloid of Atropa belladonna, an important pharmaceutical source of that drug. Datura stramonium, or Jimson weed, contains scopolamine, grows in almost all climates, and is often involved in plant-related belladonna poisoning.1,2 Other plants that have antimuscarinic agents include henbane (Hyoscyamus niger) and mandrake (Mandragora officinarum). Figure 150-1 The sites of nicotinic and muscarinic acetylcholine receptors. Ach, acetylcholine; N, nicotinic; NE, norepinephrine; NT, neurotransmitter.1 Causing tachycardia, hypertension, diaphoresis, mydriasis.2 Causing diaphoresis.3 Causing bradycardia, diarrhea, diaphoresis, urination, miosis, bronchospasm, bronchorrhea, lacrimation, salivation.4 Causing fasciculations. Physicians (and Renaissance-era Italian women) have used belladonna alkaloids for hundreds of years as mydriatics (Box 150-1).3 The belladonna alkaloids and their synthetic congeners are used today as pupillary dilators (atropine, homatropine, tropicamide, cyclopentolate), as antispasmodics (dicyclomine), to decrease gastric secretions (propantheline), to prevent motion sickness (scopolamine), and to treat asthma (ipratropium, tiotropium) and bradycardia (atropine). Atropine and glycopyrrolate are used to dry airway secretions and to block vagal responses to laryngoscopy and endotracheal intubation. The significant central nervous system (CNS) effects of scopolamine also facilitate the induction of perioperative amnesia. Many other drugs with anticholinergic activity cause side effects in addition to their main pharmacologic action. Some examples are the tricyclic antidepressants, drugs that are structurally related to the tricyclics (such as carbamazepine and cyclobenzaprine), the phenothiazines, and the antihistamines (H1 blockers). In patients with significant toxicity from any of these drugs, these antimuscarinic side effects provide valuable diagnostic clues (Box 150-2; see also Box 150-1). Accidental and intentional poisoning by anticholinergic drugs occurs commonly with over-the-counter antihistamines such as diphenhydramine and cyclizine. Poisoning from drugs with only anticholinergic effects rarely results in death when adequate supportive care is provided. However, the impaired sweating with an anticholinergic overdose may result in fatal hyperthermia in the agitated or seizing patient.4,5 Patients taking therapeutic doses of anticholinergics are at increased risk of death from heatstroke when they are exercising or exposed to heat. Finally, deaths from trauma or drowning caused by perceptual distortion are also attributed to anticholinergics.6 Poisonings with belladonna alkaloids are common. Deliberate ingestions of seeds or teas brewed from the leaves of the ubiquitous Jimson weed for their hallucinogenic effects occur in many cultures,1 and it remains popular as a recreational stimulant among teenagers.7 Commercially available herbal teas contaminated with atropine and smoking of herbal cigarettes cause inadvertent poisoning.8,9 A cluster of poisonings occurred in Oslo when the difficult-to-detect drug scopolamine was disguised as Rohypnol tablets and given to known illicit drug users.10 The tainting of heroin with anticholinergics leading to a complex toxidrome has also been reported in drug users in several eastern states of the United States.4,5 Although the reason for this tainting was never explained, it may have been an attempt to reproduce an old combination of scopolamine and morphine used in obstetric anesthesia called the twilight sleep.11 Atropine and atropine-like drugs inhibit muscarinic ACh receptors both centrally and peripherally at the end-organ sites of the parasympathetic nervous system (see Fig. 150-1). Although the term anticholinergic is commonly used, the most precise term to describe the pharmacologic action of these drugs is antimuscarinic. These drugs do not block the effects of ACh on nicotinic receptors in the ganglia or at the neuromuscular junction, with the exception of the synthetic quaternary amines. Muscarinic receptors affect smooth muscle function in the eye, intestinal tract, and bladder and also regulate sweat, salivary, and mucosal gland activity. Cardiac cholinergic receptors associated with vagal nerve fibers affect heart rate and conduction through the atrioventricular node. Muscarinic receptors in the CNS appear to be involved in new information storage, general perceptive and cognitive functions, and motor coordination.12–14 Generalized inhibition of muscarinic receptors by atropine results in tachycardia, pupillary dilation, loss of accommodation, inability to sweat, drying of mucosal surfaces, gastrointestinal paralysis, and urinary retention. In the CNS, muscarinic inhibition causes stimulation, seizures, coma, choreoathetosis, memory impairment, and perceptual and cognitive dysfunction.12–17 The mnemonic “hot as a hare, red as a beet, blind as a bat, dry as a bone, mad as a hatter” describes the more florid manifestations of the antimuscarinic syndrome. With increasing doses, CNS depression follows the initial CNS stimulation. In adults, CNS depression can predominate without an initial CNS stimulation. Antimuscarinic effects occur in a predictable order with salivation, bronchial secretions, and sweating suppressed first, followed by mydriasis and tachycardia. The organs least sensitive to antimuscarinic drugs are the bladder and the gastrointestinal tract. Patients with anticholinergic toxicity often do not exhibit all the signs and symptoms described in the toxidrome. Instead, many patients present with just a few symptoms; tachycardia (68% of patients) and decreased secretions (75% of patients) are the most common.18 Poisoning by anticholinergics has been reported after ingestion, smoking, and topical absorption.19 Systemic absorption is common after use of eye drops.19,20 Anticholinergics are generally rapidly absorbed and widely distributed throughout the body. However, with plant and seed ingestions or after an overdose, the onset of symptoms can be delayed. Prolonged anticholinergic toxicity is also reported, which may indicate slowed gastrointestinal absorption of the ingested drug or residual drug in the gastrointestinal tract.21,22 The diagnosis of acute anticholinergic poisoning is suggested by the characteristic anticholinergic toxidrome. Mydriasis, dry mucous membranes, absence of axillary sweat, flushed skin, fever, tachycardia, decreased or absent bowel sounds, and urinary retention suggest muscarinic blockade.18,23 The patient is often alert but may be nonsensical, agitated, or incoherent. Violent agitation is rare. Visual hallucinations are common. Central motor effects may be manifested as myoclonus or choreoathetoid movements. Children are more sensitive than adults to the CNS stimulant effects and more likely to have seizures, typically preceded by signs of CNS irritability or depression. Massive ingestions in both adults and children are associated with coma and cardiovascular collapse,22,24 but wide-complex tachycardia due to sodium channel blockade is rare.25,26 The agitated patient may have an elevated temperature due to increased motor activity and impaired heat exchange. In such cases, death from hyperthermia supersedes the morbidity of the anticholinergic drug itself.27 The hyperthermic patient may have hepatic necrosis, rhabdomyolysis with myoglobinuric renal failure, cerebral edema, and disseminated intravascular coagulation. Patients with chronic anticholinergic poisoning are more difficult to diagnose. They have organic mental symptoms that may be incorrectly attributed to dementia or underlying psychiatric illness.16,28,29 Significant peripheral anticholinergic signs are typically absent. Two likely settings for chronic anticholinergic toxicity are (1) the elderly patient taking anticholinergic drugs for parkinsonism or other chronic diseases and (2) the psychiatric patient receiving neuroleptic therapy and prescribed another anticholinergic drug.12,16 Resolution of behavioral or cognitive symptoms after withdrawal of the offending drug confirms the diagnosis.
Anticholinergics
Perspective
Principles of Disease
Clinical Presentation
Anticholinergics
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






