UNIT IX: MUSCULOSKELETAL CONDITIONS
CHAPTER 39
Anterior Knee Pain
Sanjiv Bansal, MD • Kathleen T. Roche, RN, FNP, PA-C MPA • William Urban, MD
Anterior knee pain is a common musculoskeletal complaint seen by primary care providers. It describes a large spectrum of clinical entities whose predominant symptoms include pain from the patellofemoral joint and surrounding structures. The term “anterior knee pain” can be used to describe primary painful syndromes as well as pain secondary to instability of the patellofemoral articulation. Diseases discussed in this chapter include patellofemoral (pain) syndrome, the most common cause of anterior knee pain seen in primary care settings, as well as other entities such as bursitis, septic and inflammatory arthritis, patellar tendinopathy, and Osgood–Schlatter disease. Acute traumatic injuries are not discussed.
This chapter focuses on painful syndromes of the patellofemoral joint. The term patellofemoral syndrome is used to encompass all the pain-causing problems of this joint except those secondary to instability. It is imperative to determine the exact etiology of anterior knee pain to develop a precise and effective treatment protocol.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
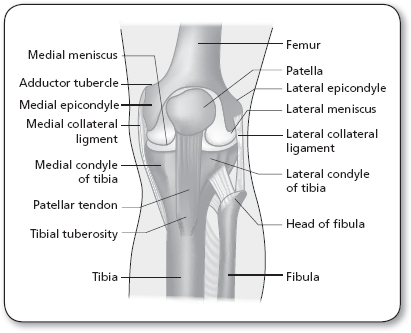
Patellofemoral Joint Anatomy
The patellofemoral joint consists of the femoral trochlear and the patellar articular surface. The trochlear surface or sulcus is divided into medial and lateral condyles, by which the patella articulates with the femur (Figures 39.1 and 39.2). The lateral condyle is higher than the medial and helps prevent lateral subluxation of the patella. The femoral sulcus is flatter proximally than distally. As it deepens distally, the femoral sulcus provides greater conformity for the patella. There is a greater propensity for the patella to subluxate or dislocate in extension than in flexion, where it is captured in the femoral sulcus.
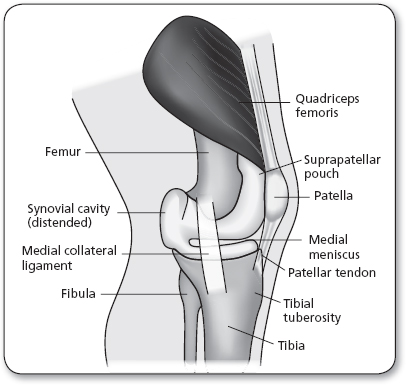
The patella is the largest sesamoid bone in the body and has the thickest articular surface. As a sesamoid bone, the patella should not be considered as a separate osseous structure, but should be viewed in the context of the entire extensor mechanism. It is divided into lateral and medial facets by the middle ridge or crest. The extensor mechanism begins proximally at the pelvis at the insertion of the rectus femoris. The mechanism is responsible for dynamic control of the patellofemoral joint in the superior–inferior plane. The vastus medialis oblique (VMO) muscle inserts into the superomedial aspect of the patella. It is the primary dynamic force responsible for medial movement of the patella and is important in stabilizing the patella both in extension and in internal rotation of the femur on the tibia. The vastus lateralis and part of the iliotibial band (ITB) provide the lateral dynamic force. Static constraints include the conformity of the facets within the sulcus of the femur and the patellofemoral ligaments. These ligaments represent thickening in the capsule medially and laterally. They are located both inferiorly and superiorly on the medial and lateral patella. They extend from the anterior surface of the patella to the posterior aspect of the femoral condyles.
Biomechanics of the Patellofemoral Joint
The patella’s most important function is to facilitate extension of the knee by biomechanically increasing the movement arm. The patella increases the quadriceps strength by as much as 50%. The patella protects the patellar and the quadriceps tendons against large shear and compressive forces. In full extension, the patella sits at the proximal aspect of the trochlear against the suprapatellar fat pad. As the knee flexes, the patella first articulates with the trochlear groove at about 10° in patients with normal patellar tendon length. On increasing knee flexion, the lateral facet contacts the lateral trochlear and the medial facet contacts the medial trochlear at 20° of flexion. With increased knee flexion, the patellar contact area increases and shifts proximally. At 90° of flexion, the patella enters the condylar fossa, where the contact areas are on both the lateral and medial trochlears of the femur. At 135° of knee flexion, the odd facet of the patella contacts the trochlear.
 EPIDEMIOLOGY
EPIDEMIOLOGY
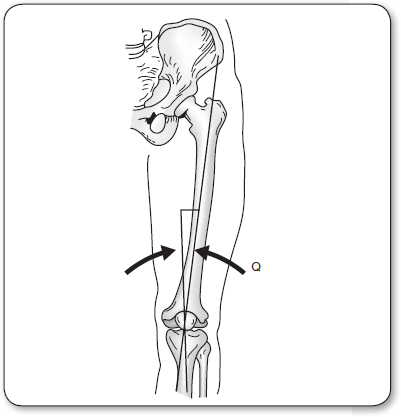
Approximately 10% of adults presenting to primary care providers with musculoskeletal complaints have anterior knee pain. Etiology varies with age groups. Osteoarthritis is more common in older patients. Patellofemoral pain syndrome is more common in a sports medicine practice. Anterior knee pain is most common in young adults, runners, and women. Women appear to be more often affected than men because of the gynecoid pelvis, which increases their Q angle (the Q angle is formed by a line drawn from the anterior superior iliac spine of the pelvis to the center of the patella and from the center of the patella to the tibial tubercle). Racial or ethnic risk factors have not been identified for most causes of anterior knee pain.
 HISTORY AND PHYSICAL EXAMINATION
HISTORY AND PHYSICAL EXAMINATION
Patients with anterior knee pain complain of pain, crepitus, “giving way,” locking, and swelling of the knee. The quality of pain must be assessed. Pain may be described as sharp, dull, burning, or aching. Patients can usually locate the pain to the kneecap, but complaints of pain referred to the back of the knee are not uncommon. The pain is worse on increased knee flexion, especially when sitting for a prolonged period. The pain is exacerbated on ascending and descending stairs. The level of pain should be assessed by discerning whether the pain prevents patients from performing activities they enjoy.
Crepitus is a common finding even in normal knees. It should be considered significant only if it is associated with pain. Crepitus in patients with anterior knee pain could be secondary to synovitis, quadriceps tendon, or chondrosis.
After a careful history, a thorough examination should be done, not only of the knee joint but also of the hip and ankle as well. Referred pain from the hip and ankle can present as patellofemoral pain. The patient must be examined walking, standing, sitting, and in supine, prone, and functional positions. Examine the hip and ankle first before proceeding to the more painful knee joint. The physical exam should begin with inspection of the patient (Table 39.1).
Inspection
When examining the patient, shoes, socks, and clothing should be removed to allow clear visualization of the entire pelvis and lower extremity. Observe the gait carefully as the patient enters the examining room. Limping could signify weak abductors, leg length inequality, or a painful joint in the lower extremity.
Standing Examination
During this phase, examine both legs. Standing alignment should be assessed for any pelvic, femoral, tibial, or pedal abnormalities that could alter the biomechanics of the knee and cause patellofemoral pain. Examine the pelvis first. The Q angle must be assessed (Figure 39.3). The normal Q angle is 8° to 10° for a man and 10° to 20° for a woman. Women have a broader pelvis, which increases the Q angle. An increased Q angle indicates an increase in a laterally directed force on firing of the extensor mechanism. These patients frequently have malrotation of the patella with subluxation.
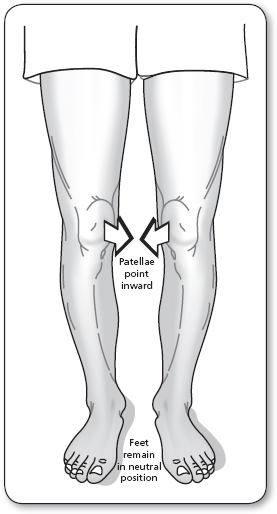
Next, examine the femur. The femur is normally slightly anteverted. With the feet in neutral position, the patella should point straight ahead. With increased anteversion, there is increased internal rotation of the hip, which increases the Q angle. This results in an inward-pointing patella, described as the “squinting” patella (Figure 39.4). Femoral anteversion should be evaluated by examining the hip for increased internal rotation when in supine and prone positions.
Physical Examination |
OBSERVATION |
Gait: limping—weak abductors, painful joint or leg length discrepancy Muscular atrophy Joint effusion |
STANDING EXAMINATION |
Alignment Q angle Hip: femoral version Knee: genu varum, valgum, recurvatum or flexion Ankle/feet: valgus hindfoot or pronated foot Ankle equinus |
SITTING EXAMINATION |
Observe for muscular atrophy Measure quadriceps girth Patella position: upward—patella alta; camelback sign |
SUPINE EXAMINATION |
Examine for pain, swelling, masses, instability, or defect Palpate knee joint; be systematic Q angle Tubercle—sulcus angle Patellofemoral grind test—chondromalacia patellae Passive patellar tilt and glide Ober test—ITB tendinitis Lachman, anterior drawer, and pivot shift tests—anterior cruciate laxity Posterior drawer and reverse pivot shift—posterior cruciate laxity Varus and valgus stress test in 0° and 30° of knee flexion 0—LCL and MCL laxity McMurray and Apley test—meniscus pathology |
PRONE EXAMINATION |
Quadriceps muscle tightness Hip rotation—femoral version |
ITB, iliotibial band; LCL, lateral collateral ligament; MCL, medial collateral ligament.
Examine the vastus medialis muscle and its insertion area for any atrophy that may help in making a diagnosis of patellofemoral disorder.
Examine the knee for genu varum (bowed legs), genu valgum (knock knees), or genu recurvatum (back knees). Genu valgum increases the Q angle and may cause patellar subluxation and lateral patellar compression syndrome. Patients may have unilateral or bilateral genu recurvatum. Those with bilateral genu recurvatum should be examined for generalized ligamentous laxity. Patients with unilateral genu recurvatum should be evaluated for possible anterior or posterior cruciate ligament insufficiency. Patients with a flexion contracture of the knee may have an untreated displaced meniscus tear, fat pad syndrome (Hoffa’s disease), hamstring tightness, or contusion. Flexion increases the patellofemoral contact pressures and leads to patellofemoral syndrome.
Next, assess the tibia for rotation. Tibial rotation is evaluated with the patella pointing straight and the examiner looking at the direction the feet are pointing. The feet should be in neutral position. If they are pointing outward, then the patient has external tibial torsion; if the feet are pointing inward, then the patient has internal tibial torsion. In patients with external tibial torsion, the tibial tubercle moves laterally and the Q angle increases. This increases the risk of patellar subluxation and lateral patellar compression syndrome. Internal tibial torsion is generally not associated with patellofemoral disorders.
FIGURE 39.3
The quadriceps angle (Q angle) is formed by a line drawn from the superior iliac spine of the pelvis to the center of the patella and from the center of the patella to the tibial tubercle.
Source: Adapted from Palmer and Epter (1998).
Finally, examine the ankles and feet. Valgus hindfoot, as in pronated foot, may be associated with genu valgus. This increases the Q angle and leads to patellofemoral pain. In addition, pronated feet may lead to internal tibial torsion, which causes increased femoral anteversion and increased patellofemoral pressure. Equinus deformity of the ankle, as in a tight Achilles tendon, may cause anterior knee pain by placing the knee in hyperextension during the stance phase of walking (Scuderi, 1995).
Sitting Examination
Examine both legs as they hang loosely over the table. Look for asymmetrical muscular atrophy, and measure the girth of the quadriceps muscles on both legs at consistent locations.
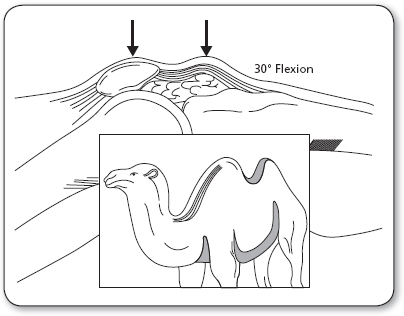
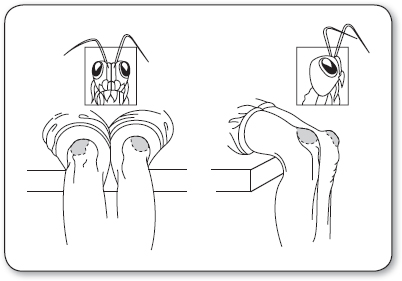
Normally, the patella points straightforward, but in patients with a high-riding patella (patella alta), the patella points upward. In these patients, there is a prominence of the infrapatellar fat pad in extension that gives the knee a double prominence when viewed from the side; this is known as the camelback sign (Figure 39.5). These patients tend to have more patellofemoral symptoms because of the increased laxity at the patellofemoral joint. In addition, some patients with proximally riding patellae also have externally rotated patellae consistent with patella alta and lateral tilt. This is known as the “grasshopper eyes” sign (Figure 39.6).
FIGURE 39.4
Squinting patellae. Rotational malalignment of the limb leads to an increased Q angle.
Source: A dapted from Scuderi (1995).
The normal medial and lateral depression at the level of the inferior and superior poles of the patella may not be appreciated if an effusion is present. To confirm the presence of an effusion, the knee should be milked and palpated. A large effusion may allow the patella to be balloted. If swelling is present over the patellar tendon, then the patient may have patellar tendinitis or prepatellar bursitis. The tibial tubercle should be evaluated for any prominence or tenderness that would suggest chronic patellar tendinitis in the adult.
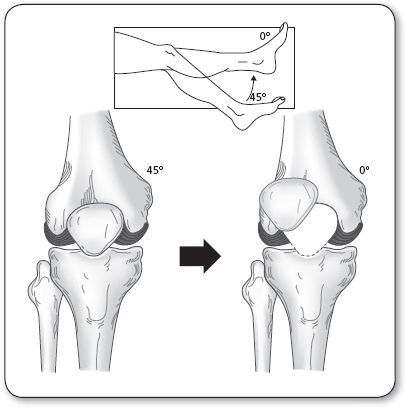
Range of motion is assessed both passively and actively. A normal range of motion of the knee is –5° to 0° of extension to 120° to 135° of flexion. Active and passive range of motion are documented and compared to the nonpainful knee. While testing range of motion, document any abnormal tracking of the patella or any patellofemoral crepitus. Normally, the patella engages the femoral sulcus at 30° to 40° of flexion. At terminal extension, the patella may subluxate or jump laterally, which is referred to as the J sign (Figure 39.7). This usually indicates excessive pull by the vastus lateralis because of a weak vastus medialis.
FIGURE 39.5
Camelback sign. Prominence of the infrapatellar fat pad is often associated with patella alta.
Source: Adapted from Scuderi (1995).
FIGURE 39.6
Grasshopper eyes. Proximal- and lateral-facing position of the patella associated with patella alta and lateral tilt.
Source: Adapted from Scuderi (1995).
Supine Examination
In the supine examination, the patellofemoral area is systematically examined for pain, swelling, mass, instability, and defect. The entire joint is palpated (see Table 39.1). The Q angle is measured and documented. An increased Q angle alone is not a reliable indicator of patellar malalignment. The Q angle is greatest in full extension; a Q angle with the knee flexed is more significant.
FIGURE 39.7
The J sign. Lateral deviation of the patella with terminal extension rather than normal straight proximal line of pull.
Source: Adapted from Scuderi (1995).
The patellofemoral grind test is performed as the provider gently compresses the patella against the femoral sulcus and then has the patient contract the quadriceps. Any pain elicited on compression may signify articular injury, such as chondromalacia patellae. To increase specificity, the test should be performed again in 30° of flexion, because the grind test may be positive in an asymptomatic knee.
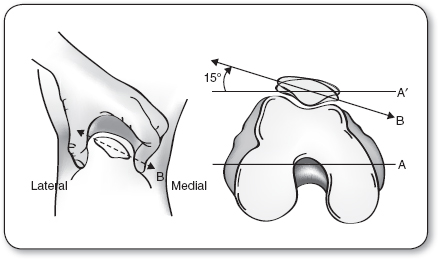
Assessments of passive patellar tilt and glide are important to determine the mobility of the patella. The passive patella tilt test evaluates the tightness of the lateral retinaculum (Figure 39.8). With the patient supine and the quadriceps fully relaxed, the patella is grasped between the examiner’s index finger and thumb at the midportion of the patella. The amount of upward tilt of the patella laterally is assessed. The normal tilt is 0°. A neutral tilt angle is one in which the lateral patellar edge is parallel to the floor. A negative tilt of <0° is consistent with an excessively tight lateral retinaculum and elevated lateral pressure syndrome. This should be compared to the asymptomatic knee. A passive patella glide test indicates medial or lateral retinacular laxity or tightness (Figure 39.9). With the quadriceps relaxed and with the knee supported in 30° of flexion, the patella is displaced medially or laterally. Considering the patella in four longitudinal quadrants, a lateral glide of three or more quadrants indicates an incompetent medial retinaculum (a medial glide of one quadrant or less is consistent with a tight lateral retinaculum or excessive lateral pressure syndrome [ELPS]). When the patella displaces medially three or more quadrants, a hypermobile patella is diagnosed, the result of congenital disorders or lateral retinacular release.
The patella can also be in a laterally tilted position if there is a tight ITB. Normally, the ITB falls posteriorly when the knee is flexed. With a tight ITB, the fibers attaching to the lateral retinaculum increase the pull between the patella and the ITB when the knee is flexed; this causes a laterally tilted patella and will cause ELPS. The Ober test is used to evaluate ITB tightness (described in the section on ITB syndrome).
Each knee is tested for laxity of the anterior cruciate, posterior cruciate, medial collateral (MCL), and lateral collateral ligaments (LCL), and meniscal pathology by performing the appropriate tests. Patients with ligament insufficiency often complain of patellofemoral pain and of the knee “giving way.” It is vital to differentiate giving way from quadriceps inhibition and instability. Reflex inhibition of the quadriceps may be caused by an effusion or patellofemoral pain. The anterior cruciate ligament is tested by performing the Lachman test, anterior drawer test, and pivot shift test. The posterior cruciate ligament can be tested by performing the posterior drawer test and reverse pivot shift and looking for posterior sag when the knee is flexed 90°. The collateral ligaments are tested by applying either varus or valgus force to the knee in 0° and 30° of knee flexion. Both patellofemoral syndrome and meniscal pathology can cause joint line tenderness in the anterior third of the medial and lateral joint line. To evaluate the meniscus, provocative tests such as those described by McMurray (Figure 39.10) and Apley (Figure 39.11) should be performed. A palpable or audible click produced in the joint by the McMurray test suggests a posterior medial meniscus tear. Pain produced by the Apley test suggests a tear related to the location of pain.
Prone Examination
FIGURE 39.8
The passive patella tilt test. The inability to tilt the patella beyond a line parallel to the transepicondylar axis is consistent with a contracted lateral retinaculum. (A’, transepicondylar axis; A, patella horizontal to transepicondylar axis; B, patella tilted beyond horizontal.)
Source: Adapted from Scuderi (1995).

Full access? Get Clinical Tree