Cadaveric image of the sciatic nerve.
Many approaches to sciatic nerve blockade exist:
Labat (classical):
Anatomy. The patient is placed in the lateral position with the operative side exposed and non-dependent. A line is drawn from the GT to the posterior superior iliac spine (PSIS) and a second line from the GT to the sacral hiatus (SH). Finally, a third line is drawn perpendicular from the midpoint of the first line to the second line creating the needle insertion point [3].
Nerve stimulator. A stimulating needle is inserted perpendicular to all planes. Often a gluteal twitch is first observed and prompt needle advancement is recommended as this can be uncomfortable for the patient. Proper needle positioning and sciatic nerve localization is indicated with movement of the hamstring, calf, foot, or toes.
Ultrasound. Place a curvilinear, low-frequency (2–5 MHz) probe on a line between the GT and SH. The sciatic nerve will be visualized as a hyperechoic, wide, and flat structure below the gluteus maximus and over the ischial spine or ischial bone.
Clinical pearls:
A gluteal twitch indicates the needle is likely too superficial and should be advanced.
If the needle contacts bone without encountering a gluteal twitch, the practitioner should stop the procedure and re-evaluate surface anatomy.
If the needle contacts bone without encountering a sciatic twitch, the needle is most likely too medial or lateral and should be redirected in either fashion.
If the needle is placed deep without encountering a twitch or bone, the needle has likely passed through the sciatic notch and should be redirected superiorly.
Advantages/disadvantages. The Labat approach was the first technique described in the early 20th century. Patient positioning can be difficult with the obese population and those with fractures.
Parasacral:
Anatomy. The patient is placed in the lateral decubitus position with the operative side non-dependent. A line is drawn from the PSIS to the IT. Needle insertion is 8 cm below the PSIS on this line [4].
Nerve stimulator. Proper placement is confirmed with a sciatic twitch, movement of the hamstring, calf, foot, or toes.
Ultrasound. Using a curvilinear, low-frequency (2–5 MHz) US probe, identify the superior margin of the gluteal cleft. Place the probe perpendicular to the gluteal cleft. The bony structures of the ischium (lateral) and sacrum (medial) can be identified. The sciatic nerve will appear as a hyperechoic structure between the bony landmarks [5].
Clinical pearls:
Gluteal or obturator internus stimulation indicates that the needle is too superficial or lateral.
An obturator twitch (adduction of the hip) indicates that the needle is too medial and deep.
If bone is contacted, the needle should be redirected more caudally as it is likely in contact with the sacrum or the ischial bone.
Advantages/disadvantages. This technique carries similar limitations to the Labat approach, including patient positioning and difficulty with landmark identification. At the parasacral level, the nerve lies superficial to the ureter, sigmoid colon, and hypogastric vessels; therefore, inadvertent puncture is possible.
Subgluteal:
Anatomy. The patient is placed in either the lateral decubitus or prone position with the operative side exposed and the knees flexed. Franco et al. found a 100% success rate of locating the sciatic nerve 10 cm from the midline in the midgluteal region in adults, irrespective of gender or body size [6]. This approach also avoids the need to identify any deeper anatomic structures [6]. In contrast, Raj et al. described an approach with the patient in the supine lithotomy position with needle insertion at the midpoint of a line connecting the GT and IT [1].
Nerve stimulator. A line is drawn between the GT and IT. The needle is inserted at the midpoint of this line. Proper placement is confirmed by foot movement.
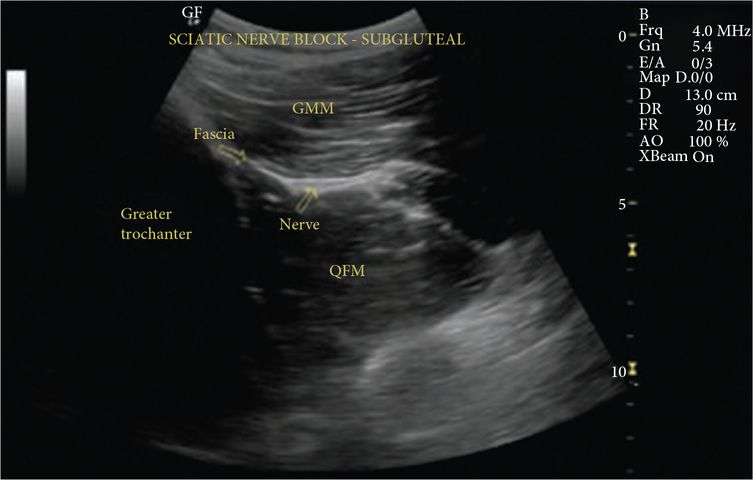
Ultrasound. Using a curvilinear, low-frequency (2–5 MHz) probe, identify the bony landmarks of the GT and IT. The nerve lies between the GT and IT, deep to the gluteus maximus and appears hyperechoic (Figure 28.3).
Clinical pearls. Due to the extensive soft tissue in this region and the thickness of the posterior thigh, the prone or lateral position may be utilized for US visualization.
Advantages/disadvantages. The subgluteal approach is advantageous because of the superficial location of the sciatic nerve compared with a more proximal approach [6]. The Raj approach is ideal for patient positioning as it renders the patient supine and stretches the nerve to allow for minimal potential vascular injury [1]. The sciatic nerve is surrounded by soft tissue in the subgluteal region and can often be difficult to locate with US. It may be mistaken for tendon insertions of the semimembranosus, semitendinosus, or quadratus femoris muscles [7].
Anterior:
Positioning. This approach can be performed with the patient in the supine position and the patella midline or laterally rotated. Chelly and DeLaunay described drawing a line between the inferior border of the anterior superior iliac spine (ASIS) and the superior border of the pubic symphysis (inguinal line) [8]. Barbero et al. modified this technique by drawing a caudad perpendicular line from the midpoint of the inguinal line to the puncture site [9]. The puncture site was calculated using a mathematical formula of (height in cm – 100)/10 and demonstrated a 92% success rate in adequately finding and anesthetizing both the sciatic and posterior cutaneous nerves [8].
Nerve stimulator. Draw the inguinal line and a perpendicular line as described above. Proper needle placement is confirmed with a sciatic twitch, mainly foot dorsiflexion, plantar flexion, eversion, or inversion.
Ultrasound. With the patient’s leg in mild external rotation, place a curvilinear, low-frequency (2–5 MHz) probe at the level of the lesser trochanter. The femur, femoral nerve, artery, and vein will be visualized laterally. The three muscle layers of the adductor longus, brevus, and magnus are identified medial to the vessels. The sciatic nerve lies below the adductor magnus, medial to the femur (Figure 28.4). Needle insertion should avoid the femoral vessel and nerve and femur.
Clinical pearls:
If no twitch is obtained, redirect the needle medially or laterally without contacting bone. The lower extremity can be rotated internally and externally if a twitch is still not obtained; however, avoid redirecting proximally to avoid entering the hip joint capsule [10].
A hamstring twitch indicates the needle is too proximal or direct muscle stimulation. Consider another approach if unable to obtain a distal twitch.
Advantages/disadvantages. The anterior approach can be performed with minimal patient movement, a benefit in trauma patients or patients who require analgesia after surgery. However, performance of the block is associated with more pain compared with posterior approaches and may require more sedation during placement. The posterior cutaneous nerve of the thigh may be missed with this approach [10].
Popliteal:
Anatomy. The popliteal block can be performed in the supine, prone, or lateral position.
Nerve stimulator. The biceps femoris muscle and the semimembranosus/semitendinosus muscles are identified, often facilitated by the patient elevating the foot. This creates a triangle. The needle is inserted at the apex of the triangle; usually 9 cm above the popliteal crease and often 1 cm lateral to the apex. Proper placement is confirmed with a tibial twitch (foot plantar flexion and/or inversion).
Ultrasound. A linear high-frequency (6–15 MHz) probe is placed in the transverse position in the popliteal crease. The popliteal artery is located and the tibial nerve is identified superficially. The tibial nerve is traced cephalad with the probe and the common peroneal nerve merges from the lateral side. Local anesthetic can be inserted before or after the sciatic nerve divides (Figure 28.5).
Clinical pearls:
A semitendinosus muscle twitch indicates medial needle placement (redirect laterally).
A biceps femoris muscle twitch indicates lateral needle placement (redirect medially).
If bone is contacted, the needle is likely too deep and should be slowly withdrawn.
Advantages/disadvantages. The popliteal block can be performed in multiple positions allowing for ease of performance in most patient populations. The nerve is superficial and easier to visualize under US. However, the posterior cutaneous nerve of the thigh is not blocked at this location.