PHARMACODYNAMICS
• Ionization best correlates with onset of action. LAs exist in free equilibrium in both charged (ionized) and neutral (non-ionized) forms:
• The ionized form binds to the receptor and exerts the drug’s action, but it is very hydrophilic and cannot penetrate the nerve membrane to exert its effect
• The non-ionized, lipid-soluble form allows the drug to penetrate nerve membrane
• Lipid solubility correlates with potency: Higher solubility = greater potency
• Protein binding best correlates with duration of action
• The relative proportion of ionized and non-ionized LA molecules is a function of the drug’s pKa and the tissue pH
• pKa = pH at which the concentrations of ionized and non-ionized forms are equal
• Clinical implications include slower onset in acidic (infected) tissue
Speed of LA onset affected by:
• pKa: Lower pKa of the anesthetic = greater the fraction of non-ionized molecules at a given pH → easier membrane penetration → faster onset
• Bicarbonate (HCO3) addition: Higher pH → more non-ionized → quicker onset time
• Lipid solubility: Higher solubility generally = slower onset, may be due to sequestration in lipid membranes
• Higher concentration and total dose of local = faster onset due to diffusion gradient (↑ solution concentration explains ↑ onset of procaine and 2-chloroprocaine despite ↑ pKa)
• Site of injection and distance of diffusion to target nerve (presence of neural sheath delays onset)
Duration of LA action affected by:
• Protein binding: ↑ protein binding → longer duration
• Site of local injection: More vascular sites have shorter duration (more systemic uptake)
• Degree of vasodilation (all locals except cocaine are vasodilators)
• Lipid solubility: ↑ lipid solubility = ↑ duration
• Pseudocholinesterase deficiency : ↑ duration of ester anesthetics
• Liver disease: ↑ duration of amide anesthetics
SPECIFIC CONSIDERATIONS
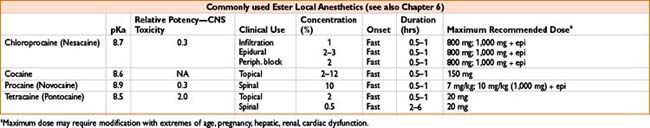
Chloroprocaine
• Most rapid hydrolysis among ester class
• Increasing popularity for short-acting spinal; historical concern about neurotoxicity possibly related to bisulfite preservative
• Useful in obstetrics due to rapid onset, ↓ risk of systemic toxicity/fetal exposure (rapid hydrolysis in bloodstream)
• Useful in pts with significant liver disease, seizure hx
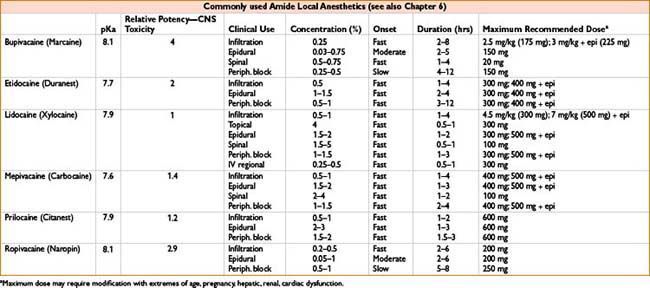
Lidocaine
• Versatile—used for topical, regional, intravenous, peripheral nerve block, and spinal/epidural anesthesia.
• Transient neurologic symptoms (TNS) after spinal anesthesia (also reported with other LAs)
• Pain/sensory ∆ in lower back, buttocks, thighs—no motor or bowel/bladder dysfunction
• Increased risk with lidocaine, lithotomy, ambulatory anesthetic; pregnancy may be protective
• Symptoms occur within 2–24 hrs → complete resolution within 10 d (most in 2 d)
• Tx with NSAIDs and opioids as needed
Bupivacaine
• Useful due to long duration in peripheral and epidural blocks, common in spinals
• High-quality sensory anesthesia relative to motor blockade
• Severe, refractory cardiovascular collapse with toxic intravascular doses
Ropivacaine
• Greatest margin of safety among long-acting locals
• More vasoconstriction, less lipid solubility than bupivacaine → reduced systemic toxicity
Tetracaine
• Useful in spinals due to rapid onset, long duration (4–6 hrs with epi)
• Longer duration but possibly less adequate sensory blockade versus bupivacaine
Cocaine
• Vasoconstrictor property unique among LAs
• CNS stimulant through ↓ reuptake of norepi, dopamine, serotonin
• Used in 4% solution as topical anesthetic (sinus surgery, awake nasal fiberoptic) or 11.8% with tetracaine, epi (TAC) for ED wound repair
• Side effects: HTN, tachycardia, arrhythmias, coronary ischemia, stroke, cerebral & pulmonary edema, seizures
Emla cream—Eutectic Mixture of Local Anesthetics (Lidocaine 2.5%, Prilocaine 2.5%)
• Topical anesthesia for minor procedures (pediatric IV placement)
• Apply to intact skin using smallest amount necessary, cover with occlusive dressing
• Onset ∼45–60 min, duration ∼2 hrs
• Adult dose: 2.5–10 g
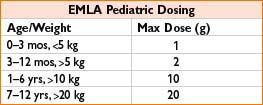
• Avoid in G6PD deficiency and amide allergy
• Toxicity including methemoglobinemia possible
ADDITIVES TO ENHANCE LOCAL ANESTHETICS
• Vasoconstrictors (epinephrine, occasionally phenylephrine) → ↓vascular uptake of drug, ↓ systemic absorption/toxicity, ↑ duration and ↑ intensity of the block; little effect on onset time
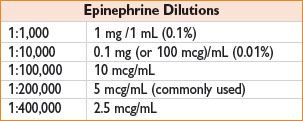
• Add to LA at time of use due to epi instability at higher pH
• Variable response between LA and the location of injection as to whether vasoconstrictors ↑ duration of action:
• Infiltration, peripheral blockade: ↑ duration of shorter (lidocaine) > longer-acting (bupivacaine) LA
• Epidural blockade: Addition of epi to procaine, lidocaine, and bupivacaine →↑ duration of block
• Spinal blockade: Addition of epi (0.2–0.3 mg) to lidocaine, bupivacaine, tetracaine → sig. ↑ duration of block
• Epi may also ↑ quality of epidural/spinal due to α2 adrenergic activation
• Bicarbonate–alkalinization of LA solution →↑ percentage of non-ionized form of the drug → ↑ membrane penetration, ↓ onset time; reduces pain during subcutaneous infiltration
• Opiates: ↑ duration of neuraxial block, ↑ quality of surgical anesthesia and postoperative analgesia
• Clonidine, dexmedetomidine: Useful in peripheral and neuraxial blocks, multiple sites of action; ↑ anesthesia and ↑ duration of block
SYSTEMIC ABSORPTION AND TOXICITY
Systemic toxicity results from excessive plasma concentrations (due to absorption of LAs from tissue or inadvertent intravascular injection). Factors relating to rate of absorption:
• Dose of LA: A 1% solution of any drug contains 1,000 mg of drug per 100 mL of solution, or 10 mg/mL (note multiple doses of different LAs are additive)
• Rate of injection/infusion: Use incremental injection technique with intermittent aspiration
• Local vasodilation (epi vasoconstricts and reduces systemic absorption, some LAs are stronger vasodilators)
• Lipid solubility (potency) of LA, metabolism (plasma vs. liver), renal/hepatic disease, CHF
• Site of injection (based on vascularity of the tissue), with the greatest degree of absorption as follows:
Intravascular > tracheal > intercostal > caudal > epidural > brachial plexus > subcutaneous
Toxicity mainly affects CV system and CNS. CNS is usually affected first. Progressive signs of local anesthetic toxicity:
Light-headedness → circumoral numbness → facial tingling → tinnitus → slurred speech → seizures → unconsciousness → respiratory arrest → cardiovascular depression → circulatory arrest
• “Test dose” of local with epi can indicate likely intravascular injection if associated with a significant and rapid ↑ HR, ↑ BP, or T-wave ∆; use caution as general anesthesia, active labor, β-blocker use can confound results
• CNS toxicity: ↑ with hypercarbia & acidosis (↓ seizure threshold, ↓ bound fraction of drug)
• CV toxicity:
• May have transient ↑ in HR, BP due to CNS stimulation
• Dose-dependent myocardial depression, hypotension, dysrhythmias (especially with bupivacaine)
• ECG ∆s: ↑ PR, ↑ QRS, ↑ QT intervals
LA Toxicity Treatment
• Stop injecting LA; get help; maintain airway (intubate if necessary); give 100% oxygen and consider hyperventilation in the presence of metabolic acidosis; treat seizures (benzodiazepines, propofol in small doses)
• If cardiac arrest with LA toxicity: CPR and treatment of arrhythmias with standard protocols. Consider cardiopulmonary bypass or treatment with 20% lipid emulsion (no role for propofol)
• Lipid emulsion protocol: 20% intralipid 1.5 mL/kg bolus over 1 min (∼100 mL in 70 kg pt); start infusion at 0.25 mL/kg/min (17.5 mL/min for 70 kg pt); if circulation not restored can repeat initial bolus × 1–2 and increase infusion to 0.5 mL/kg/min (www.lipidrescure.org)
• Continue CPR throughout lipid infusion. Recovery may be delayed (>1 hr)
Methemoglobinemia (Normal Hemoglobin Oxidized to Methemoglobin)
• Causes: LAs (benzocaine, prilocaine), antibiotics (dapsone, trimethoprim), nitrates
• Symptoms and signs: SOB, cyanosis (traditional pulse ox unreliable), MS ∆s, loss of consciousness; if >50% met-Hb → dysrhythmias, seizures, coma, and death
• Diagnosis: Blood is “chocolate-brown” color, ABG analysis will typically reveal normal pO2 +/- metabolic acidosis, measure met-Hb level with co-oximetry
• Treatment: Supplemental O2, 1% methylene blue 1–2 mg/kg IV (restores iron in Hb to its normal reduced O2-carrying state), hyperbaric O2

Full access? Get Clinical Tree








