Anesthetic Risk, Quality Improvement, and Liability
In anesthesia, as in other areas of life, everything does not always go as planned. Undesirable outcomes may occur regardless of the quality of care provided. An anesthesia risk management program can work in conjunction with a program for quality improvement to minimize the liability risks of practice while ensuring the highest quality of care for patients (Posner KL, Adeogba S, Domino KB. Anesthetic risk, quality improvement, and liability. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013: 90–104).
I. Anesthesia Risk
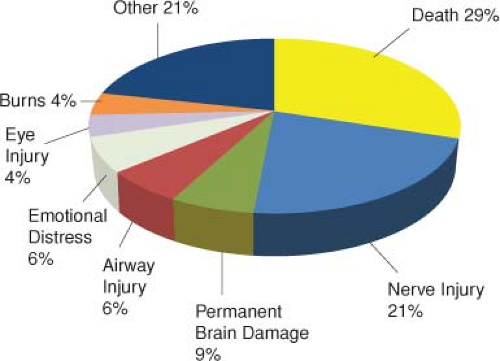
Mortality and Major Morbidity Related to Anesthesia. Estimates of anesthesia-related morbidity and mortality are difficult to quantify because of different methodologies, definitions of complications, lengths of follow-up, and evaluation of contribution of anesthesia care to patient outcomes (Table 4-1). It is generally accepted that anesthesia safety has improved over the past 50 years. However, several recent complications related to anesthesia have received increasing attention (Table 4-2 and Fig. 4-1).
II. Risk Management
Conceptual Introduction. Risk management and quality improvement programs work hand in hand in minimizing liability exposure while maximizing quality of patient care. Quality improvement (sometimes called patient safety) departments are responsible for providing the resources to provide safe, patient-centered, timely, efficient, effective, and equitable patient care.
Risk Management in Anesthesia. Aspects of risk management most directly relevant to the liability exposure of anesthesiologists include prevention of patient injury, adherence to standards of care, documentation, and patient relations.
Table 4-1 Recent Estimates of Anesthesia-Related Death
Time Period
Country
Data Sources and Methods
Anesthesia-Related Death
1989–1999
USA
Cardiac arrests within 24 hr of surgery (72,959 anesthetics) in a teaching hospital
0.55/10,000 anesthetics
1992–1994
USA
Suburban teaching hospital (37,924 anesthetics and 115 deaths)
0.79/10,000 anesthetics
1995–1997
USA
Urban teaching hospital (146,548 anesthetics and 232 deaths)
0.75/10,000 anesthetics
1995–1997
Holland
All deaths within 24 hr or patients who remained comatose 24 hr after surgery (869,483 anesthetics and 811 deaths)
1.4/10,000 anesthetics
1990–1995
Western Australia
Deaths within 48 hr or deaths in which anesthesia was considered a contributing factor
1/40,000 anesthetics
1994–1996
Australia
Deaths reported to the committee (8,500,000 anesthetics)
0.16/10,000 anesthetics
1992–2002
Japan
Deaths caused by life-threatening events in the OR (3,855,384 anesthetics) in training hospitals
0.1/10,000 anesthetics
1994–1998
Japan
Questionnaires to training hospitals (2,363,038 anesthetics)
0.21/10,000 anesthetics
1989–1995
France
ASA 1–4 patients undergoing anesthesia (101,769 anesthetics and 24 cardiac arrests within 12 hr after anesthesia)
0.6/10,000 anesthetics
1994–1997
USA
Pediatric patients from 63 hospitals (1,089,200 anesthetics)
0.36/10,000 anesthetics
1999–2005
USA
Deaths with anesthesia-related complication codes from death certificate data
8.2/million hospital surgical discharges
2003–2005
Australia
Deaths reported to Anesthesia Mortality Committees
Anesthesia-related deaths 0.19/10,000
ASA, American Society of Anesthesiologists; OR, operating room.
Table 4-2 Complications Related to Anesthesia
Postoperative nerve injury
Ulnar nerve injury
Lower extremity neuropathy after surgery in the lithotomy position after neuraxial anesthesia
Awareness during general anesthesia (estimated to occur in 1–2 per 1,000 patients in a tertiary care setting)
Vision loss and eye injuries
Corneal abrasion
Ischemic optic neuropathy
Central retinal artery occlusion
Dental injury (3.6/10,000 for general anesthesia with tracheal intubation)
The key factors in the prevention of patient injury are vigilance, up-to-date knowledge, and adequate monitoring. The Web site of the American Society of Anesthesiologists (ASA) may be reviewed for any changes in ASA Standards of Practice as well as a review of ASA guidelines.
Table 4-3 World Health Organization Surical Safety Checklist Elements
Before Induction 
Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access