1. Because pediatric anesthetics outside the operating room are performed with increasing frequency, it is important for any institution to have a system in place to meet the service needs and enable effective allocation of personnel.
2. The provision of these services is in demand because of the expertise that anesthesiologists can bring to increasing comfort, efficiency, and quality care in these nontraditional locations.
3. Clinicians must be familiar with the anesthetic demands of the procedures and of the limitations and nature of the practice environment. Both of these are likely to be considerably different from the familiar operating room setting, but the same standards for pre-, intra-, and postanesthetic care must be maintained.
4. Recovery from anesthesia may be integrated into the institution’s already existing recovery system, but considerations of scale and of transport, especially if long distances are involved, may argue in favor of a satellite facility.
Perhaps one of the greatest areas of growth in pediatric anesthesia practice has been in “off-site” anesthesia. The expansion of services to remote locations in the hospital and clinic has been driven by several factors:
• Parental demand for more humane and compassionate care for their children during nonoperative procedures.
• The recognition that “sedation” services provided by nonanesthesiologists may not optimally meet the needs of many patients undergoing more invasive procedures, and that the unique capabilities that anesthesiologists have regarding advanced techniques and drugs enable greater flexibility when caring for complex patients.
• The greater efficiency and safety that can be afforded by anesthesiologists and postanesthesia recovery systems (1).
The provision of anesthesia services in these environments, however, is not the same as in the operating room (OR) and requires careful attention to details that the anesthesiologist may otherwise take for granted in more familiar surroundings. It is imperative that the same standard of care and the same safety systems be in place no matter where the anesthetic is administered.
I. Patient selection
A. Imaging studies, diagnostic and interventional procedures, and radiation treatments are all dependent on equipment that cannot, in many cases, be moved into the OR. Therefore, any infant or child might need an anesthetic outside the surgical suite. The skills and techniques of the anesthesiologist must also be mobile to accomplish these cases. Even critically ill patients can be anesthetized for these procedures, but may require greater resources for safe transport to and from the intensive care unit.
B. Children receiving radiation therapy, intrathecal chemotherapy, esophageal dilations, and the like have their procedures and anesthetics repeated on a regular basis. It is extremely helpful if they have as stress-free an experience as possible, particularly for the first few visits. Distress and anxiety during anesthetic induction are linked to negative behavioral changes, and the problems of maladaptive behavior can be greatly magnified in these patients if the anesthetic experience is repeatedly difficult (2). Family-centered pediatric perioperative care can have a particularly dramatic beneficial impact here, and integration of these principles should be imbedded into the system of care (3,4). An implanted vascular access device is invaluable for these patients; for those who cannot have one, premedication or even the use of hypnosis should be seriously considered.
CLINICAL PEARL Children with implanted ports (as opposed to tunneled catheters) who are anesthetized daily can have their ports accessed on Monday and heparin locked for the week, and then de-accessed on Friday.
II. Preoperative evaluation and assessment. Children receiving anesthesia “off-site” are in many ways managed no differently than in the OR. They still require a preprocedural evaluation that includes a history and physical examination with particular attention to the airway, cardiovascular, and respiratory systems, as well as those systems that affect drug uptake, distribution, and metabolism. Because many of these patients will be discharged on the day of the procedure, suitability for rapid discharge from the postanesthesia care unit (PACU) must be assessed.
A. To avoid unanticipated cancellations, there should be a mechanism by which the child’s parents are contacted a day or more before they arrive at the hospital and are assessed preliminarily either by telephone or in person. This also provides an opportunity to reinforce preanesthetic teaching about NPO status, administration of regular medications, and to answer questions that the parent might have that could otherwise present unforeseen problems on the day of the procedure.
B. For imaging studies, where the ordering physician is often not present, it is very important to have a letter of referral or consultation note in the chart so that the anesthesiologist knows exactly why the procedure is being performed and the details of the patient’s history. Ideally this can be required in order to actually book the study.
III. Recovery from anesthesia. The major decision for recovery facilities is whether the patient should be transported to the regular PACU or if an off-site recovery facility can be developed.
A. The latter choice has numerous advantages, including efficiency and the elimination of the transport of an anesthetized patient over what might be significant distances through public hallways and elevators. Transport always carries some risk, and requires monitoring and trained personnel with clearly planned routines and contingency and emergency procedures that should be practiced at regular intervals.
B. Two people, a nurse and an anesthesiologist, must accompany the unconscious or emerging patient during transport. If transport involves the use of an elevator, one of the transport personnel should have a key to control the elevator (“fireman’s key”) and only the personnel involved in the transport should ride in the elevator.
C. For cases that begin in an off-site location and then conclude in the OR (e.g., magnetic resonance imaging [MRI] for fiducial placement before craniotomy), it is usually best to secure the airway at the time of induction and transport the patient anesthetized and monitored. For the opposite scenario, when imaging studies or other investigations follow and operation, realistic scheduling, and ongoing communication in the event of delays are needed.
D. Off-site recovery for ambulatory cases—a satellite PACU—can consume both physical and human resources and is not without serious start-up costs, but is probably the best choice if the institution has adequate case volume to support this option. Efficiency can be improved and cost savings realized if multiple sites are physically located adjacent to the off-site PACU. It is essential that the identical standards of staffing, training, and care apply to this recovery facility as they apply in the OR PACU.
IV. Types of procedures. Off-site anesthetics are generally administered to two broad groups of children: those who require immobilization for nonstimulating procedures (most commonly imaging or related diagnostic procedures) and those who are undergoing a painful invasive procedure in a location distant from the OR. The former are more commonly children who are younger and uncooperative due to developmental issues, but older children with developmental delays or those with neuropsychiatric disorders may require similar treatment. Nearly all children younger than 3 years will require some sort of sedation or anesthesia for imaging procedures that require complete immobilization and last more than several minutes. Noninvasive procedures are most commonly imaging studies, radiation treatments, or neurologic testing such as brainstem auditory evoked responses (BAERs).
Interventional procedures most often require general anesthesia even in older children. These may be more complex and involve more frequent use of a secured airway, and may even be nearly as stimulating as some operative procedures. These may also require postoperative conditions that are more demanding than for noninvasive procedures, such as several hours of limited motion and supine positioning after angiography or cardiac catheterization. Such considerations must be factored in to not only the anesthetic technique but also into postanesthetic recovery facilities and conditions, and these more complex patients may best recover in the OR PACU.
V. Clinical settings and environments. These cases may commonly be performed in locations where equipment is “hard-wired” and cannot be moved to the OR (MRI, computed tomography [CT], radiation therapy, cardiac catheterization, etc.) or for other reasons may be in distant clinics (oncology, bronchoscopy, endoscopy). In most hospitals, decentralization of off-site locations presents numerous challenges to the anesthesiologist, and requires the implementation of new systems for technologist support, preoperative evaluation, postoperative recovery, and intraoperative nursing support by personnel familiar and experienced with caring for anesthetized children. The careful and thoughtful implementation of such systems is critical to the safe conduct of off-site anesthetics, as it is the integration of these systems that determines both risk and prompt and appropriate responses to the adverse events which inevitably will occur.
CLINICAL PEARL A successful and efficient off-site anesthesia service is best planned and instituted by a multidisciplinary working group consisting of anesthesiologists, proceduralists, preoperative and PACU nurses, technologists, and even hospital physical plant personnel, to jointly plan the physical layout, patient flow scheme, and necessary resource allocation. A systematic approach like this is much less likely to fail than spontaneous and unplanned efforts to fill the gaps that inevitably arise.
A. The radiology suite. Any imaging procedure that requires immobility for more than a brief period of time is likely to benefit from the use of general anesthesia. Although it is common for various sedative drugs to be used in place of general anesthesia, numerous studies have shown a higher success rate, fewer complications, and better efficiency when an anesthesiologist-run program is employed. The major impediment to the implementation of such programs is usually the lack of adequate anesthesiology staff.
1. Magnetic resonance imaging. Because of the frequency of its use and the length of scan times, MRI may be the most common location for anesthetics in radiology. The magnetic field presents unique technologic problems, but commercially available equipment has largely ameliorated these issues.
a. It is essential that equipment brought into the magnet room be able to function safely in a high-magnetic-field environment and not emit radiofrequency noise that can interfere with the scan. Most magnet rooms will have a 50-gauss line marked on the floor beyond which MRI-compatible equipment may be used. Several manufacturers produce MRI-compatible anesthesia machines, monitors, and infusion pumps. Laryngoscopes that are made of plastic or nonferromagnetic metals are available, but one must also use lithium batteries rather than the more common alkaline types that can be deflected by the magnetic field. Plastic stethoscopes and scissors must also be used. Safety in the magnet room, especially as 3T magnets become more common, is a critical priority, as ferromagnetic objects can become dangerous projectiles if brought too close to the magnetic field.
b. Numerous anesthetic techniques for MRI have been described. Recently, dexmedetomidine has received a lot of attention for this indication, in large part because of the lower risk of airway problems. Its disadvantage is slow induction and much longer emergence times, which can adversely affect case throughput in a busy radiology department. It is of particular advantage when scanning children with upper airway obstruction and sleep-disordered breathing (5). This author believes that the best technique for anesthetic maintenance in the MRI for most children is a continuous infusion of propofol. Because the anesthetic goal for MRI, like most imaging techniques, is immobilization without any need for analgesia, propofol is ideal. In most circumstances, careful titration of the infusion rate produces an immobile patient with well-maintained spontaneous ventilation and also permits rapid emergence with minimal risk of nausea. The very rapid recovery time can allow discharge much sooner than with other techniques (6).
c. In the author’s experience, most pediatric patients require an infusion rate of approximately 200 µg/kg/minute to assure immobility, assuming an uninstrumented airway, although 100 µg/kg/minute after a 2-mg per kg loading dose has been reported to prevent movement (7). General anesthesia has been shown to be superior to sedation with other agents administered by nonanesthesiologists (8). For children who do not have an intravenous (IV), we most often perform an inhalation induction with sevoflurane, place an IV as soon as consciousness is lost, and then switch to propofol without a loading dose.
d. Most syringe pumps, if kept outside of the 50-gauss line, will function accurately in a 1.5T or lower environment, but this must be checked by the hospital’s biomedical instrumentation service and unless mounted to a fixed object carries a risk of being drawn into the magnet. The pump should be run on batteries rather than on line current. Remote-controlled pumps are available for the MRI environment, but perhaps the best solution is to have a radiofrequency shielded port in the doorframe, through which a long extension tubing set is threaded (Fig. 39.1). This enables control and refilling of the pump as necessary without interrupting the scan to enter the magnet room.
e. Because the patient is within the bore of the magnet during the scan and difficult to visualize, respiratory monitoring is particularly important. End-tidal CO2 monitoring is essential for the safe conduct of general anesthesia or sedation in the MRI because auscultation is nearly impossible and chest wall motion is difficult to assess accurately. In the unintubated patient, the use of nasal cannulae attached to a sidestream capnograph can easily confirm spontaneous respiration even when direct visualization of the patient is obscured (9).
f. If the patient is able to maintain a patent airway and has normal ventilatory control, it is rarely necessary to intubate or place a laryngeal mask airway (LMA). Supplemental oxygen can be administered through nasal cannula, but meticulous attention to head position is necessary. Cardiac MRI, however, involves multiple sequences requiring breath-holding, and therefore these patients will need to be intubated (10). MRI angiography may similarly require breath-hold sequences (11). Unlike most MRIs, where the anesthesiologist can, with proper remote monitoring, remain outside the magnet room during the scan, during these scans the anesthesiologist needs to be in the room with the patient. Ear protection should be worn because of the noise level, and there must be an effective means of communication with the technologist running the scanner at all times.
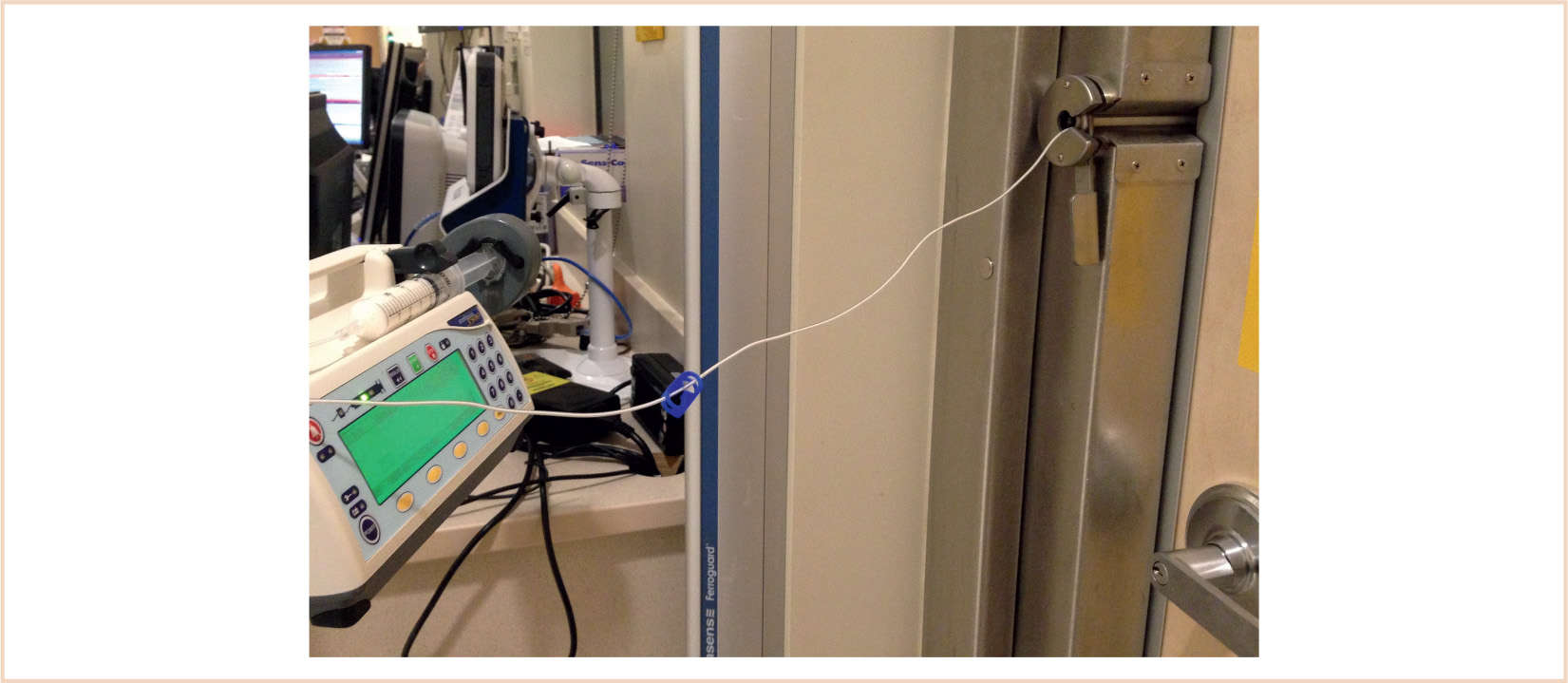
FIGURE 39.1 Propofol infusion fed through a radio frequency shielded port in the door frame of the MRI.

Full access? Get Clinical Tree








