CHAPTER 27 Anesthesia for Ophthalmic Surgery
Anesthesia for ophthalmologic procedures in children requires an understanding of several physiologic and pharmacologic concepts that are unique to this population. The majority of ophthalmic procedures are brief and noninvasive, but the spectrum extends to more invasive procedures in patients with significant comorbid disease. Caring for otherwise healthy children undergoing nasolacrimal duct probing or strabismus surgery may be relatively straightforward, but the pediatric anesthesiologist is also required to care for vulnerable infants born prematurely or with congenital disorders and associated pathology of the eye. In 2005 there were 2.2 million procedures performed on patients younger than 15 years of age; 12,000 of these were operations on the eye (Defrances and Hall, 2007). Most of these procedures are performed in the ambulatory setting. In an analysis of ophthalmic procedures performed in surgery centers, the reasons for cancellation of surgery within 24 hours were explored. The pediatric group (0 to 9 years of age) had the highest rate of cancellation when compared with those in other age groups. The majority of cancellations, however, were because of unpreventable causes such as patient illness (Henderson et al., 2005). The information contained in this chapter will give anesthesiologists the information needed to plan for and safely perform anesthesia for ophthalmic procedures.
Anesthesiologists with a particular interest in ophthalmologic anesthesia can find valuable resources through the Ophthalmic Anesthesia Society (http://www.eyeanesthesia.org) and the British Ophthalmic Anaesthesia Society (http://www.boas.org). A glossary of terms is given in Box 27-1.
Box 27-1 Glossary of Ophthalmologic Terms
From Dorland’s illustrated medical dictionary, Philadelphia, 2000, Saunders.
Anatomy and Physiology
Knowledge of the anatomy and physiology of the eye is paramount to understanding the array of ophthalmic procedures performed, the influence that anesthesia may have on normal and abnormal ocular physiology, and the systemic effects that surgical manipulation of the eye may have on the patient (McGoldrick, 1992a).
Anatomy Overview
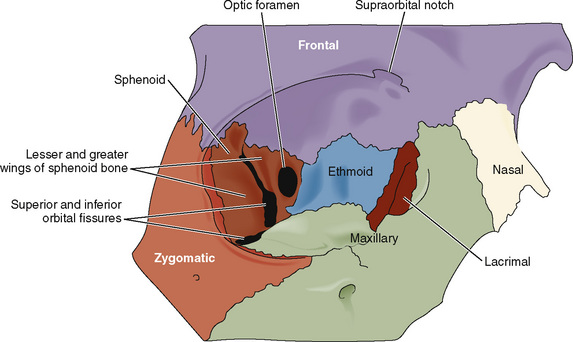
The orbit is formed by a complex arrangement of seven cranial bones: frontal, zygomatic, sphenoid, maxilla, palatine, lacrimal, and ethmoid (Fig. 27-1). The optic foramen transmits the optic nerve, the ophthalmic artery and vein, and the sympathetic contributions from the carotid plexus. The superior orbital fissure transmits branches from four other cranial nerves (oculomotor, trigeminal, trochlear, and abducens) and the superior and inferior ophthalmic veins. The infraorbital fissure (representing the weakest aspect of the orbit) transmits the infraorbital and zygomatic nerves. The infraorbital foramen (located below the orbital rim) transmits the infraorbital nerve, artery, and vein.
The aqueous humor occupies the anterior and posterior chambers of the eye and is responsible for providing nutrients to the avascular lens and the endothelial aspect of the cornea (Fig. 27-2). The volume of aqueous humor (0.3 mL in the adult) is primarily responsible for intraocular pressure (IOP) regulation. The vitreous humor, created embryologically between 1 and 4 months’ gestation, is a hydrophilic gel that accounts for 80% of the volume of the globe. The vitrous humor is 99% water, although in the presence of hyaluronic acid (a mucopolysaccharide), its viscosity is twice that of water. The volume of the vitreous humor is more constant than that of the aqueous humor, although it may be slightly influenced by hydration status and osmotically active medications.
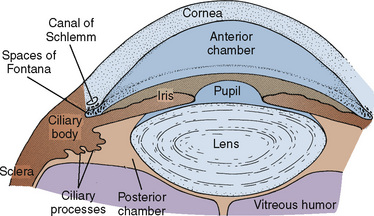
FIGURE 27-2 Anatomy of the anterior eye.
(From McGoldrick KE: Anesthesia for ophthalmic surgery. In Motoyama ES, Davis PJ, editors: Smith’s anesthesia for infants and children, ed 6, Philadelphia, 1996, Mosby.)
The optic nerve (cranial nerve II) is the nerve of vision and may be thought of as a diverticulum of the forebrain. The oculomotor nerve (cranial nerve III) provides motor innervation to four of the six extraocular muscles and the levator palpebrae superioris, as well as parasympathetic innervation to the pupillary sphincter (miosis) and ciliary muscles (accommodation). The two other extraocular muscles are innervated by the trochlear and abducens nerves. The ophthalmic division of the trigeminal nerve (cranial nerve V) transmits all of the nonvisual sensory innervation from the eye and orbit and provides sympathetic innervation to the pupillary dilators (mydriasis). The temporal and zygomatic branches of the facial nerve (cranial nerve VII) innervate the orbicularis oculi (Ellis and Feldman, 1997).
Blood is supplied to the eye and orbit through branches of the internal and external carotid arteries. The first branch of the intracranial carotid artery, the ophthalmic artery, divides into the central retinal artery, as well as the long and short posterior ciliary arteries, to nourish the retina. The long and short posterior ciliary arteries converge to supply the choriocapillaris, the capillary layer within the choroid that supplies 60% to 80% of the oxygen to the retina. The anterior portion of the optic nerve is perfused by the posterior ciliary arteries. It is this network of arteries that is subject to significant individual variation, predisposing some patients to anterior ischemic optic neuropathy after periods of hypotension. The posterior optic nerve is perfused by pial vessels branching from the ophthalmic artery. Superior and inferior ophthalmic veins drain the orbit, and the central retinal vein provides ocular drainage. All venous drainage is subsequently transmitted to the cavernous sinus (Williams, 2002).
Physiology Overview
Normal IOP varies between 10 and 20 mm Hg and may differ by as much as 5 mm Hg between the two eyes. Normal pressures are somewhat lower in the newborn (average, 9.5 mm Hg) but approximate adult pressures by 5 years of age (Pensiero et al., 1992). A pressure above 25 mm Hg at any age is considered abnormal (Johnson and Forrest, 1994). Transient changes in IOP are well tolerated in the intact eye, although chronic elevations may be detrimental to normal retinal perfusion and vision.
With mydriasis, Fontana’s spaces narrow, resistance to outflow is increased, and IOP rises. Mydriasis is a threat in both closed-angle and open-angle glaucoma.* Hence, a miotic agent such as pilocarpine hydrochloride is often efficacious when applied conjunctivally before surgery in patients with glaucoma.
The arterial circulation of the eye is autoregulated. Only marked deviations in systemic arterial pressures affect IOP. Elevated venous pressures, on the other hand, can dramatically increase IOP, primarily by augmenting the choroidal blood volume and tension of the orbit. Coughing, vomiting, and Valsalva maneuvers may increase IOP to 40 mm Hg or more. Respiratory acidosis increases IOP, whereas metabolic acidosis has the opposite effect. Conversely, respiratory alkalosis decreases IOP, whereas metabolic alkalosis increases IOP (Calobrisi and Lebowitz, 1990). Hypoxia is capable of increasing IOP by dilating intraocular vessels, whereas hyperoxia appears to decrease IOP (Johnson and Forrest, 1994).
The OCR, through its vagal efferent pathway, may manifest as sinus bradycardia, ectopy, and sinus arrest. Death secondary to the OCR in otherwise healthy children has been described (Lang and Van der Wal, 1994; Smith, 1994). A more thorough description of this reflex, prophylaxis, and therapy are provided later in the discussion on intraoperative complications.
The ORR has also been recognized for nearly 100 years but is less often appreciated with the use of controlled ventilation. Through a postulated connection between the trigeminal nerve, the pneumotaxic center of the pons, and the medullary respiratory centers, pressure on the extraocular muscles may result in tachypnea or respiratory arrest (Johnson and Forrest, 1994). This reflex is not inhibited by the use of atropine or glycopyrrolate. A review of the ORR and its potential for causing hypercapnia and hypoxia (potentially aggravating the OCR) has heightened awareness of the reflex and led some investigators to recommend controlled ventilation during strabismus surgery (Blanc et al., 1988).
The OER is admittedly more theoretic than the other two reflexes but would explain the high incidence of nausea and emesis after strabismus surgery. An association between the OCR and the OER has been demonstrated such that patients who exhibit the OCR intraoperatively are 2.6 times more likely to experience postoperative vomiting than those without OCR manifestations (Allen et al., 1998). Anticholinergic therapy does not decrease the incidence of postoperative nausea and vomiting (PONV). Appropriate prophylaxis and treatment of PONV have been studied extensively and are thoroughly reviewed later in this chapter.
General Considerations In Caring for the Ophthalmologic Patient
Associated Congenital and Metabolic Conditions
Ophthalmologic disorders may be inherited as isolated defects in autosomal recessive, autosomal dominant, and X-linked recessive fashion. An additional large number of metabolic defects, congenital syndromes, and chromosomal abnormalities are also associated with ocular pathology. The anesthesiologist caring for the ophthalmologic patient must be aware of these associations. An overview of the commonly encountered syndromes and disorders along with their ocular manifestations and potential anesthetic implications is provided in Table 27-1 (McGoldrick, 1992d; Butera et al., 2000; Baum and O’Flaherty, 2006).
TABLE 27-1 Congenital Syndromes and Chromosomal Abnormalities with Associated Ocular Manifestations
| Disorder or Syndrome | Ocular Manifestations | Anesthetic Implications |
| Acute intermittent porphyria | Cataracts, retinal degeneration, optic atrophy | Various medications, including barbiturates and etomidate, may trigger attacks. |
| Apert’s syndrome | Glaucoma, cataracts, strabismus, hypertelorism, proptosis | Possibly difficult intubation, possible choanal stenosis, cervical spine fusion, CHD (10% incidence) |
| Cri du chat syndrome | Strabismus | Micrognathia and possibly difficult intubation, hypotonia, prone to hypothermia, CHD (33% incidence) |
| Crouzon’s disease | Glaucoma, cataracts, strabismus, hypertelorism, proptosis | Possibly difficult intubation, possible elevated intracranial pressure |
| Cystinosis | Corneal clouding, retinal degeneration | Chronic renal failure, possible diabetes mellitus, esophageal varices, recurrent epistaxis, hyperthermia |
| Down syndrome | Cataracts, strabismus | Trisomy 21, airway obstruction, atlantoaxial instability, CHD (50% incidence), may be more sensitive to atropine |
| Ehlers-Danlos syndrome | Retinal detachment, blue sclera, ectopia lentis, keratoconus | Laryngeal trauma possible with intubation, careful positioning, avoid arterial and central venous lines |
| Goldenhar’s syndrome | Glaucoma, cataracts, strabismus, lacrimal drainage defects | Hemifacial microsomia and possible cervical spine abnormalities, possible difficult mask and intubation, rare CHD, and hydrocephalus |
| Hallerman-Streiff syndrome | Congenital cataracts, coloboma, microphthalmia, glaucoma | Major craniofacial abnormalities with likely difficult intubation, upper airway obstruction, chronic lung disease |
| Homocystinuria | Ectopia lentis, pupillary block glaucoma, retinal detachment, central retinal artery occlusion, strabismus optic atrophy, | Marfanoid habitus with kyphoscoliosis and sternal deformity, prone to thromboembolic complications and hypoglycemia |
| Hunter’s syndrome | Retinal degeneration, optic atrophy | Often difficult intubation, copious secretions, macroglossia, stiff temporomandibular joint, limited neck mobility, possible ischemic or valvular heart disease |
| Hurler’s syndrome | Corneal clouding, retinal degeneration, optic atrophy | Often difficult intubation and difficult mask, possible cervical spine instability, possible ischemic or valvular heart disease |
| Jeune syndrome | Retinal degeneration | Limited thoracic excursion, pulmonary hypoplasia, possible renal and hepatic insufficiency |
| Lowe’s syndrome | Cataracts, glaucoma (hydrophthalmia) | Renal failure, renal tubular acidosis |
| Marfan syndrome | Ectopia lentis, glaucoma, retinal detachment, cataracts, strabismus | Aortic or pulmonary artery dilation, aortic and mitral valve disease, pectus excavatum, risk for pneumothorax |
| Moebius sequence | Strabismus, ptosis, congenital nerve VI and VII palsy | Possibly difficult intubation, micrognathia, copious secretions, possible cervical spine anomalies |
| Myotonia congenita | Cataracts, blepharospasm | Prone to myotonic contractions, sustained contraction with succinylcholine |
| Myotonic dystrophy | Cataracts, ptosis, strabismus | Prone to myotonic contractions, succinylcholine-associated contractions and hyperkalemia, cardiac conduction abnormalities, sensitive to central nervous system depressants |
| Rubella syndrome | Cataracts, microphthalmos, glaucoma, optic atrophy | Neonatal pneumonia, anemia, and thrombocytopenia; CHD, hypopituitarism, diabetes mellitus |
| Sickle cell disease | Retinal detachment, vitreous hemorrhage, retinitis proliferans | Tendency for sickling occurs with high hemoglobin S concentrations, hypoxemia, cold, stasis, dehydration, and infection |
| Smith-Lemli-Opitz syndrome | Congenital cataracts | Possibly difficult intubation, micrognathia, pulmonary hypoplasia, CHD, gastroesophageal reflux, seizure disorders |
| Stickler syndrome | Vitreous degeneration, retinal detachments, cataracts, strabismus | Possibly difficult intubation, micrognathia, mitral valve prolapse, marfanoid habitus, scoliosis, kyphosis |
| Sturge-Weber syndrome | Choroidal hemangioma, glaucoma, ectopia lentis | Angiomas of the airway, CHD and high output failure, seizure disorders, hyperkalemic response to succinylcholine in those with hemiplegia |
| Treacher Collins syndrome | Lid defects, microphthalmia | Often difficult intubation, mandibular hypoplasia, CHD |
| Turner’s syndrome | Ptosis, strabismus, cataracts, corneal scars, blue sclera | Possibly difficult intubation and intravenous access, CHD |
| von Hippel–Lindau syndrome | Retinal hemangioma | Possible increased intracranial pressure, possible pheochromocytoma, cerebellar tumors may also produce episodic hypertension |
| von Recklinghausen’s disease | Ptosis, proptosis, optic glioma and meningioma, optic atrophy, glaucoma, Lisch nodules | Possibly difficult mask ventilation and intubation, possible airway tumors, restrictive lung disease, renovascular hypertension, possible pheochromocytoma, sensitive to neuromuscular blockers |
| Zellweger syndrome | Glaucoma, cataracts, optic atrophy, optic nerve hypoplasia | Micrognathia, possible CHD, renal and adrenal insufficiency |
CHD, Congenital heart disease.
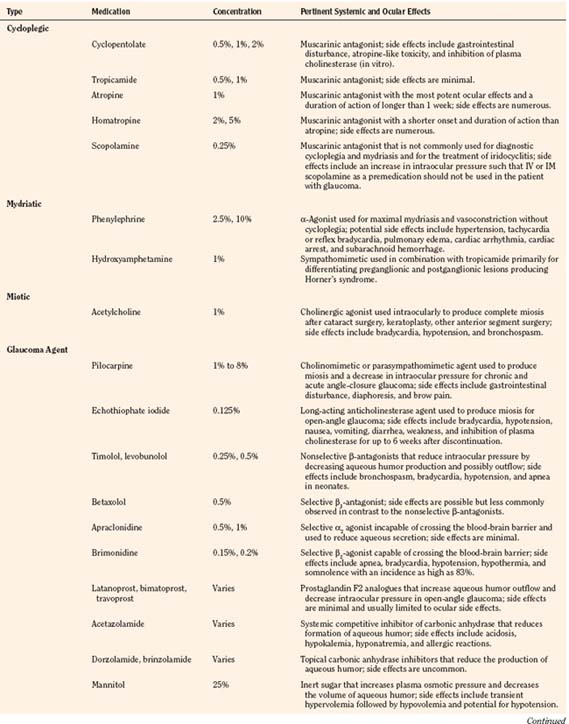
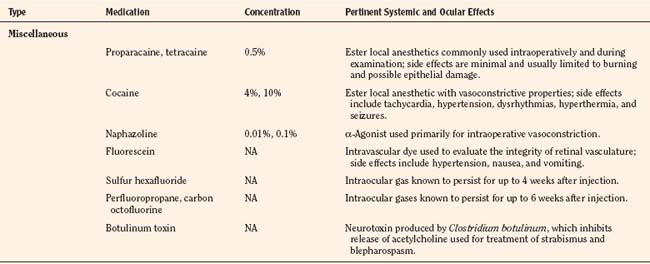
Ophthalmologic Medications and Their Systemic Effects
There are a variety of medications used by pediatric ophthalmologists in the outpatient and perioperative settings that may have important anesthetic ramifications. As with all medications, the ophthalmic agents have both desirable and undesirable effects that may be more pronounced and ominous in the pediatric patient by virtue of greater systemic absorption or higher dosing relative to body weight and pharmacologic compartment. The anesthesiologist must be familiar with every medication used in the perioperative period and pay particular attention to the total dose administered and potential for deleterious effects. An overview of the ophthalmic medications is provided (Table 27-2).
Topical ophthalmologic agents have greater use than systemic agents in the pediatric and adult populations, primarily because most of the side effects that would be consequential to systemic administration are diminished. Nevertheless, the excess from ocular application invariably enters the lacrimal system, reaching the nasopharyngeal mucosa where systemic absorption is greatly enhanced compared with that at the conjunctival sac. Whereas a single drop from a commercial eye dropper may have a volume ranging between 50 and 75 μL, maximal ocular bioavailability is reached by instillation of only 20 μL (McGoldrick, 1992b). It has been recommended that digital pressure over the lacrimal duct for 5 minutes after instillation may reduce systemic absorption by 67% (Zimmerman et al., 1984). Keeping the eye gently closed for 5 minutes may afford similar benefit, yet both techniques are understandably difficult in the conscious and fretful child.
Cycloplegic and Mydriatic Agents
Cyclopentolate, a commonly used cycloplegic agent, has a peak effect within 20 to 45 minutes and residual effects that persist for as long as 36 hours (Cooper et al., 2000). Mild gastrointestinal discomfort and feeding intolerance are the most commonly encountered side effects, although more severe atropine-like toxicity with symptoms ranging from vomiting, ileus, hyperthermia, delirium, and grand mal seizures (Kennerdell and Wucher, 1972; Bauer et al., 1973) has also been reported.
Atropine and homatropine are extremely potent anti-accommodative agents that are rarely used for pediatric patients in the perioperative setting. These agents are more commonly used for intraocular inflammation and amblyopia therapy; they may also be used for prolonged mydriasis after cataract extraction to prevent the formation of synechiae. Common side effects include thirst, tachycardia, and hyperthermia, although more severe symptoms may result after overzealous administration (McGoldrick, 1992b).
Ophthalmic phenylephrine (available in 2.5% and 10% concentrations) is commonly used for mydriasis and vasoconstriction during various procedures. Maximal effects are usually observed within 15 minutes, and residual effects may persist for 4 hours after administration. The generally accepted dosing limit for pediatric patients is one drop of the 2.5% solution in each eye per hour (Borromeo-McGrail et al., 1973). One drop (50 µL) of the 2.5% solution contains approximately 1.25 mg of phenylephrine. The potential for severe hypertension, pulmonary edema, cardiac arrhythmia, cardiac arrest, and subarachnoid hemorrhage with topical phenylephrine is well appreciated by surgeons and anesthesiologists alike. With careful application of the 2.5% solution, systemic effects are typically mild, well tolerated, and generally observed within 1 to 20 minutes after application (Fraunfelder et al., 2002). Although one study demonstrated no significant difference in the mydriatic effects of cyclopentolate vs. phenylephrine (both administered in combination with tropicamide), many ophthalmologists still rely on the medication either primarily or when additional dilation is needed after the administration of other preparations (Rosales et al., 1981).
Glaucoma Pharmacologic Therapy
Pilocarpine is a parasympathomimetic agent that produces miosis and a fall in IOP that is thought to result from an increase in aqueous humor outflow. It is rarely used for temporary treatment before surgery in children but should be discontinued on the evening before surgery for adequate assessment of pressure (Khaw et al., 2000). At recommended dosages, side effects are thought to be rare but may include gastrointestinal disturbances and diaphoresis. More severe cardiovascular effects (e.g., hypotension, bradycardia, and atrioventricular block) are occasionally observed in the geriatric patient (Everitt and Avorn, 1990).
Topical epinephrine and its prodrug, dipivefrin, are sympathomimetic agents historically used in the treatment of glaucoma. Topical epinephrine is occasionally used by ophthalmologists in the intraoperative setting and is known to potentiate dysrhythmias in the myocardium sensitized by the volatile agents. Of all the potent inhalation agents, halothane clearly has the greatest dysrhythmogenic potential, although one study has demonstrated that the pediatric heart may be more resistant to the interactions between halothane and exogenous epinephrine (Karl et al., 1983; Ueda et al., 1983). At equipotent concentrations, isoflurane has three times less dysrhythmogenic potential than halothane (Marshall and Longnecker, 2001). Desflurane and sevoflurane are thought to be similar to isoflurane in this regard (Moore et al., 1993; Navarro et al., 1994).
The β-blocking agents timolol, levobunolol, and betaxolol act by decreasing the production of aqueous humor and are occasionally used postoperatively in children. The agents should not be used in the neonatal and infant populations in light of several reports of apnea with the use of timolol (Olson et al., 1979; Bailey, 1984). In older children and adults, the use of betaxolol, which is selective for the β1-receptors, is associated with fewer complications involving the pulmonary system, although dyspnea and bronchospasm have been reported (Everitt and Avorn, 1990). Lethargy, bradycardia, and heart block are possible with all of the topical β-blocking agents (Gross and Pineyro, 1997).
Apraclonidine and brimonidine are topical α2-agonists that decrease sympathetic tone and subsequently reduce aqueous humor production. Brimonidine, unlike apraclonidine, is capable of crossing the blood-brain barrier and should be used with great caution in young children. Bradycardia, hypotension, hypothermia, hypotonia, and apnea have all been reported with the use of brimonidine (Enyedi and Freedman, 2001).
Newer topical agents, including the prostaglandin analogues (latanoprost, bimatoprost, and travoprost) and the topical carbonic anhydrase inhibitors (dorzolamide and brinzolamide), are generally very safe in the pediatric population but are believed to be less effective than they are in adults (Beck, 2001). The topical carbonic anhydrase inhibitors, like systemic acetazolamide, are sulfonamide derivatives that should be avoided in the patient with sulfa sensitivity.
Miscellaneous Ophthalmologic Agents
Topical anesthetics, including cocaine, tetracaine, and proparacaine, are occasionally used by ophthalmologists in the perioperative setting. Cocaine is rarely used, but it is unique among the local anesthetics because of its vasoconstrictive properties. The potential for serious cardiovascular and central nervous system effects should be recognized by both the surgeon and anesthesiologist. The accepted maximum dose is 3 mg/kg, 1.5 mg/kg in the presence of volatile anesthetics. One drop of the 4% formulation contains approximately 1.5 mg of cocaine (McGoldrick, 1992b). The drug should not be used in patients with cardiovascular disease or in the presence of additional adrenergic-modifying medications such as monoamine oxidase inhibitors or tricyclic antidepressants.
Intraocular gases, including sulfur hexafluoride, perfluoropropane, and carbon octofluorine, are poorly diffusible inert gases that may be injected during certain vitreoretinal procedures. When nitrous oxide is present during injection, the nitrous oxide equilibrates with these new gas spaces to increase the volume and pressure of the intraocular injection, potentially compromising retinal perfusion. Animal studies, case reports, and mathematic models have demonstrated the necessity of discontinuing nitrous oxide no less than 15 minutes before intraocular gas injection and avoiding subsequent use of nitrous oxide for at least 4 weeks after the use of sulfur hexafluoride and 6 weeks after the use of perfluoropropane or carbon octofluorine (Wolf et al., 1983; McGoldrick, 1992b; Seaberg et al., 2002).
Effects of Various Anesthetic Agents on Intraocular Pressure
The central nervous system depressants (benzodiazepines, barbiturates, and opioids) commonly used by the anesthesiologist decrease IOP in both normal and glaucomatous eyes. The agents commonly used for preoperative anxiolysis in the pediatric population are associated with minor decreases in IOP that should not affect diagnostic measurements and likewise should not be relied on to attenuate the increase in IOP attributable to the use of succinylcholine and laryngoscopy. Effects specific to the use of oral or rectal midazolam in the pediatric population have not been delineated, although two studies of the use of intravenous (IV) midazolam in adults demonstrate minimal effects on IOP (Virkkila et al., 1992; Carter et al., 1999).
With the possible exception of ketamine, all of the IV induction agents are associated with a significant decrease in IOP. Thiopental and propofol reduced IOP by 40% and 53%, respectively, in one study, although both agents are unable to completely attenuate increases that are secondary to succinylcholine and laryngoscopy (Mirakhur and Shepherd, 1985; Mirakhur et al., 1987). Etomidate diminished IOP more profoundly than thiopental in one adult study (Calla et al., 1987). Etomidate-related myoclonus could be hazardous to the patient with traumatic injury and bothersome to the ophthalmologist. Early studies of the effects of ketamine uniformly demonstrated an increase in IOP, but subsequent studies in adults and children have demonstrated either insignificant changes or minor decreases in IOP (Peuler et al., 1975; Ausinsch et al., 1976). There is no clear consensus regarding the effects of ketamine on IOP, although its association with blepharospasm and nystagmus makes other induction agents more useful for ophthalmologic surgery.
All of the volatile anesthetics are associated with a dose-dependent decrease in IOP. Various postulated mechanisms include a reduction in aqueous humor production with a concomitant increase in outflow, relaxation of the supporting musculature, and depression of the central nervous system control center for IOP (McGoldrick, 1992c). As was previously demonstrated with halothane, reliable measurements of IOP may be made for approximately 10 minutes after mask induction with sevoflurane (Watcha et al., 1990; Yoshitake et al., 1993).
The deleterious effects of succinylcholine on IOP and the various methods of attenuating these effects have been evaluated by numerous investigators for several decades. The augmentation of IOP is thought to be mediated not only by tonic contractions of the extraocular muscles but also by dilation of the choroidal vasculature and relaxation of the orbital smooth muscle (Calobrisi and Lebowitz, 1990). In a study of patients undergoing elective enucleation, it was noted that the change in IOP after succinylcholine administration was the same in the normal eye as in the eye where the extraocular muscles were detached; therefore, it does not appear that extraocular muscle contraction significantly contributes to the increase in IOP after succinylcholine administration (Kelly et al., 1993). In adult patients with normal IOP, succinylcholine at doses between 1.5 and 2 mg/kg increased pressures by no more than 9 mm Hg, with peak effects demonstrated within 3 minutes after administration (Pandey et al., 1972). In patients who were not intubated, IOP was restored to baseline within 6 minutes, although other studies have demonstrated mild elevations that may persist for 30 minutes after succinylcholine administration. Whereas these effects of succinylcholine are significant in comparison with the effects of the nondepolarizing agents, they are clearly insignificant in comparison with the increase in IOP that is possible with laryngoscopy, coughing, and retching.
Numerous methods of blunting the rise in IOP secondary to succinylcholine and laryngoscopy have been evaluated, although none has demonstrated consistent or reliable efficacy. The results of early studies of pretreating patients with small doses of the nondepolarizing agents were promising but later refuted (Miller et al., 1968; Meyers et al., 1978). In two adult studies, the use of alfentanil was demonstrated to significantly attenuate the response to succinylcholine and intubation (Polarz et al., 1992; Eti et al., 2000). Another study comparing the effects of fentanyl and alfentanil demonstrated that although both agents were effective in attenuating the response to succinylcholine, fentanyl did not significantly attenuate the increase in IOP secondary to laryngoscopy (Sweeney et al., 1989). Early studies concerning the benefit of lidocaine before succinylcholine were discouraging, but lidocaine had favorable effects on IOP during laryngoscopy and intubation in subsequent investigations (Smith et al., 1979; Mahajan et al., 1987; Warner et al., 1989). The opioids and lidocaine may also facilitate gentle extubations after intraocular procedures and in patients with elevated IOP.
More contemporary methods of controlling IOP with the use of succinylcholine and laryngoscopy have been promising. Premedication with sublingual nifedipine and oral clonidine has demonstrated efficacy in the elderly population (Ghignone et al., 1988; Indu et al., 1989; Polarz et al., 1993). Intramuscular (IM) dexmedetomidine also effectively reduced IOP during regional anesthetic procedures in adults (Virkkila et al., 1994). None of these methods has been evaluated in the pediatric population.
More information regarding airway management and the effects on IOP are discussed in Chapter 30, Anesthesia for the Pediatric Trauma Patient. In addition, Vachon and others (2003) review the use of succinylcholine and the open globe.
General Anesthetic Considerations
Premedication
The value of premedication is well appreciated by all physicians providing anesthetic care to children. Premedication is useful to ease separation from parents and to provide for a smooth induction. Children between the ages of 1 and 6 years commonly benefit from premedication. Older children, especially those subject to repeated procedures, may also benefit from premedication or having a parent present during induction of anesthesia (Kain et al., 2006). Parental presence has also been shown to enhance the effects of oral midazolam on induction and emergence behavior (Arai et al., 2007). Oral midazolam (0.25 to 0.5 mg/kg) is commonly used and is generally effective within 10 to 20 minutes after administration (Coté et al., 2002). Nasal midazolam (0.2 mg/kg) may be useful in the patient refusing oral administration, but the acidity of the formulation is associated with a 71% incidence of burning and crying on administration (Karl et al., 1993). Oral clonidine (2 to 4 mcg/kg) also provides adequate anxiolysis within 30 minutes and has been demonstrated to decrease the incidence of PONV after strabismus surgery in two investigations (Mikawa et al., 1995; Handa and Fujii, 2001). In one study, oral clonidine was more effective than oral midazolam in multiple aspects of premedication, including acceptance by patients, more effective sedation, and better recovery from anesthesia (Almenrader et al., 2007). Neither midazolam nor clonidine consistently decreases the incidence of emergence delirium (Fazi et al., 2001; Valley et al., 2003). At recommended doses, neither of the agents should prolong the time required for discharge from the postoperative recovery unit.