CHAPTER 35 Anesthesia for Office-Based Pediatric Anesthesia
“A pediatrician’s dream of the ideal world would be to have individuals knowledgeable about the special needs of infants and children assembled wherever children are to be treated” (Avery, 1975). Little did Dr. Avery know back in 1975, as she wrote these words in the journal Anesthesiology as a guest editor introducing a symposium on pediatric anesthesia, to what extent and in what places children were to be anesthetized and by whom. The prophetic nature of her question, “Where will pediatric surgery be done in the future?” and her statement, “Surely the anesthetist should contribute to the definition of what can be done in what setting,” is astounding when considering how rapidly the surgical and anesthetic care of children has progressed from the hospital to the ambulatory surgery center to the office-based setting since Dr. Avery’s remarks (1975).
The concept of office-based anesthesia and surgery is not a novel one, because dentists, oral surgeons, and plastic surgeons have been using office-based procedures for decades. In fact, dentists and oral surgeons have been at the forefront of office anesthesia and surgery dating back to one of the first office-based anesthetics, involving Colton and Wells in 1844, for an extraction of a wisdom tooth (Jacobsohn, 1995; Yagiela, 1999).
Surgical practice has now come full circle, because before the early 1900s many surgical procedures were performed in offices. Subsequently, because surgical procedures became more complex, the hospital became the major site for surgery (Yagiela, 1999). Despite this shift, the development of ambulatory anesthesia continued throughout the twentieth century with the development of the first free-standing surgical center in 1916, by Waters, and ultimately with the first ambulatory surgery center established by Reed and Ford in the late 1960s (White, 1997).
Over the past several years, the concept of office-based anesthesia and surgery has become well publicized. In addition to the increasing number of clinical reports, professional society publications, review articles and texts looking at the efficacy or regarding the subject of office-based anesthesia, there are unfortunately numerous reports of significant morbidity and mortality, as well as near misses both in the medical and dental literature and in the lay press (LaMendola, 1998; Laurito, 1998; Schulte and Bergal, 1998; de Jong, 1999; Neergaard, 1999; Rao et al., 1999; Tang et al., 1999; Arens, 2000; Morrell, 2000; Stoelting, 2000; Vogt, 2000; Hilton, 2001; Joshi, 2003; Gooden, 2006; Kaushal et al., 2006; Hussain, 2006; Hausman and Frost, 2007; Shapiro, 2007; ASA, 2008a, 2008b, 2008c; Coldiron et al., 2008; Heard et al., 2009; Sherry, 2009). The initial reports of mortality in the office-based setting have been highlighted by the unexpected death of the mother of music celebrity Kanye West and consequent legislation in California (Carter, 2007; McGreevy, 2009).
Resident training in office-based anesthesia has also recently been advocated by some within the field of anesthesia. This information, along with the fact that there is an ongoing closed-claim analysis of office-based anesthesia and surgery within the American Society of Anesthesiologists (ASA) (lending itself to the knowledge that this entity does exist and that improvements to existing procedures have been started), must be compelling evidence for the anesthesiologist to realize that office-based surgery and anesthesia are here to stay (Domino, 2001; Hausman et al., 2006; Hausman, 2008; Posner, personal communication, January 2009).
Interest in office-based anesthesia is also manifesting in the increasing number of societies—specifically, the Society for Ambulatory Anesthesia (SAMBA), and the Anesthesia Patient Safety Foundation (APSF)—that promulgate educational and safety-related literature in this relatively new arena for anesthesiologists. Also, the ASA, as well as other groups including, but not limited to, The American College of Surgeons and various surgical subspecialty societies, the American Dental Association, the American Academy of Pediatric Dentistry, and the American Association of Nurse Anesthetists, have published guidelines specifically addressing office-based anesthesia or surgery or both (Table 35-1). Furthermore, the ASA Committee on Ambulatory Surgical Care and SAMBA have published a “how-to” manual for setting up a safe office environment (ASA, 2008d).
TABLE 35-1 Specialty-Specific Guidelines for Sedation and Analgesia and Office-Based Anesthesia and Surgery*
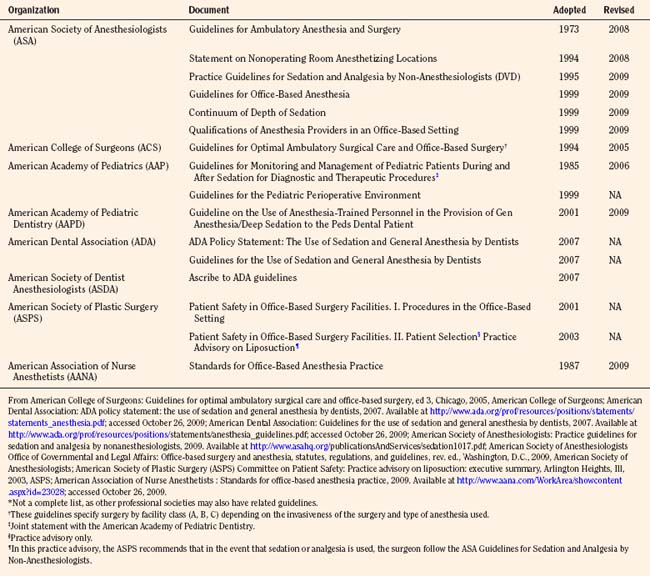
In an effort to establish consistency in the safe administration of sedation and anesthesia to children, some societies have established joint guidelines or updated guidelines outlining the use of anesthesia personnel to its membership (American Academy of Pediatrics, 2006; American Academy of Pediatric Dentistry, 2009). All of these societies have developed their guidelines or policies in response to the overwhelming interest and growing participation by their memberships in this area, as well as an overall common concern for patient safety.
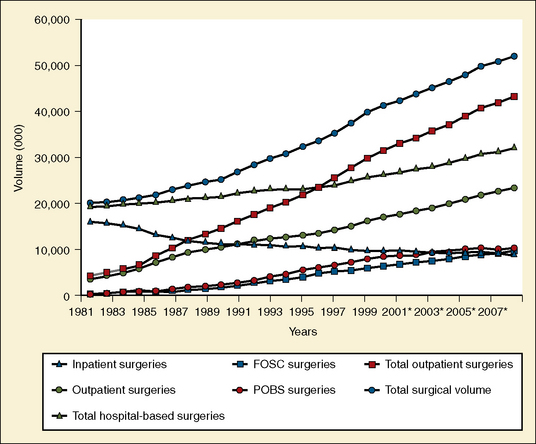
Estimates of the actual number of surgical cases completed, pediatric or otherwise, in an office setting, are difficult to ascertain. It is estimated that there were 10 million office-based surgical procedures performed in 2005, consistent with one marketing study from several years ago, that estimated that by 2006 the total number of outpatient procedures performed would be approximately 40 million, with 11 million of these being office-based procedures (Fig. 35-1) (SMG Marketing-Verispan, L.L.C., 2002; Twersky, 2008). In 2009, these numbers are holding steady; however, the dynamic nature of the reimbursement environment and the development of minimally invasive surgical technologies may make the number of office-based procedures skyrocket over the next several years.
According to a 2009 report from the National Center for Health Statistics, in 2006 there were approximately 35 million ambulatory surgery visits in the United States, with most of these being in hospital-based facilities vs. free-standing facilities (Cullen et al., 2009). Just over 7% of these reported ambulatory surgery visits were by children younger than 15 years of age. Although the total number of ambulatory surgery visits for this age group went up in 2006, the percentage decreased from the 8.5% reported for 1996 (Hall and Lawrence, 1998). As is suggested, without mandatory reporting of all ambulatory surgery procedures requiring anesthesia to a central agency, office-based anesthesia data will remain obscure (Perrott, 2008).
Although many different types of surgical procedures, including otolaryngologic, urologic, cosmetic, ophthalmologic, and radiologic (including single-photon emission computed tomography [SPECT]) scanning are performed on children in the office-based setting, the majority of procedures requiring anesthesia or sedation in the office setting for children are dental procedures (Cartwright et al., 1996; Goldblum et al., 1996; Grevelink et al., 1997; Yagiela, 1999; Siegel et al., 2000; Smith and Smith, 2000; Garin et al., 2001; Friedman et al., 2002; Ross and Eck, 2002; Barinholtz, 2009; Gravningsbraten et al., 2009).
The most common reason for children to require dental procedures is related to early childhood caries (ECC), with an incidence in primary teeth of 41% in children between ages 2 and 11 years (Beltrán-Aguilar et al., 2005). Furthermore, a majority of ECC in the United States occurs in children from low-income households. (Vargas et al., 1998; Nunn et al., 2009). Yagiela (1999) reports that a survey by the American Academy of Pediatric Dentistry estimated in 1995 that the number of children who received anesthesia for dental procedures was close to 200,000. Presently, the actual number of dental procedures performed with patients under general anesthesia is difficult to determine because of underreporting, and because estimates are generated from Medicaid-provided information of hospital-based care (Casamassimo et al., 2009). The actual number of children requiring anesthesia for these procedures may be significantly greater than this, with the discrepancy being because of a paucity of access to the appropriate care secondary to a lack of primary-care access and as important, a lack of insurance coverage. Significantly, this access to care can be positively impacted by state legislation. White and others (2008) report that non–Medicaid and Medicaid dental visits increased by approximately 60% and 30% (p < .05), respectively after the State of North Carolina introduced general-anesthesia legislation for preschool-aged children.
In a 2006 survey of Illinois dentists licensed to give some form of sedation or anesthesia, close to 116,000 cases were performed with some form of sedation and general anesthesia (Flick et al., 2007). Most of these sedation and anesthesia cases (90%) were performed by oral and maxillofacial surgeons (63% of survey respondents); however, general dentist and pediatric dentist respondents (29%) accounted for most of the remaining sedation and anesthesia. The number of pediatric patients cared for, however, was not specified.
Why office-based surgery and anesthesia?
As one can see from the information presented in Figure 35-1, there is a compelling need to be able to provide quality surgical and anesthesia services in the office-based setting. The actual reasons as to why this boom has occurred and continues to evolve and why anesthesiologists are more aggressively entering this arena are severalfold.
Ostensibly, the most persuasive argument for a paradigm shift to the office-based setting is financial. Potential and realized limitations and reductions in reimbursement because of health care reform and economic constraints are causing physicians to become more creative in facilitating cost-effective approaches to surgery. Costs can be reduced by reducing or eliminating facility fees that ordinarily accompany the cost-sharing charges at hospital-based and ambulatory surgery-based centers. Much of office-based surgery, especially cosmetic surgery, is performed on a cash-payment, fee-for-service basis, and therefore cost containment by limiting facility-fee overhead becomes crucial to patient affordability. This affordability is critical in the case of pediatric dental procedures, where in many instances, neither dental nor medical insurance covers out-of-office dental procedures and anesthesia costs (Ross and Eck, 2002).
One surgical study from the United States as early as 1994 compares the cost of performing an inguinal herniorrhaphy in the hospital with that of the cost in an office setting. This study finds the latter a more cost-effective alternative with a reduction in cost of a laparoscopic approach or an open approach of approximately 70% and 60%, respectively when compared with the hospital outpatient setting (Schultz, 1994). In one pediatric study, Lalwani and others (2007) show a per-patient savings of close to $5000 when patients with special health care needs who require anesthesia or sedation undergo dental rehabilitation procedures in an office-based setting when compared with those receiving care in a hospital operating room.
Safety and outcome
With the government, medical community, third-party payers, and the consumers (patients) pushing for more expeditious and cost-effective (and hence potentially more profitable) ways in which to provide surgical and anesthesia services, the anesthesia services provided are moving further away from the hospital safety net. Dr. Ervin Moss (1998), the impetus behind tighter regulation of office-based anesthesia and surgery in the state of New Jersey and perhaps beyond, stated, “Some say the major difference between the office-based and hospital-based anesthesiologist is that the former must be more courageous or foolhardy.”
Whether or not Dr. Moss’s characterization of the office-based anesthesiologist holds true, the fact remains that anesthesia care must be provided safely, if not more vigilantly, than hospital-based or surgery center-based anesthesia. Although some have questioned whether the convenience of office-based surgery and anesthesia is worth the risk, consensus opinion, as this specialty area continues to develop, is that it must be done correctly and consistently (Arens, 2000; Bridenbaugh, 2005).
Although anesthesia-related mortality risk continues to be difficult to assess, perhaps because of methodologic issues, it has nevertheless decreased over the past several decades (Lagasse, 2009). Anesthesia-related mortality risk in the United States has recently been quoted to range from 0.1: 10,000 to approximately 0.8:10,000 procedures performed (Biboulet et al., 2001; Lagasse, 2002, 2009; Newland et al., 2002; Li et al., 2009). These numbers appear slightly lower than the rate published outside the United States, at 1.12:10,000 cases (Braz et al., 2006).
In children, the incidence of cardiac arrest from anesthesia is reported to range from 1.4:10,000 to 4.6:10,000 with the incidence of anesthesia-related mortality being reported by some as between 1.2:10,000 and 7.7:10,000 cases in ASA Physical Status (PS) I-II and ASA PS III-IV, respectively (Morray et al., 2000). This disparity seen between patients of lower and higher ASA PS is consistent with morbidity statistics presented by Murat and others (2004) in a report of over 24,000 anesthesia cases over 2½ years and by Kakavouli and others (2009) in a study comparing adverse events for patients receiving anesthesia in the operating room (2.5%) with those outside the operating room (3.5%). Respiratory events were the leading cause in both studies, 1.7% and 1.9%, respectively (Zuercher and Ummenhofer, 2008; Bharti et al., 2009).
Interestingly, the number of pediatric arrests related to medications decreased almost 20% from 1994 to 1997 (37%) and from 1998 to 2004 (18%) as reported in an update on the pediatric perioperative cardiac arrest (POCA) registry (Bhananker et al., 2007). The authors suggest that this may be because of the decreased use of halothane in pediatric anesthesia. This is important in that the relatively newer, faster onset and offset (desirable characteristics in the office-based setting) volatile agents, sevoflurane and to a lesser extent desflurane, may confer a larger therapeutic index in the office-based setting. Furthermore, these authors report that airway causes for pediatric arrest still occur with a high incidence (27%), reemphasizing the importance of having superior airway management skills in pediatric anesthesia regardless of location.
Many of the cases brought to the attention of the medical, dental, and lay community involve children undergoing dental procedures (Morell, 2000; Hussain, 2006; Sherry, 2009). This information is not only tied intimately to the present topic but also is the point of origin for much of the controversy over the safety and efficacy of office-based anesthesia for children.
In two reports from the United States, Coté and others (2000a, 2000b) retrospectively analyzed information obtained from the Food and Drug Administration, the United States Pharmacopoeia, and a survey of pediatric specialists to report on contributing factors to critical incidents and medications used in sedation as they relate to adverse sedation events in children undergoing diagnostic and therapeutic procedures.
In the first report, Coté and others (2000a) reported on 95 incidents. Over half of these incidents resulted in death (n = 51) or permanent neurologic injury (n = 9). The remaining patients either had prolonged hospitalization without injury (n = 21) or sustained no harm as a result of the adverse event (n = 14). Of note was that those children who were cared for in non–hospital-based facilities (older and healthier) had a much higher rate of death and permanent neurologic injury (93%) than did those cared for in hospital-based facilities (37%). The authors also reported that inadequate resuscitation was a major factor in the non–hospital-based facilities (57%) compared with the hospital-based setting (2.5%) and that patients cared for in the nonhospital setting were more likely to sustain a cardiac arrest as the second or third event compared with those in the hospital setting (p < .001).
In the second report, Coté and others (2000b) used the same 95 incidents to determine whether there was a relationship between medications and adverse events. Although the authors noted no relationship between the class of drug used, the route of administration, and the incidence of death and permanent neurologic injury, they did note that adverse outcomes were associated with the administration of drug overdoses and administration of three or more sedating medications. Furthermore, 11 of 12 patients (all younger than 6 years of age) sustained adverse outcomes either at home or in a car. Two of the 12 patients, who had received sedative medication at home before their procedure, sustained an adverse event at home before the scheduled procedure.
Of note was that over one third of the reported events occurred during sedation for dental procedures (n = 32). Twenty-nine of these resulted in death or permanent neurologic injury. Most of the involved practitioners were either oral surgeons or dentists, three were pedodontists, and one was a nurse anesthetist under the supervision of a dentist. None of the practitioners was an anesthesiologist (Coté et al., 2000b).
Although these conclusions may seem intuitive to those who regularly care for children, they are reinforced by recent reports suggesting that severe adverse outcomes in pediatric sedation or analgesia outside the operating room may be improved by consistency in guidelines, training, and adverse-event reporting across institutions and specialties that are implemented through well-designed sedation services (Cravero et al., 2006, 2009; Bhatt et al., 2009). In the latter study, Cravero and others (2009) show that whereas the incidence of pulmonary events (e.g., stridor, laryngospasm, excessive secretions, and central and obstructive sleep apnea) is high, they report a low incidence for cardiopulmonary resuscitation (0.4:10,000) and no mortalities in approximately 50,000 sedation procedures performed by various nonanesthesiologist pediatric specialists. Lightdale and others (2006) advocate the use of microstream capnography to enhance the safety of pediatric patients undergoing procedures under sedation or analgesia via early detection of hypoxemia caused by alveolar hypoventilation.
Although there are anecdotal reports and studies of adverse outcomes, complications, and side effects related to sedation and anesthesia in the dental literature, others have reported on a safety record that is as good as, if not better than, that of the anesthesia community (Denman et al., 1968; Yee et al., 1985; Blayney et al., 1999; Girdler and Smith, 1999; Laskin, 1999; Saxen et al., 1999; Whitmire, 1999; Johnson et al., 2001; Manoharan et al., 2001; Yagiela, 2001; Perrott et al., 2003). The incidence of mortality rates in dental anesthesia is reported to be anywhere from 1:250,000 in the United Kingdom to 1:300,000 to less than 1:1 million in the United States (Cartwright, 1999; Brandom and Herlich, 1999; D’Eramo, 1999; Laskin, 1999).
As if there is not enough controversy within the anesthesia community, within the dental community there is also debate over who can best serve the patient requiring anesthesia for a dental procedure. Yagiela (2001) points out that members of the American Society of Dental Anesthesiologists, those who provide “approximately 25,000 pediatric general anesthetics per year,” subscribe closely to the American Academy of Pediatrics and American Society of Anesthesiologists guidelines for sedation and anesthesia. He also states that “since the organization’s inception 2 decades ago, there have been no known incidents of mortality or significant morbidity in children managed in the dental office by a dentist anesthesiologist” and intimates that safety may be improved in dental offices with a greater adherence to these guidelines by the dental community as a whole (Yagiela, 2001).
In contrast to the paucity of information about the safety and outcomes related to office-based anesthesia, the efficacy of anesthesia in pediatric ambulatory surgery in general is well known. As reported by Willetts and others (1997), outpatient surgery may date back to James H. Nicoll, a Glasgow surgeon who in the early 1900s successfully performed several thousand ambulatory procedures on young children at the West Graham Street Dispensary for Children. Contemporary literature continues to confirm over the past 50 years that for a growing variety of surgical procedures, the ambulatory setting for surgery and anesthesia is safe, cost effective, and therefore preferable to inpatient surgery (Postuma et al., 1987; Patel and Hannallah, 1988; Hannallah, 1991; Ghosh and Sallam, 1994; Blacoe et al., 2008; Shah et al., 2008; Mattila et al., 2009).
In one prospective study examining the efficacy of pediatric day surgery at the Children’s Hospital of Eastern Ontario, the overall complication rate was very low. The investigators, over 5 years, prospectively studied children undergoing various outpatient procedures, including myringotomy, tonsillectomy and adenoidectomy, dental procedures, and inguinal hernia repairs. Most of the children were between 2 and 7 years old, and the total number of cases approached 25,000. The reported complication rate was 1.6% per year. The most common complication was postoperative bleeding, primarily secondary to tonsillectomy and adenoidectomy. None of the complications resulted in permanent disability (Letts et al., 2001). In a retrospective study from Children’s National Medical Center focusing on pediatric otolaryngology procedures, Shah and others (2008) report that in close to 5000 cases (55% of total surgical cases) over 7 years, the rate of unanticipated outcomes was 0.2%. Similar to the previous study, the majority of adverse outcomes were related to posttonsillectomy and adenoidectomy bleeding.
Most of the information relative to the outcomes for office-based anesthesia and surgery is related to adult patients. In a retrospective report specifically looking at outcomes for plastic surgical procedures, Hoefflin and others (2001) reported no significant morbidity and no mortality over 18 years in more than 23,000 procedures in which general anesthesia was used. The anesthesia was provided by a board-certified anesthesiologist, and the single facility was accredited by the American Association for Accreditation of Ambulatory Surgical Facilities (AAAASF) (Hoefflin et al., 2001). In this report, most of the patients underwent cosmetic surgery, with some patients having multiple procedures. The only incidents reported as significant by the authors were the rare occurrence of electrocardiograph and oxygen-monitor failure. None of these events resulted in any patient complications, although three patients were hospitalized for custodial care. Minor anesthetic complications included nausea and vomiting (fewer than 5%), postextubation sore throat (fewer than 5%), shivering, one case of dental damage, one case of delayed (10 days) deep vein thrombosis, and one case of carpal tunnel syndrome after intravenous catheter infiltration.
In a retrospective study comparing outcomes in physician offices and ambulatory surgery centers in Florida, Vila and others (2003) found that despite new regulations imposed by the Florida Board of Medicine in the year 2000, between 2000 and 2002 there was a significantly increased risk of adverse incidents and deaths in offices (65.8:100,000 and 5.3:100,000, respectively) compared with ambulatory surgery centers (9.2:100,000 and 0.8:100,000, respectively). Furthermore, the authors estimated that a significant number of injuries and at least six deaths per year could have been prevented had all surgical cases been performed in an ambulatory surgery center.
In another report and as a follow-up study to previous reports, Coldiron and others (2008) reviewed critical surgical incidents that occurred in physicians’ offices in the state of Florida from 2000 to 2007 subsequent to mandatory reporting that began in February 2000 (Coldiron 2001, 2002). This mandatory reporting initially resulted from several newspaper accounts of poor patient outcomes and questions of whether office anesthesia and surgery were safe. Those incidents requiring reporting are listed in Box 35-1.
Box 35-1 Incidents in Surgical Offices Requiring Reporting by the State of Florida
From Coldiron B: Office surgical incidents: 19 months of Florida data, Dermatol Surg 28:710, 2002.
In the data obtained from Florida’s Agency for Health Care Administration, there were 31 deaths and 143 procedure-related complications and hospital transfers. Most of the bad outcomes occurred during “nonmedically-indicated” cosmetic surgery such as liposuction or liposuction with abdominoplasty. Plastic surgeons were responsible for 48% of all deaths and 52% of hospital transfers. Interestingly, most of the deaths (78%) occurred in ASA PS I patients. These authors note that the reported deaths and complications were unrelated to whether the physician was board certified or whether the physician had similar surgical privileges in a hospital (the latter being a mandatory requirement in some states). However, only 40% of facilities reporting adverse events were accredited by an independent agency. Despite the latter data, there are those who suggest that rigid state regulations and licensing laws along with accreditation of office-based surgical and anesthesia practices will help ensure patient safety (Kaushal et al., 2006).
Bitar and others (2003) retrospectively reviewed close to 5000 office-based plastic surgery procedures that were performed under monitored anesthesia care with sedation. The procedures in this study were performed by board-certified plastic surgeons, and anesthesia was provided by a CRNA. Nearly all patients were reported to be ASA PS I or II (99.9%), and the majority of patients were adult females (92%). The most common complications reported in this study were dyspnea (0.05%, n = 2), protracted nausea and vomiting (0.2%, n = 6), and unplanned hospital admission (0.05%, n = 2). One patient required intubation without prolonged sequelae. The author reported no cardiac arrests, deaths, or any incidence of deep vein thrombosis or pulmonary embolus. The author concluded that office anesthesia and surgery were safe when using appropriate protocols and patient selection.
Koch and others (2003) reported on several office-based anesthesia practices from various regions of the United States that were performed between 1981 and 2002. In this report, the authors noted no intraoperative deaths in over 64,000 anesthesia cases. Furthermore, in a subset of pediatric patients that comprised this report, one Chicago-based office anesthesia practice reported no intraoperative deaths, significant perioperative morbidity, or emergent hospital transfers in over 600 pediatric anesthesia cases. This number is now approximately 1200 cases and includes only one pediatric emergent hospital transfer (a possible malignant hyperthermia case). All complications continue to be minor, with a reported incidence of immediate and delayed PONV of less than 0.07% and 1%, respectively. Children in this subset ranged in age from 18 months to 17 years. Most of the children were younger than 6 years old and were classified as ASA PS I or II patients (Barinholtz, personal communication, 2009). These safety results are consistent with those reported by others caring for special-needs dental patients in the office-based setting (Caputo, 2009).
In a review of the ASA’s Closed Claims Project database, Domino (2001) compared claims (all age populations) made against anesthesiologists in the office setting (n = 14) with those made in other ambulatory surgery settings (n = 753). Claims for dental damage and for nonoperative pain management were excluded from this analysis. Although patient demographics were similar in both groups (Table 35-2), most of the claims in the office-based setting were related to plastic surgery or dental procedures, whereas in the ambulatory setting, most claims were related to procedures other than plastic or dental. The severity of injury appeared greater in the office-based setting compared with other ambulatory sites. In this initial report, most of the claims made in other ambulatory sites (62%) were for “temporary or nondisabling injury,” whereas most of the claims from the office-based setting were for death (64%). The author pointed out, however, that without a denominator, a true risk assessment for each site cannot be ascertained. Subsequent data from the ASA Closed Claims Analysis, with more claims in both the ambulatory (total, n = 877) and office-based settings (total, n = 29), continue to show a preponderance of death and brain damage in the office-based setting, although at a reduced (40%) incidence (Posner, personal communication, 2009). Likewise, Jimenez and others (2007), in a closed claims analysis of 532 pediatric cases from 1973 to 2000 (not exclusively ambulatory or office-based, but from 1990 to 2000 the highest percentage of the claims involved dental, otolaryngologic, and maxillofacial surgeries), found that death and brain damage were also the dominant injuries in malpractice claims, although the proportion of these claims decreased in the 10 years before 2001.
TABLE 35-2 Patient Characteristics in Analysis of Claims Made in Office-Based Anesthesia Incidents
| Ambulatory (n = 753) | Office Based (n = 14) | |
| Age (mean yr) | 41 | 45 |
| Female (%) | 58 | 64 |
| ASA PS class I/II (%) | 82 | 89 |
| Elective surgery (%) | 97 | 100 |
| Anesthesia type | ||
| General (%) | 66 | 71 |
| MAC (%) | 10 | 14 |
| Surgical procedure | ||
| Dental (%) | 3 | 21 |
| Plastic surgery (%) | 32* | 64* |
| Other (%) | 64† | 14† |
MAC, Monitored anesthesia care.
* p < 0.05, Ambulatory vs. office based.
† p < 0.01, Ambulatory vs. office based.
From Domino KB: Office-based anesthesia: lessons learned from the Closed Claims Project, ASA Newsletter, 2001, American Society of Anesthesiologists.
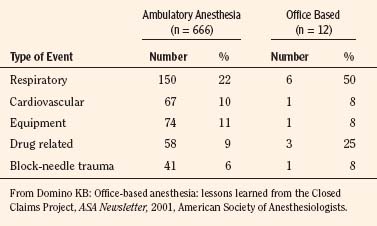
In both office-based settings and ambulatory settings, Domino (2001) noted that respiratory events were most common. A summary of airway-related complications and drug-related complications in office-based claims is shown in Table 35-3. Although the timing for injury was similar for both sites, there tended to be fewer claims for events occurring after discharge in the other ambulatory claims (7%) than for the office-based claims (21%).
The Closed Claims Project analysis also discloses that a greater number of office-based claims continue to be potentially preventable with better monitoring (Posner, personal communication, 2009). In the earlier report, a greater percentage of office-based claims involved substandard care compared with other ambulatory settings (not statistically significant), and payment was made in a higher percentage of claims (92% vs. 59%) and for a higher median payment ($200,000 vs. $85,000) for office-based claims than for other ambulatory settings (Domino, 2001).
Legislation and regulations
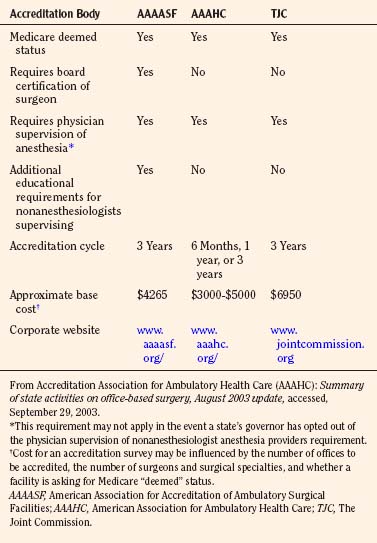
There are many entities presently imparting their influences on the practice of office-based anesthesia and surgery. These include, but are not limited to, state regulatory bodies; federal regulatory agencies such as the Centers for Medicare and Medicaid Services (CMS) and the Office of the Inspector General (OIG); national medical professional societies; national medical and safety organizations such as the Federation of State Medical Boards (FSMB, 2002), the National Committee for Quality Assurance (NCQA), and the National Patient Safety Foundation (NPSF); accrediting organizations such as the American Association for Accreditation of Ambulatory Surgery Facilities (AAAASF), the Accreditation Association for Ambulatory Health Care (AAAHC), and The Joint Commission; and the insurance industry. Also, in 2003, the AMA published the Core Principles for Office-Based Surgery that are currently endorsed by government agencies, the accrediting bodies, and specialty societies.
The main problem with regulation and legislation concerning office-based surgery and anesthesia is the wide regulatory variability that exists among states. Some states are highly regulated, whereas other states have no regulations (Fig. 35-2). In the states that do have regulations, these regulations are often ambiguous. State regulations regarding facility structure, personnel, equipment, and credentialing of individual practitioners differ widely. A more complete compendium of state regulations is available through the ASA Office of Governmental and Legal Affairs (ASA, 2009). In addition to state agencies and legislation, professional societies can regulate practice by establishing practice guidelines, practice standards, and advisories. The disadvantage of professional societies is that they run the risk of being self-interest groups. Consistent regulatory control could also be achieved by recognizing established accrediting bodies as oversight organizations. The organizations most commonly involved in the accreditation of ambulatory surgery centers are AAAASF, AAAHC, and The Joint Commission.
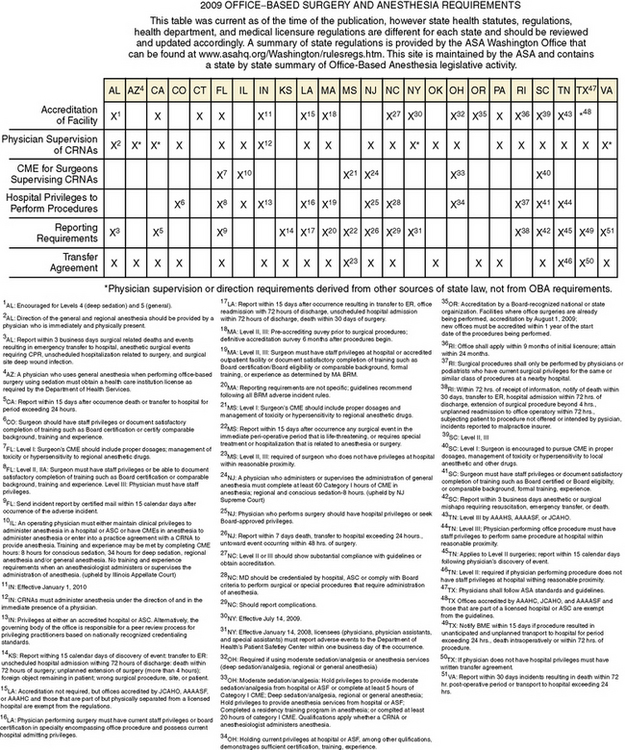
FIGURE 35-2 2009 Office-based surgery and anesthesia requirements.
(From ASA Office-based anesthesia: considerations for anesthesiologists in setting up and maintaining a safe office anesthesia environment.American Society of Anesthesiologists, 2008d.)
Historically, AAAASF, known until the early 1990s as the American Association for Accreditation of Ambulatory Plastic Surgery Facilities (AAAAPSF), was created to accredit only outpatient plastic surgery facilities. However, as other medical specialties moved procedures to free-standing outpatient settings, this organization became active in accrediting these facilities as well (AAAASF, 2003).
In contrast to AAAHC and The Joint Commission, AAAASF accredits facilities over a much narrower spectrum of medical specialties. The surgical specialties include colon and rectal surgery, obstetrics and gynecology, ophthalmology, orthopedic surgery, otolaryngology, plastic surgery, general surgery, and urology. AAAASF is particularly restrictive in its practitioner credentialing. This organization requires all surgeons to be certified by the American Board of Medical Specialties (ABMS) and requires all of its surgeons practicing at an ambulatory or office-based facility to have hospital privileges for the same procedures being performed in the office facility (AAAASF, 2003). AAAASF will only accredit a practice where the surgeons practice in their area of board certification. Furthermore, the AAAASF will not accredit an organization if propofol is not administered by an anesthesiologist or a properly supervised CRNA or anesthesia assistant.
In addition to defining requirements for surgical personnel, all three organizations offer accreditation processes that outline expectations for the facilities as they relate to meeting standards for the facility physical plant (e.g., by ensuring that state, local, Occupational Safety and Health Administration [OSHA], and National Fire Protection Association regulations are followed), anesthesia administration, monitoring, equipment and personnel, ancillary staff, patient transfer policies, patient safety and emergency resuscitation issues, quality improvement, and patient satisfaction issues. A summary of some of the similarities and differences between the three most visible accrediting organizations is given in Table 35-4.
Whether accreditation affects outcomes in office-based surgery and anesthesia is uncertain. In a survey study, the AAAASF sent a questionnaire to its accredited facilities that addressed patient safety in plastic surgery office facilities. Two hundred forty-one of 418 facilities responded to the questionnaire. Over 5 years 400,000 surgical procedures were studied, and the authors reported the risk of significant complications to be 1:213 and the risk of death to be 1:57,000 cases. They concluded that overall risk in an accredited office is comparable with that of other ambulatory surgery sites (free-standing or hospital based) (Morello et al., 1997). In a retrospective review of an accredited office-based plastic surgery facility, Byrd and others (2003) reported no deaths in over 5000 cases. However, these authors noted that several patients required hospital admission for various medical problems.
Clinical aspects
Patient and Procedure Selection
Because most office-based procedures for pediatric patients involve dental procedures, a majority of the children undergoing these procedures are older than 1 year of age. However, as the realm of office surgery for children expands (including tonsillectomies), and because there are no prospective studies as yet in the office-based anesthesia literature looking at outcomes and patient age for children undergoing office-based surgery, it seems that the present guidelines for other ambulatory surgery venues should be used (Gravningsbraten et al., 2009). When taking this latter point into consideration, the minimum age requirement (other parameters such as type of procedure not withstanding) for children undergoing office-based procedures can be determined by whether a child requires prolonged postoperative monitoring based on postconceptual age or the administration of opiate analgesics and other respiratory depressant agents (Welborn and Greenspun, 1994; Galinkin and Kurth, 1998). Although postanesthesia care unit (PACU) complications resulting from respiratory complications may be more common in neonates and infants, any other minimum age requirements are often arbitrary and may reflect the comfort level of the surgeon, office staff, and anesthesia personnel caring for the child (Westman, 1999; Ross and Eck, 2002; Murat et al., 2004). Adherence to policies and guidelines set forth for minimum age requirements for outpatient anesthesia in ambulatory surgery centers and hospital-based ambulatory surgery departments is critical.
Most children cared for in the office-based setting are ASA PS I and II patients. In some situations, it may be acceptable to provide anesthesia care for those children with stable comorbidities who are ASA PS III patients despite the fact that these patients in general may be more susceptible to adverse outcomes from anesthesia (Morray, 2002; Murat et al., 2004; Jimenez et al., 2007). Not surprisingly, getting consensus from pediatric anesthesiologists as to which comorbidities are appropriate for hospital-based or free-standing ambulatory surgery is difficult, but some of the pediatric comorbidities considered high risk for the office-based surgical suite are listed in Box 35-2 (Abu-Shahwan, 2007).
In an early prospective study looking at prolonged recovery stay and unplanned hospital admission after ambulatory surgery in pediatric patients, the authors reported annual rates of approximately 4% and 2%, respectively. PONV and respiratory complications were the most common factors leading to prolonged recovery stay, whereas respiratory complications (32%) and surgical reasons (30%) were the factors most commonly responsible for unplanned hospital admission. These authors also found that higher ASA physical status had a direct relationship to unplanned hospital admission and adverse respiratory events (D’Errico et al., 1998).
Subsequently, Dornhoffer and Manning (2000), in a retrospective chart review, evaluated unplanned hospital admission after four types of otologic procedures (not including myringotomy tube placement) in adult and pediatric outpatients. The unplanned hospital admission rates for children and adults were 5.7% and 2.3%, respectively. The most common reason for unplanned hospital admission was PONV. These findings are relatively consistent over time, and in a more recent study, Blacoe and others (2008)

Full access? Get Clinical Tree