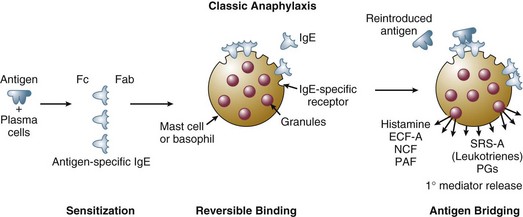
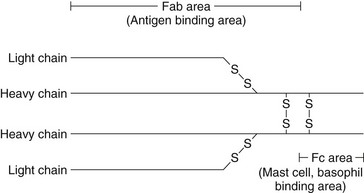
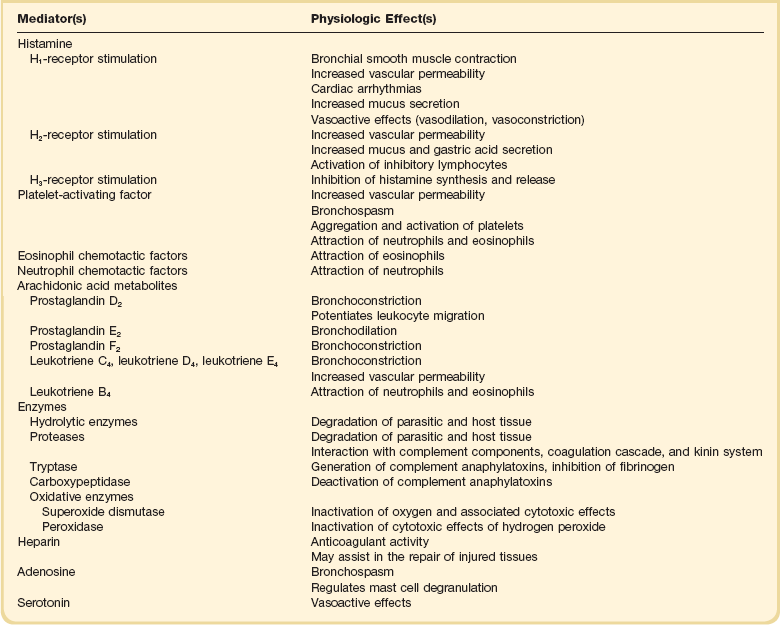
28 PATHOGENESIS AND PATHOPHYSIOLOGY Immunologic Events Leading to Mast Cell and Basophil Activation and Mediator Release Nonimmunologic Events Leading to Mediator Release Cellular Characteristics of Anaphylaxis Biochemical Mediators of Anaphylaxis Biochemical and Pharmacologic Regulation of Mediator Release Pathophysiologic Effects of Mediators CLINICAL AND HEMODYNAMIC FEATURES The term anaphylaxis refers to a life-threatening event, allergic in nature, which may result from IgE- or non-IgE-mediated mast cell degranulation. The clinical manifestations of severe anaphylaxis are often explosive in onset and may lead to upper airway obstruction, respiratory failure, and circulatory shock. Milder symptoms can also develop. The term anaphylactoid reaction, which referred to a non-IgE-mediated reaction, is no longer being used. A recent National Institutes of Health (NIH) consensus conference defined anaphylaxis as one of the following three scenarios.1 1. Acute onset of a reaction (minutes to hours) with involvement of the skin, mucosal tissue, or both and at least one of the following: (a) respiratory compromise (b) or reduced blood pressure or symptoms of end-organ dysfunction; 2. Two or more of the following that occur rapidly after exposure to a likely allergen for that patient—involvement of the skin/mucosal tissue, respiratory compromise, reduced blood pressure or associated symptoms, and persistent gastrointestinal symptoms; or 3. Reduced blood pressure after exposure to a known allergen (adapted from Sampson and colleagues1). The IgE-mediated anaphylactic response is classified as a type I reaction according to the Gell and Coombs classification. The IgE-mediated anaphylactic reaction has clinical features similar to other, milder type I reactions, such as allergic rhinitis, hives, urticaria, and allergic asthma. IgE-mediated anaphylactic reactions are characterized by a well-defined immunologic sequence of events that involves antigen-specific and IgE-specific effector cells. When stimulated, these cells release a variety of inflammatory mediators.2 The effector cells consist of mast cells and basophils, which are based primarily in tissues and in the circulating blood volume. Severe anaphylaxis rapidly progresses to a generalized systemic reaction. Agents that produce well-documented IgE-mediated anaphylactic reactions include medications such as beta lactam antibiotics, biologic agents, nonsteroidal anti-inflammatory drugs (NSAIDs), foods (peanut and other legumes, nuts from trees [walnuts, almonds, etc.], milk, and egg), Hymenoptera venoms (honey bees, yellow jackets, hornets, wasps, and fire ants), natural rubber latex, occupational allergens, and seminal fluid prostate-specific antigen (Table 28.1). Table 28.1 Agents Frequently Associated with Immune and Nonimmune Types of Anaphylaxis Immune-mediated IgE-dependent or IgE-independent and non-immune-mediated mast cell degranulation-mediated anaphylactic reactions have similar clinical features. Agents capable of producing direct mast cell degranulation include NSAIDs, opiates, ciprofloxacin, and physical factors, (cold, heat, exercise). Patients who are taking beta blockers or ACE inhibitors may develop severe anaphylaxis to an inciting agent and are less likely to respond to first-line agents.3–6 In idiopathic anaphylaxis, the pathophysiology and triggering events are unknown. Idiopathic anaphylaxis is a diagnosis of exclusion. It is mostly seen in adults and adolescents. About half these patients have concomitant atopic disease. They respond to treatment with corticosteroids and antihistamines.7,8 Special testing like serum tryptase, C4 levels may be necessary to exclude conditions such as systemic mastocytosis, hereditary angioedema, and acquired C1 inhibitor deficiency. Allergic emergencies have been described in humans since ancient times.9–11 At the turn of the twentieth century, a more detailed description of these events was reported by two French physiologists, Portier and Richet.12 They coined the term anaphylaxis, which originates from the French word anaphylactique, which means “reverse protection.” It was believed that these reactions were in contrast to the attenuated or tachyphylactic reactions that commonly protect subjects from reintroduced antigens such as viruses. More recent research defining the role of IgE; the interactions between IgE, antigen, mast cells, basophils, and eosinophils; and the biochemical mediators from these cells has clarified the events leading to clinical anaphylaxis.2,13–15 The true incidence of the various types of anaphylactic reactions is difficult to determine because these reactions are often spontaneous and unpredictable and are clinically similar to other acute reactions. Lifetime prevalence of anaphylaxis due to all triggers is estimated to be 0.05% to 2%.16 Estimates of the incidence of the most commonly reported episodes are possible, however. In the United States, penicillin alone probably accounts for several hundred fatalities each year.17–19 Anaphylaxis to the cephalosporins also is commonly reported.20 It has been estimated that among patients with an allergic reaction to a penicillin, there is a 3% to 7% rate of allergic reaction to a cephalosporin. Reports of anaphylactic reactions to the newer β-lactam antibiotics are accumulating.21 Insects, especially those of the Hymenoptera order, which includes bees, wasps, hornets, and fire ants, account for numerous immediate hypersensitivity reactions. About 3% of adults and 1% of children are affected and the anaphylaxis can be fatal at the first sting. About 50 people experience fatal reactions to insect stings every year in the United States, and about half of them do not have a prior sting exposure.22–24 Fire ants are aggressive insects from South America that now reside in the southern United States. In some areas, they have been known to sting 58% of the residents yearly and account for serious allergic reactions.25 Snake bites account for probably a dozen or so anaphylactic deaths per year in the United States. Snake bites may be associated with typical anaphylactic symptoms and other problems related to the enzymes, proteins, and peptides in venom. Local tissue necrosis, coagulation problems, hemolysis, and neurologic transmission defects have been described. In the United States, most anaphylactic reactions to snake bites are caused by pit vipers. These snakes include rattlesnakes, water moccasins, and copperheads.26,27 Food-induced anaphylaxis is probably the most common cause of anaphylaxis and accounts for 30% of fatalities. Peanuts (legumes) and typical nuts from trees account for 90% of fatal cases. Additional common food antigens include fish, soybeans, egg whites, and shellfish.28 Biphasic reactions are much more common in food-induced anaphylaxis than in other types of anaphylaxis and have been reported in 25% of fatal cases.29–31 Iodinated contrast agents account for approximately 125 deaths per year32 and lead to clinical symptoms similar to anaphylaxis. Life-threatening reactions are extremely rare, with an incidence of 0.1%.33,34 With the advent of low osmolar iodinated contrast agents, the risk of anaphylaxis to contrast agents has decreased drastically.35 Latex, used in surgical gloves, balloons, condoms, rubber bands, and many other products, may produce anaphylaxis.36,37 The use of universal precautions as a result of the acquired immunodeficiency syndrome epidemic has increased the number of reactions to latex in health care workers. Children with spina bifida and genitourinary tract abnormalities are especially susceptible to latex-induced anaphylaxis because of frequent exposure to latex-containing bladder catheters and other products. Anaphylactic reactions during anesthesia have been described and typically are associated with hypotension and cardiopulmonary arrest. One review suggests that most cases of intraoperative anaphylaxis are from muscle relaxants (e.g., suxamethonium, tubocurarine, pancuronium).38 Latex, protamine, and blood products also may cause intraoperative anaphylaxis. Anaphylaxis and other types of IgE-mediated allergic reactions tend to occur in susceptible, genetically predisposed individuals. The reason for the genetic inheritance of sensitivity to the antigens that produce anaphylaxis continues to be speculative. A popular theory is that type I reactions, when confined to an area of parasitic invasion (e.g., intestinal tract), facilitate the killing and removal of parasites and confer a survival advantage to individuals capable of mounting a type I response. Various clinical and laboratory observations support this view.39–41 The sites of IgE synthesis in laboratory subjects correspond to the sites of entry of many parasites. These sites include the lymphoid tissue of the respiratory tract, the gastrointestinal tract, and the skin. Eosinophils, cells that migrate to the site of antigen introduction in anaphylaxis, elaborate mediators that are toxic to the outer parasitic covering. When an antigen to which an individual has previously been sensitized is reintroduced, a sequence of events is initiated that leads to mediator release (Fig. 28.1). At least several weeks are required between the initial exposure to antigen and a subsequent exposure for clinical manifestations of anaphylaxis to occur. The antigen may be introduced through the skin, respiratory tract, or gastrointestinal tract. Antigen also may be introduced intravenously, usually in association with drug administration. Although most venoms are injected subcutaneously, some may access the circulation through an intravascular route. In most cases of anaphylaxis, when antigen is reintroduced into the host, it encounters IgE, previously synthesized by plasma cells in response to a previous introduction of antigen. IgE, similar to other immunoglobulins, is composed of two heavy chains and two light chains linked by disulfide bonds. Two portions of the molecule have well-defined functions. The Fab portion of the molecule recognizes and binds antigen. The Fc portion of the molecule binds reversibly to receptors on the surface of mast cells and basophils (Fig. 28.2). The combination of reintroduced antigen with antigen-specific IgE sets the stage for a sequence of biochemical and cellular events that produce the clinical syndrome of anaphylaxis. The bivalent antigen cross-bridges two IgE molecules (see Fig. 28.1). Cross-bridging facilitates the approximation of Fc surface receptors on mast cells and basophils, triggering the release of mediators from intracellular granules and membrane-based phospholipids. The systemic release of these mediators leads to the pathophysiologic changes that produce the clinical manifestations of anaphylaxis. Clinical reactions similar to anaphylaxis mediated by immunoglobulins of the IgG class have been described. IgG molecules may combine with antigens, producing an antigen-antibody complex that activates complement. Activation of complement generates C3a and C5a, also known as anaphylatoxins because they stimulate mediator release from mast cells and basophils. IgG-mediated reactions are considered type III reactions according to the classification of Gell and Coombs or may be referred to as Arthus reactions. These reactions may characterize IgA-deficient individuals who exhibit sudden reactions to blood transfusions. These individuals may develop an antibody of the IgG class to the IgA in the transfused blood product.42,43 This combination of IgG and IgA antibody activates complement, generates C3a and C5a, and produces a sudden reaction typical of anaphylaxis. Because approximately 1 in 700 individuals is IgA deficient, numerous people are susceptible to this type of blood transfusion reaction.43 The anaphylactic responses to protamine may be IgG-, IgE-, or non-immune-mediated.44–46 The mediators released during nonimmune reactions originate from mast cells and basophils and are identical to the mediators of immune-mediated anaphylaxis. The direct activation of surface receptors on mast cells and basophils by antigen may be responsible for mediator release in these reactions. Iodinated contrast agents, opiates, and highly charged polyionic antibiotics seem to activate surface receptors directly. Physical stimuli, including heat, cold, and hyperosmolar stimuli, also are capable of stimulating mast cells and basophils. Exercise-induced anaphylaxis may be associated with the stimulation of mast cells through cooling of the airways. Other possible mechanisms include complement activation without immune complex mediation (old preparations of propafol with cremophor diluent),47 direct mast cell degranulation (merperidine),48 and direct activation of the kinin-kallikrein pathway, resulting in the generation of bradykinin, C3a, and C5a (oversulfated chondroitin sulfate in heparin products).49 Despite the release of similar mediators during anaphylaxis, mast cells and basophils differ in several ways. Mast cells are more abundant than basophils and generally reside in the connective tissue of subcutaneous and submucosal areas. Basophils characteristically circulate in the blood.50 Despite these differences in location and number, functional differences between the two cell types have not been clearly identified. Both types of cells have receptors for the Fc portion of IgE, and both have granules that bind basic dyes. In addition, the granules of both cells contain histamine and various other mediators that participate in the anaphylactic response. Eosinophils are commonly identified in the tissues and plasma of patients with both immune- and non-immune-mediated anaphylactic reactions. These cells typically migrate to the site of antigen introduction. They are attracted by a variety of chemotactic factors, including factors derived from mast cells and basophils, antigen-antibody complexes, histamine, and complement. The granules of eosinophils stain with acidophilic dyes and contain a variety of biochemical mediators that are toxic to helminthic parasites. Substances that inactivate leukotrienes and histamines also are elaborated. Eosinophils function as modulators of the inflammatory response triggered by mast cell and basophil activation.51,52 The biochemical mediators of anaphylaxis are divided into primary and secondary mediators. Mediators directly released from mast cells and basophils are termed primary mediators (Table 28.2). Secondary mediators are released from other cell types in response to primary mediator release (Table 28.3). Primary mediators are subdivided further into preformed and newly synthesized mediators. Preformed mediators are formed and stored in the intracellular granules of mast cells and basophils. Newly synthesized mediators are derived from the metabolism of arachidonic acid, a phospholipid derived from cell membrane. Table 28.2 Physiologic Effects of Primary Mediators of Anaphylaxis Derived from Mast Cells and Basophils Table 28.3 Secondary Mediators of Anaphylaxis and Physiologic Effects
Anaphylaxis and Anaphylactic Shock
Category
Examples
Antibiotics
Penicillin and penicillin analogues, β-lactam antibiotics, cephalosporins, tetracyclines, erythromycin
Nonsteroidal anti-inflammatory drugs
Salicylates, ibuprofen, indomethacin
Narcotic analgesics
Morphine, codeine, meprobamate
Local anesthetics
Procaine, lidocaine, cocaine
General anesthetics
Thiopental
Muscle relaxants
Suxamethonium, tubocurarine, pancuronium
Blood products and antisera
Red blood cell, white blood cell, and platelet transfusions; gamma globulin; rabies, tetanus, diphtheria antitoxin; snake and spider antivenom
Diagnostic agents
Iodinated radiocontrast agents
Foods
Eggs, milk, nuts, legumes (peanuts, soybeans, kidney beans), fish, shellfish
Venoms
Bees, wasps, hornets, fire ants, scorpions, snakes
Enzymes and other biologic agents
Acetylcysteine, pancreatic enzyme supplements, chymopapain
Extracts of potential allergens used in desensitization
Pollen, food, venom extracts
Chemotherapeutic agents
Cisplatin, cyclophosphamide, daunorubicin, methotrexate
Insulin
Pork, beef, and human insulin
Other drugs
Protamine, chlorpropamide, parenteral iron, iodides, thiazide diuretics
History and Incidence
Pathogenesis and Pathophysiology
Immunologic Mechanisms Leading to Mast Cell and Basophil Activation and Mediator Release
Nonimmunologic Events Leading to Mediator Release
Cellular Characteristics of Anaphylaxis
Biochemical Mediators of Anaphylaxis
Mediator(s)
Physiologic Effect(s)
Neutrophil, platelet, and eosinophil-derived mediators
Permeability, coagulation changes, proteolysis
Activated complement system
C3a and C5a
Contract bronchial smooth muscle; increase vascular permeability; attract neutrophils, macrophages, and monocytes
C6-C9
Membrane damage
Activated coagulation cascade
Intravascular coagulation, permeability changes, tissue injury
Activated kinin system (bradykinin)
Increases vascular permeability

Full access? Get Clinical Tree


Anaphylaxis and Anaphylactic Shock