• Compressions and circulation
• Check for a pulse
• If a pulse is present, continue rescue breathing
• Reassess pulse every 2 min
• If a pulse is not present within 10 sec or pt shows signs of poor perfusion, begin chest compressions
• Chest compressions (should now be before airway/breathing)
• Initiate immediately
• Minimize interruptions between compressions
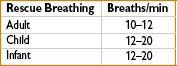
• Adult, child, and infant
• Continuous ventilation @ 8–10 breaths/min
• Continuous compressions @ 100/min
• Resume CPR immediately after defibrillation
• Complete chest recoil between compressions
• If 2 rescuers present, switch roles every 2 min to prevent fatigue
• Continue cycles of CPR until a defibrillator or additional help arrives
• Rhythm checks should not be longer than 10 sec
• Should be done after 5 cycles of CPR have been completed (2 min)
• Pulse checks should be done only if an organized rhythm is restored
• Drug administration and definitive airway placement should minimally interrupt compressions
• Airway/breathing
• Maintain patent airway, give supplemental oxygen
• Place advanced airway
• Minimize interruptions of chest compressions during placement
• Continuous waveform capnography should be used for confirmation & maintenance of ETT placement
• After airway placed, 2 providers should administer continuous CPR (not in cycles)
• Intravascular access should be obtained
• Intravenous—peripheral or central (faster med onset, but may interfere with CPR)
• Intraosseous (IO) access—may be safely used if difficult IV access
• Endotracheal route—not desirable, last resort if IV or IO cannot be obtained
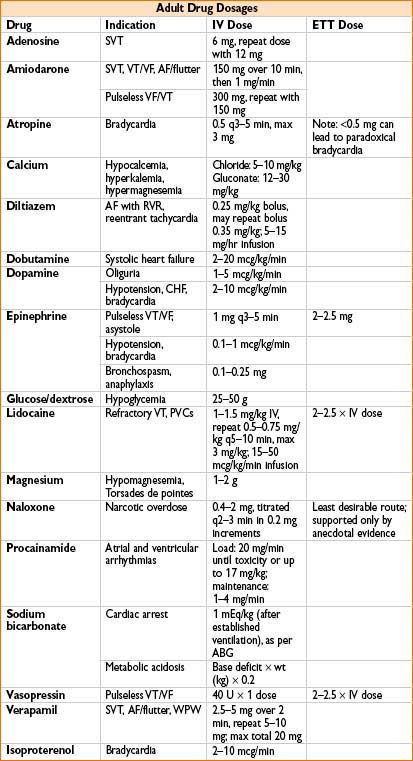
• Dose: 2–2.5 × standard IV dose diluted in 5–10 mL NS
• Drugs OK via ETT → lidocaine, atropine, epi, vasopressin, narcan
• Defibrillation
• Prompt defibrillation is critical when a patient displays a shockable rhythm
• Initial dose for biphasic is 120–200 J; monophasic is 360 J; 2 J/kg in peds (1–8 yrs)
• Differential diagnosis—diagnose and treat throughout resuscitation
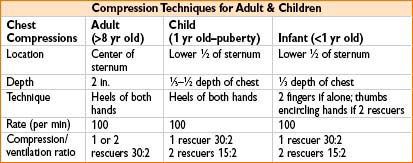
Figure 34-1. ACLS: Adult cardiac arrest.
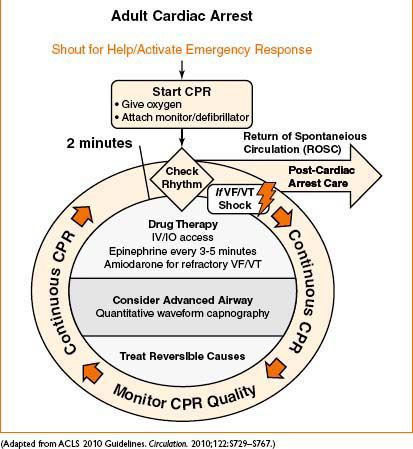
Figure 34-2. ACLS: Adult cardiac arrest.
Figure 34-3. ACLS: Bradycardia algorithm.
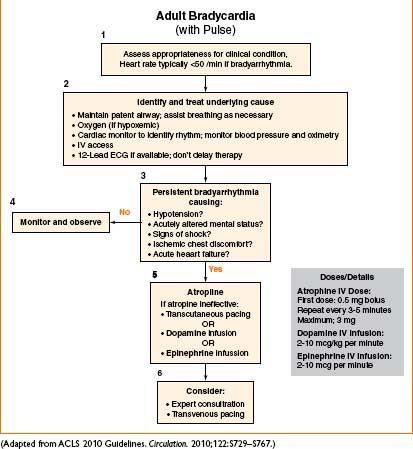
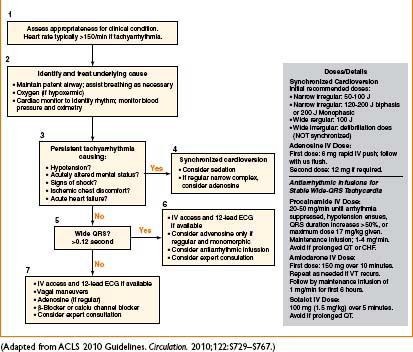
Figure 34-4. ACLS: Tachycardia with a pulse algorithm.

Full access? Get Clinical Tree








