Chapter 6 Airway Pharmacology
I Introduction
1. Pharmacodynamics: concerned with drug action, both positive (efficacy) and negative (toxicity)
2. Pharmacokinetics: concerned with optimal delivery and removal of the drug from sites of action (the biophase)
3. Pharmacoeconomics: concerned with cost-effectiveness in the selection of drug.
II Airway Pharmacology in Normal Airway Physiology
A Clinical Issues
B Physiology of the Upper Airway
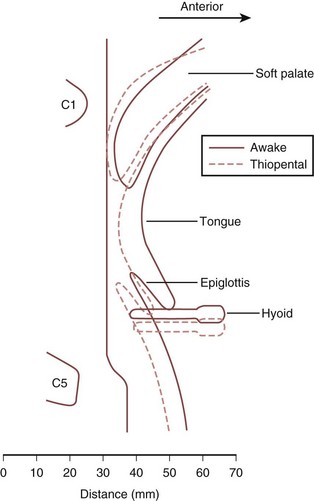
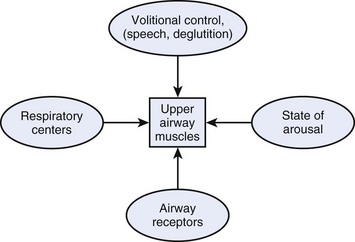
Physiology of the upper airway is considered in detail in Chapter 5. In the awake patient, airway patency is maintained by muscle tone in the head and neck, particularly the pharynx and tongue. The upper airway muscles are influenced by afferent information from a number of sources (Fig. 6-1), including receptors in the upper airway and lung that respond to changes in airway pressure and a variety of chemical and mechanical stimuli.
4 Voluntary Regulation of Airway Patency
Factors involving voluntary regulation of airway patency include speech and swallowing.
C Effects of Drugs on the Airway
1 Direct Effect
Several types of drugs can be administered topically to the airway.
1. Local anesthetics attenuate the afferent limbs of the powerful reflexes that serve to protect the upper airway from aspiration of foreign material.
2. Sympathomimetics, such as epinephrine and phenylephrine, cause local vasoconstriction to minimize tissue vascularity or reduce edema.
3. Volatile inhalational agents cross the alveolar-capillary membrane to have an indirect effect on the respiratory tract via the CNS, but they also have direct effects, including bronchodilation and mucosal irritation.
4. Bronchodilators are commonly administered topically, as reviewed in the second part of this chapter.
2 Indirect Effect
1. Sedatives and analgesics affect central and peripheral neurologic pathways, largely motor but also sensory, to lessen muscle tone in the upper and lower airways and thereby affect patency and gas flow. Secondary effects on O2 and CO2 tension also affect airway tone.
2. Neuromuscular blocking (NMB) agents clearly affect skeletal muscle tone and have a major influence on airway management under general anesthesia.
3. Lidocaine, given intravenously, affects airway reactivity.
4. Antihistamines, used topically in the treatment of rhinitis, can be administered systemically to attenuate histamine-induced reflex bronchoconstriction.
5. Antimuscarinics, such as atropine, inhibit the parasympathetic nervous system to reduce salivary gland secretions and dry the upper airway. Upper airway tone is not significantly affected by this antiparasympathetic action, but lower airway resistance is reduced and airway reactivity is attenuated when drugs such as ipratropium bromide are given parenterally or are inhaled.
6. Respiratory stimulants, such as doxapram, are used occasionally to provoke spontaneous respiratory effort on cessation of general anesthesia. IV doxapram stimulates chemoreceptors in the carotid arteries, which in turn stimulate the respiratory center in the brainstem to increase respiratory muscle activity. Potentially serious side effects include cardiovascular instability and cerebral irritation.
III Drugs with a Direct Effect on the Airway
A Local Anesthetics
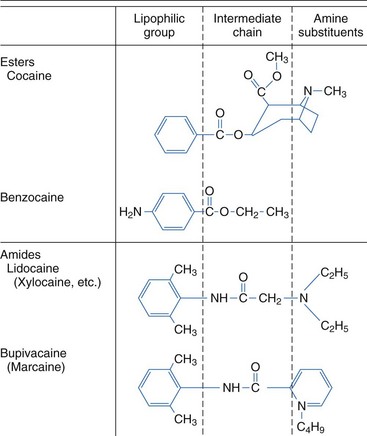
Local anesthetics produce a rapid, reversible depression of nerve conduction, particularly with regard to sensory nerves, by binding to sodium channels and interfering with their function, thereby preventing propagation of action potentials. Chemically, they usually consist of a lipophilic group connected to an ionizable group, typically a tertiary amine, by either an ester or an amide link (Fig. 6-2).
1 Complications of Airway Local Anesthesia
A reduction in upper airway patency has been demonstrated after topicalization of the airway.1,2 This occurs because of the loss of afferent feedback and the resultant decrease in motor tone, which may lead to upper airway obstruction, particularly in an airway that is already compromised. Hence, care is needed when considering an awake airway management technique in a patient with evidence of upper airway narrowing.
Systemic toxicity is extremely rare in patients receiving local anesthesia for instrumentation or examination of the upper or lower airway. Most reports suggest that plasma lidocaine levels very rarely approach the reported toxic plasma concentration of 5 to 6 µg/mL. However, one study demonstrated near-toxic levels after gargling of large volumes of lidocaine.3 Toxicity tends to involve the CNS with irritability or convulsions and the cardiovascular system with circulatory compromise. The safe maximum dose for airway administration for the most commonly used agent, lidocaine, is uncertain, but in one study in which patients received 9 mg/kg lidocaine, none had plasma concentrations in excess of 5 mg/mL.4 However, the death of a healthy volunteer due to presumed lidocaine toxicity after topicalization for fiberoptic bronchoscopy has been reported in the literature, so some consideration of the dose administered is advisable.5 The British Thoracic Society recommendation for the use of topical lidocaine with a flexible fiberoptic bronchoscope in adults is not to exceed 8.2 mg/kg.6
2 Specific Local Anesthetic Agents
d Cocaine
Cocaine, available in solutions of 1% to 10%, provides excellent topical anesthesia and has the advantage of providing intense vasoconstriction, which is often desirable as part of topicalization of the nasal passages before intubation. However, concerns about sympathomimetic toxicity and abuse potential have reduced its use in recent years, particularly in children, since a fatality was reported.7
B Sympathomimetics
The use of sympathomimetics to influence vascular blood flow in airway mucosal vessels is a technique that is commonly used in cases of acutely compromised upper airway in an attempt to reduce swelling. The most common agent used for this purpose is epinephrine, administered via a nebulizer.8 Vasoconstrictors such as phenylephrine are also used electively to reduce the potential for bleeding during upper airway instrumentation (e.g., nasotracheal intubation).
Topical vasoconstrictors such as epinephrine can also be used to minimize systemic absorption of topical local anesthetics and thereby reduce toxicity, improve efficacy, and increase duration of action.9 Unwanted effects of sympathomimetics are uncommon and largely relate to systemic absorption of the drug, which can result in an increase in cardiac work.
C Inhaled Volatile Agents
Inhaled anesthetic agents have a number of direct effects. For example, all volatile agents cause bronchodilation (i.e., increase in the diameter of the lower airways). Isoflurane appears to have the most potent effect, whereas desflurane also has the potential to cause the reverse effect and induce airway constriction.10
Airway irritation with increased salivary, laryngeal, and bronchial secretions (caused by an increase in mucus production and a decrease in mucociliary flow rates) varies among agents, with sevoflurane and halothane being essentially nonirritant and isoflurane and desflurane being potential irritants. This stimulation of airway receptors also appears to be responsible for the tachycardia and hypertension observed when desflurane is administered in high concentrations. The depressed mucociliary function seen with volatile agents is likely to contribute to impaired clearance of secretions and potentially to postoperative respiratory complications. The concomitant use of IV opioids lessens the irritant effect of inhaled volatile agents such as desflurane.11
IV Drugs with an Indirect Effect on the Airway
A Sedatives and Upper Airway Patency
The effect of general anesthetic agents on the upper airway is crucial to the practice of safe airway management, largely in terms of airway patency but also in terms of airway reactivity and airway protection against aspiration. There is a decrease in muscle tone associated with the loss of wakefulness, and this is compounded by specific drug-induced inhibition of upper airway neural and muscle activity and suppression of protective arousal responses. These processes tend to narrow the airway lumen, leading to airway obstruction. The mechanism of the reduction in muscle electrical activity relates, in part, to depressed hypoglossal nerve activity that occurs in excess of a similar depressant effect on other respiratory muscles, such as the diaphragm or intercostal muscles, which are more resistant to this dose-dependent loss of muscle tone.12 This reduction in hypoglossal nerve activity results in reduced tone in the muscles of the tongue and soft palate.
The differential suppression of respiratory muscles seems to vary among sedative agents, being less pronounced, for example, with ketamine than with other agents.13 Ketamine also has an indirect effect on the lower airways, causing bronchodilation by inducing the release of endogenous catecholamines. However, the loss of muscle tone caused by sedatives may not only relate to a specific effect of motor nerves. The depressed state of arousal results in a reduction of inputs from the reticular activating system to these motor nerves. This theory is borne out by changes in upper airway patency demonstrated during natural sleep, which show similarities to those induced by sedative drugs.
Originally, the upper airway narrowing associated with anesthesia was attributed to a posterior shift of the base of the tongue. Evidence now suggests that the soft palate and, to a lesser extent, the epiglottis are more relevant (Fig. 6-3). One study using lateral radiography demonstrated that occlusion of the airway under general anesthesia occurred most consistently at the level of the soft palate and sometimes at the level of the epiglottis, but in no patient did the tongue base come into contact with the posterior pharyngeal wall.14
Despite the assumption that loss of upper airway patency relates to a reduction in tone of the surrounding muscles, a consistent relationship between electromyographic activity and upper airway resistance has not been demonstrated. Thiopental causes measurable changes in muscular activity, but the changes are inconsistent and do not correlate with the onset of airway obstruction.15 Similarly, benzodiazepines increase upper airway resistance but again do not appear to have a consistent effect on genioglossus activity.16 Therefore, airway obstruction under general anesthesia may not relate to a simple diminution of muscular activity but to a disruption of the normal coordination of muscle activity that provides overall control of upper airway function.
The phase of the respiratory cycle is also relevant to the patency of the upper airway during spontaneous ventilation under general anesthesia. In a study by Nandi and colleagues, the movement of the soft palate during expiration was similar to that during apnea. However, during attempted inspiration, there was a significant reduction in the airway lumen at all levels, with the tongue now reaching the posterior pharyngeal wall in some cases and thus contributing further to the airway obstruction.14 This has relevance when one considers upper airway patency during anesthesia with or without muscle paralysis. The dynamic collapse of the upper airway that occurs during spontaneous inspiration anesthesia may be insignificant when pharmacologic paralysis is achieved. Similarly, the application of continuous positive airway pressure (CPAP) may also reduce this effect and help to maintain gas flow.
In summary, the increased collapsibility associated with anesthesia and sedation seems to be universal, regardless of whether the route of administration is inhalational or parenteral. Although this collapsibility lessens with decreasing anesthetic depth, the two do not necessarily have a linear relationship.17,18 The extent of the upper airway narrowing may vary subtly among agents, but the only clinically relevant difference appears to be the described lesser effect with ketamine.
At a laryngeal level, the effect of general anesthesia is probably different. One study demonstrated that the width of the laryngeal vestibule increased after administration of thiopental and succinylcholine.19
B Effect of Sedatives on Airway Reactivity and Airway Protection
Airway reflexes such as coughing, the expiration reflex, breath-holding, and laryngospasm are important in protecting the airway against contamination. These airway reflexes are usually obtunded by general anesthesia, although the exact relationship between specific agents and this suppression of activity has not been fully explored. Propofol, for example, has been shown to depress these reflexes,20 but vigorous airway reflexes have been demonstrated under baseline propofol anesthesia, suggesting that the depression with propofol as a lone agent is relatively limited in moderate doses. Combination with fentanyl, however, appears to have a significant influence on lessening airway reflexes.21
D Sedatives and the Lower Airway
All sedative agents that reduce muscular tone are likely to contribute to a reduction in a patient’s functional residual capacity (FRC) and an increased work of breathing. Benzodiazepines appear not to have a significant effect on lower airway patency, despite causing an apparent relaxation of tracheal smooth muscle and potentially attenuating reflex bronchoconstriction. The effect of IV anesthetic agents on bronchial smooth muscle is also unlikely to be of clinical significance. In vitro data suggest that propofol has a direct relaxant action.22 However, case reports and studies of IV induction agents used in asthmatics suggest that ketamine is the only agent with a significant bronchodilatory action. In contrast, volatile agents are fairly potent bronchodilators and have been used in the treatment of status asthmaticus.23,24
E Opioid Analgesics and the Airway
When fentanyl is combined with propofol, the depressant effect on upper airway reflexes is considerably more profound than with propofol alone, with the cough reflex being the most suppressed reflex and laryngospasm being the most resistant.21 The central mechanisms for this depression of reflexes are unclear and are probably complex.
Muscle rigidity associated with opioid use has been described25; although rare, it may be the direct cause of a significant increase in lower airway resistance that can make ventilation extremely difficult. Others suggest that this rare phenomenon in fact has more to do with vocal cord closure than with decreased pulmonary compliance secondary to chest wall rigidity.26 If the increase in airway resistance is truly linked to muscle rigidity, then its clinical manifestation is unpredictable and relates to many factors, including the opioid drug, its dose, its speed of administration, the effects of concomitant sedatives and muscle relaxants, and the age of the patient.
Short-acting narcotics are used at times in place of NMB agents, in combination with sedatives, to facilitate endotracheal intubation. However, upper airway conditions for airway instrumentation may be inferior, and the risks of arterial hypotension and laryngeal trauma may be higher.27
Remifentanil merits specific discussion because it is a relatively new drug in anesthesia and its use in facilitating safe and effective airway management is increasing. It is a potent, ultrashort-acting synthetic opioid that is administered typically by continuous infusion because it is immediately metabolized in the plasma. It causes profound respiratory depression and therefore is used clinically to successfully prevent spontaneous respiratory effort when assisted ventilation is the chosen mode of gas exchange. It also reduces muscle tone considerably and can be used to facilitate endotracheal intubation in the absence of NMB drugs.28 Use of remifentanil to facilitate smooth extubation is well described, and for some anesthesiologists,29 this technique has replaced deep general anesthesia extubation. Continuing remifentanil while discontinuing sedation results in a predominant effect of suppression of upper airway reflexes, in excess of any sedative effect. This allows extubation with good endotracheal tube (ETT) tolerance and a minimum of coughing. However, care is required when using the drug because of its potency. Apnea is likely and can even occur in a patient who is receiving remifentanil alone for conscious sedation.30 As with other synthetic opioids, muscle rigidity is described but not common.31
The main effect of opioids on the lower airway is similar to that described earlier, namely reduced airway reactivity and attenuated reflex bronchoconstriction. Mechanisms of action are again a combination of a neural effect and a direct dose-dependent effect in relaxing airway smooth muscle. For example, there is evidence that morphine attenuates vagally mediated bronchoconstriction in asthmatics.32 Opioid administration has been shown to cause histamine release, and there is also evidence that they cause an increase in tracheal smooth muscle tone, but neither effect has been associated with clinically demonstrable bronchoconstriction. A condition termed wooden chest syndrome has been described after administration of IV opioids, particularly if given at high dose; in this syndrome, thoracic and abdominal muscle rigidity apparently results in difficulty with assisted ventilation. The clinical significance of this finding is uncertain, but it has not restricted the use of these drugs worldwide.
F Neuromuscular Blockade and the Airway
NMB agents have several properties that may affect airway function. They are used in clinical practice to facilitate endotracheal intubation by abolishing airway reflexes and to facilitate mechanical ventilation by eliminating spontaneous respiratory effort. Similar to the effects of sedative agents on the respiratory muscles, these drugs also demonstrate a differential effect, with the diaphragm and the adductor muscles of the larynx being more resistant to paralysis than some of the muscles affecting upper airway patency.33 This relative sparing of the diaphragm permits the maintenance of respiratory effort even during complete paralysis of peripheral muscles. However, it also means that upper airway patency may be compromised at levels of paralysis that otherwise permit maintenance of normal spontaneous ventilation. Clinically, this is most relevant at extubation. A patient with residual NMB drug may maintain adequate ventilation with an artificial airway, such as an ETT or a supralaryngeal airway (SLA), in situ. After removal of the device, airway obstruction leading to hypoxemia may develop.
Removal of protective airway reflexes can have negative consequences if there is a risk of aspiration. Similarly, elimination of spontaneous respiratory effort may be deleterious if assisted ventilation cannot be delivered. Hence, care and experience are required for the safe use of NMB agents, and in certain clinical scenarios, it may be prudent to withhold them. However, the major clinical debate regarding their use seems to relate to their effect on upper airway patency. There is evidence that paralysis of the upper airway musculature improves upper airway patency. A recent study published data indicating that NMB using rocuronium facilitated bag-mask ventilation in anesthetized patients (Fig. 6-4).34
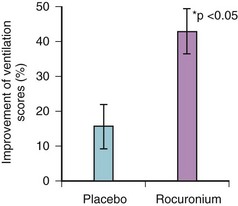
Figure 6-4 Efficacy of facemask ventilation in anesthetized patients with or without neuromuscular blockade.
(From: Szabo TA, Spinale FG, et al: Neuromuscular blockade facilitates mask ventilation. Anesthesiology 109:A184, 2008.)
Another study on the physiologic comparison of spontaneous ventilation and positive-pressure ventilation (PPV) in laryngotracheal stenosis concluded that spontaneous ventilation creates a negative inspiratory extrathoracic intratracheal pressure that causes indrawing of the mobile tracheal segments, further narrowing the airway.35 During expiration, there is positive intratracheal pressure, and a similar reduction in airflow does not occur. During PPV with muscle paralysis, however, a positive intraluminal pressure is created during inspiration that improves ventilation. Whether the conclusions of this paper can be extrapolated to the management of the upper airway under general anesthesia per se is uncertain, but several leading airway experts feel strongly that they should. The argument states that muscle relaxation makes upper airway management easier (and therefore safer) in terms of ventilation through a facemask or SLA and in terms of airway instrumentation, including intubation.36,37
Historically, there has been a fear that the prolonged effect of muscle paralysis during failing airway management under anesthesia contributes to severe hypoxic damage, but there does not appear to be any convincing evidence to support this supposition. The fear appears to relate to the loss of reversibility of the anesthetic technique, although it can never be certain whether the awakening of a patient during failing airway management is feasible before catastrophic desaturation occurs. The evidence suggests that, when faced with impossible bag-mask ventilation, very few anesthesiologists choose to discontinue the general anesthesia or avoid NMB.38 Most choose to provide oxygenation by intubating the trachea or by ventilating through an SLA device or performing an emergency cricothyrotomy. If ventilation is possible but intubation has been unsuccessful, “wake up” is strongly advocated by discontinuing any sedative drugs while reestablishing muscular tone and respiratory drive and maintaining oxygenation.
Impaired neuromuscular transmission secondary to partial pharmacologic blockade, even to a degree insufficient to evoke respiratory symptoms, markedly impairs upper airway dimensions and function. This may be explained by an impairment of the balance between upper airway dilating forces and the negative intraluminal pressure generated during inspiration. The same effect does not appear to occur during expiration.39 Furthermore, reflex glottic activity may be preserved, with a tendency toward coughing and laryngospasm, and it may also have a negative effect on gas flow. Complete muscular paralysis necessitating assisted PPV appears to have the reverse effect and increases upper airway patency.
Monitoring of the degree of NMB during anesthesia involving muscle relaxants is indicated, but there are limitations with the available techniques. The degree of blockade is frequently monitored by the response of the adductor pollicis to stimulation of the ulnar nerve, although this muscle is more sensitive than the diaphragm to paralysis.33 At present, monitoring methods that would reliably demonstrate the return of power required to maintain and protect the airway with an effective cough are lacking, and anesthesiologists tend to use a combination of monitoring and clinical assessment.
Reversal of nondepolarizing NMB before extubation and discontinuation of assisted ventilation is standard anesthetic practice. Use of a cholinesterase inhibitor, such as neostigmine, to flood the neuromuscular junction with acetylcholine and thereby restore neuromuscular function has traditionally been the only technique available for reversing the paralysis. These drugs could theoretically cause bronchospasm, but they appear to have no significant effect on airway resistance when combined with an anticholinergic drug such as atropine or glycopyrrolate. More importantly, inadequate reversal of the block, which is probably much more common than most anesthesiologists appreciate, can result in respiratory compromise, morbidity, and mortality.40 A meta-analysis of current reports of NMB in anesthesia revealed a 41.3% incidence of residual paralysis.41
G Other Drugs with Indirect Effect on the Upper Airway
IV lidocaine affects airway tone and reactivity, tending to relax smooth muscle and attenuate reflex bronchoconstriction such as that caused by intubation in asthmatics.42 However, the effect is unpredictable, and reports of IV lidocaine’s actually causing bronchoconstriction have been published.43 Historically, IV lidocaine has been used to improve intubation and extubation conditions by reducing upper airway reactivity.
V Airway Pharmacology for the Treatment of Asthma
Asthma (from the Greek, asthma, “panting”), as defined by the Global Initiative for Asthma (GINA),44 is a “chronic inflammatory disorder of the airways in which many cellular elements play a role. The chronic inflammation is associated with airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread, but variable, airflow obstruction within the lung that is often reversible either spontaneously or with treatment.”
A Overview
The complex, recursive interplay of inflammation, hyperresponsiveness, and airflow limitation determines the disease course, which over time produces structural airway changes, termed remodeling. There is presently greater recognition of the essentially inflammatory nature to asthma, with treatment directed at reducing this component over the long term as well as providing treatment to alleviate symptoms.45 An idea of the interplay of these factors is shown in Figure 6-5.
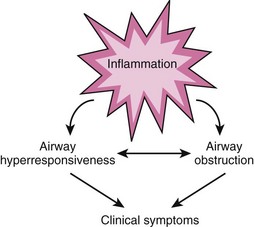
Figure 6-5 Interplay of airway inflammation, hyperresponsiveness, and obstruction.
(Adapted from National Asthma Education and Prevention Program: Expert Panel Report III: Guidelines for the diagnosis and management of asthma. Summary report 2007. J Allergy Clin Immunol 120[Suppl 5]:S94–S138, 2007.)
1 Diagnosis
Asthma is a clinical diagnosis, based on the symptoms and signs. Symptoms are variable, with one or more of the following being present: wheeze, breathlessness, cough, and chest tightness.46,47 None of these symptoms is specific to asthma. For example, wheeze is a function of any airway narrowing as a consequence of reduction of FRC. Signs of asthma include clinical verification by auscultation, spirometry, and lung function testing, which may include gas transfer measurements.48
There are no standard definitions for types of symptoms, nor for frequency or severity.47
2 Prevalence
Worldwide, asthma is estimated to affect more than 300 million people, 7% to 10% of the global population.49 About 15 million daily adjusted life-years (DALYs) are lost each year, which places asthma 20th in the current disability ranking, similar to schizophrenia and diabetes. There are about 225,000 asthma deaths each year, amounting to 1 in 250 deaths from all causes.50 In the United States, 7.3% of the population is diagnosed with asthma, and asthma accounted for 17 million physician consultations in 2006.51 The worldwide prevalence of asthma is predicted to increase by another 100 million by 2025.46
3 Distribution
There are marked differences in national and geographic distribution. Although methodologic factors may confound accurate measurement, there is widespread agreement that asthma is a disease of industrialized nations.46 Indoor aeroallergens, especially house dust mite52; tobacco smoking53; and obesity are some implicated factors.54,55
Genetic factors may contribute. Inheritance of an “asthmatic genotype” is complex with variable transmission.56 Atopy, the development of immunoglobulin E (IgE) antibodies to specific allergens, is the strongest identifiable risk for developing asthma.46,57,58 A family history of asthma, particularly on the maternal side, is a strong risk factor.59 Other inheritable traits are the forced expiratory volume in 1 second (FEV1) and response to drug therapies.56
Additionally, there are gender differences, with a higher incidence of asthma in prepubertal boys compared to girls.60 In middle age, however, there is a higher incidence among women.
4 Pathology
The pathology of asthma is incompletely understood and is an area of active research.61,62
a Airflow Limitation
Airflow limitation results from a combination of bronchoconstriction, inflammatory edema, and hypersecretion of mucus with airway plugging. Blood vessel hyperemia may also narrow small airways.63,64 These factors, either individually or collectively, narrow airways with impairment of respiratory gas exchange.
Mucus has a complex and variable structure. It is composed of long chains of mucin glycoproteins covalently cross-linked by disulphide bonds, polymerized DNA (from dead cells, particularly eosinophils), and polymerized (fibrous) F-actin together with a mixture of chemical mediators, modulators, and active, inactive, dead, or dying inflammatory cells65 (Fig. 6-6).
Green sputum is common but is not always indicative of infection, rather resulting from an abundance of eosinophils.66 When infection occurs, it is usually viral. Bacterial infection is uncommon.67 Most asthma exacerbations attributed to infection are from viruses,68 particularly rhinovirus.69
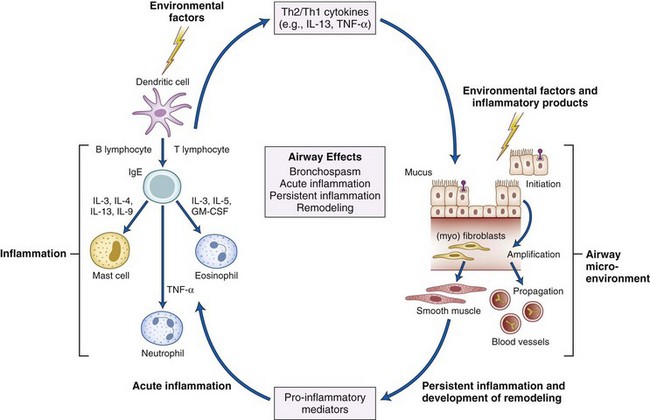
c Inflammation
One crucial aspect of asthma is considered to be the relative dominance of pro-inflammatory over anti-inflammatory factors driven by a variety of cell types in complex, dynamic, and variable ways. CD4+ lymphocytes, particularly the T helper type 2 (Th2) subtype, are presently thought to have a key role, with a predominance of this population over the T helper 1 (Th1) group. Relative overactivity of the Th2 group, especially at crucial developmental (childhood) stages, with expression of inflammatory cytokines such as interleukin-4 (IL-4), IL-5, IL-9, and IL-13, is considered to play a pivotal role.70
The inflammatory cytokines recruit and activate mast cells and eosinophils, leading to cellular infiltration, the density of which is often linked to disease severity.71 Some interleukins (IL-4 and IL-13) promote B-lymphocyte production of IgE in response to inhalation of allergens (aeroallergens). IgE binds to mast cell surface receptors, conferring immunologic memory and triggering release of mast cell contents (degranulation) when exposed to the specific aeroallergen.
A variety of substances such as histamine, proteases (including mast cell tryptase, a time-sensitive marker of degranulation), and cysteinyl-leukotrienes are released.72 At least 100 mediators have been described.73 Other stimuli, such as mechanical changes around these cells, may account for mast cell degranulation in response to cold-induced and exercise-induced asthma.74
Other cells, such as natural killer cells,75 Th17 cells,76 regulatory T cells,77 dendritic cells,78,79 macrophages,80 mast cells,81 and neutrophils, may be involved.82 Neutrophil activity is associated with severe disease and sudden deterioration.83
d Remodeling
Poorly controlled asthma may be complicated by anatomic changes in airway structure, which are often correlated to worsening of the disease84 but may start before diagnosis.85 A variety of cells are implicated in causing smooth muscle hypertrophy and hyperplasia, subepithelial fibrosis, angiogenesis, and mucus gland hyperplasia—collectively called the epithelial-mesenchymal trophic unit.
Recent attention has focused on the role of pulmonary blood flow in asthmatics, which is higher at rest compared with control subjects and increases during episodes of asthma enough to interfere with airflow.86

Full access? Get Clinical Tree


 ) mismatch, with an increase in intrapulmonary shunt fraction.
) mismatch, with an increase in intrapulmonary shunt fraction.