Chapter 25 Airway management and acute upper-airway obstruction
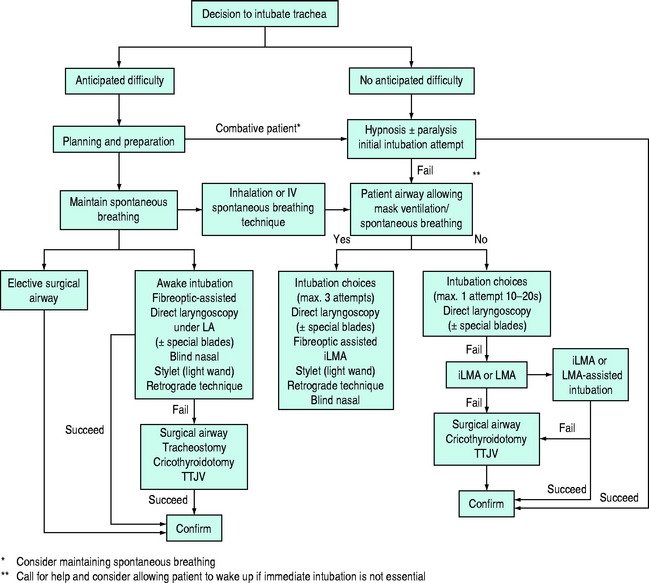
The primary objective of airway management is to secure unobstructed gas exchange and protect the lungs from soiling. Because of the critical importance of maintaining gas exchange, upper-airway obstruction is a life-threatening emergency. Upper-airway obstruction results from a wide range of pathophysiological processes, and therefore rapid assessment and establishment of a patent airway must take priority, even in the absence of a specific diagnosis. As no single airway management modality is universally applicable, the intensive care unit (ICU) physician must be capable of performing a variety of airway management techniques and instituting them in a logical and systematic way (Figure 25.1).
AIRWAY MANAGEMENT TECHNIQUES
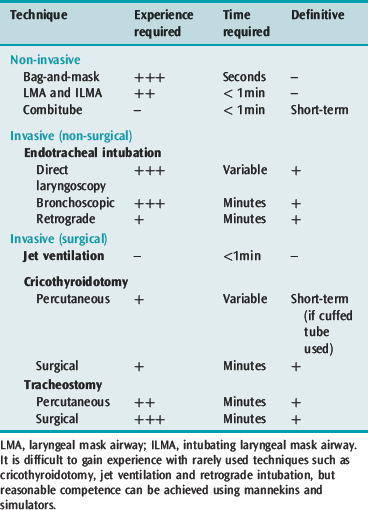
Airway management techniques are generally classified as non-invasive or invasive, depending on whether instrumentation occurs above or below the glottis, surgical or non-surgical, and definitive (Table 25.1). Definitive techniques secure the trachea and provide some protection from macroscopic aspiration and soiling. While bag-and-mask ventilation and direct laryngoscopic tracheal intubation remain the routine methods of airway management in ICU, the use of fibreoptic bronchoscopy is increasingly common, especially in special circumstances. Management of failed intubation and ventilation by various alternative techniques, particularly the use of the intubating laryngeal mask airway (iLMA) and cricothyroidotomy, is well described.1,2
The technique of choice will depend on each individual situation and is determined by the interaction of patient and clinical factors, which partially determine the appropriate technique (Table 25.2), and the clinician’s experience in applying the chosen technique. Other factors include availability of help, levels of training and supervision and accessibility of equipment. A portable storage unit with a wide choice of equipment appropriate for difficult airway management should be available in every ICU (Table 25.3).
Table 25.2 Commonly recommended applications of described airway management techniques. Examples of common alternatives are given in approximate order of choice
| Difficult direct laryngoscopic intubation | With difficult spontaneous/mask ventilation | |
|---|---|---|
| Awake | Fibreoptic bronchoscopic intubation Direct laryngoscopic intubation* Blind nasal intubation Retrograde intubation | Percutaneous cricothyroidotomy* Surgical tracheostomy* |
| Anaesthetised or comatose (empty stomach) | Bag-and-mask ventilation Direct laryngoscopic intubation Different blade Fibreoptic bronchoscopic intubation Intubating LMA/LMA Lighted stylet Blind nasal intubation | Laryngeal mask airway (LMA) Transtracheal jet ventilation Rigid ventilating bronchoscope Percutaneous cricothyroidotomy Surgical tracheostomy |
| (full stomach) | Maintain cricoid pressure with all techniques Intubating LMA/Proseal LMA Combitube | Percutaneous cricothyroidotomy Surgical tracheostomy Combitube |
The technique(s) chosen should also depend on the clinician’s knowledge and ability. Cricoid pressure should be applied with a force of approximately 30 N, but applied force can be temporarily reduced to assist airway manoeuvres.
Table 25.3 Suggested contents of a portable storage facility for difficult airway management
| Masks |
| Face and nasal masks of differing make and size variety |
| Airways |
| Oropharyngeal airways |
| Nasopharyngeal airways |
| Airway intubator guide for oral endoscopic intubation |
| Laryngeal mask airway (LMA) and intubating LMA with appropriate endotracheal tubes |
| Rigid laryngoscope with a variety of designs and sizes |
| Short handle or variable angle (Patil-Syracuse) laryngoscope |
| Curved blades: Macintosh, Bizarri-Guiffrida |
| Straight blades: Miller |
| Bent blade: Belscope |
| Articulating-tip blade: McCoy |
| Fibreoptic stylet laryngoscope or Bullard laryngoscope |
| Endotracheal tubes of assorted size |
| Murphy tubes |
| Microlaryngoscopy tubes |
| Endotracheal tube stylets |
| Gum elastic bougie (Eschmann stylet) |
| Malleable stylet |
| Tube changer, hollow tube changer (jet stylet) |
| Lighted stylet (light wand) |
| Fibreoptic intubation equipment |
| Patil endoscopic mask, oral airways or blocks to facilitate oral endoscopic intubation |
| Fibreoptic endoscopes with light source, adult and paediatric-sized |
| Combitube |
| Emergency surgical airway access |
| Percutaneous cricothyroidotomy set |
| Transtracheal jet ventilation – cannula and high-pressure O2 source connectors |
| Regulated central wall O2 pressure (Sanders-type injector) |
| Unregulated central wall O2 pressure device |
| Exhaled carbon dioxide monitor |
| Capnometer/capnograph |
| Chemical indicators |
NON-INVASIVE TECHNIQUES
BAG-MASK VENTILATION
Some considerations when performing mask ventilation include the following:
ORO- AND NASOPHARYNGEAL AIRWAYS
A nasopharyngeal airway is a soft rubber or plastic tube inserted into the nostril and advanced along the floor of the nose (in the direction of the occiput). Correctly positioned, the tube traverses the posterior pharynx. It is better tolerated by semiconscious patients than the oropharyngeal airway. Complications include epistaxis, aspiration and, rarely, laryngospasm or oesophageal placement.
LARYNGEAL MASK AIRWAY (LMA) AND INTUBATING LMA
The LMA is a reusable device that consists of a silicone rubber tube connected to a distal elliptical spoon-shaped mask with an inflatable rim, which is positioned blindly into the pharynx to form a low-pressure seal against the laryngeal inlet.3 LMAs are useful to achieve non-definitive airway patency in many emergency situations (see Figure 25.1), and can be used to provide positive-pressure ventilation.2 Once positioned the LMA has been used to guide the passage of stylets, bougies, the bronchoscope and an endotracheal tube into the trachea, but with difficulty.2,4 The iLMA or FasTrach is a modification of the LMA with several features to facilitate intubation once the iLMA is placed.5 There is a guiding ramp and epiglottic elevating bar at the aperture to direct the endotracheal tube to the glottis. It also has an anatomically curved, rigid shaft and handle to allow easy and firm manipulation during placement and when the endotracheal tube is passed.6 The iLMA is the laryngeal mask of choice if intubation is required, as is frequently the case in ICU patients.
Although preparation and patient positioning techniques for placement of a LMA and iLMA are similar, the insertion technique is quite different. The mask airway is prepared for insertion by deflating and smoothing out the cuffed rim to be wrinkle-free, and the posterior surface and patient hard palate are lubricated with water soluble jelly. The patient is positioned as for endotracheal intubation, with slight flexion of the neck and extension of the atlanto-occipital joint (sniffing-the-morning-air position). The LMA is inserted with the tip of the cuff continuously applied to the hard palate, and with the right index finger guiding the tube to the back of the tongue until a firm resistance is encountered. The cuff is then inflated with 20–40 ml of air (adult sizes) before attachment of the breathing circuit.
COMBITUBE (OESOPHAGEAL–TRACHEAL DOUBLE-LUMEN AIRWAY)
The oesophageal–tracheal Combitube is a double-lumen tube that is blindly inserted into the oropharynx up to the indicated markings.7 The oesophageal lumen is blocked at the distal end and has side perforations at the pharyngeal level whereas the tracheal lumen has a hole at the distal end. It has two balloon cuffs, a distal one and a proximal pharyngeal balloon. The patient is ventilated through the oesophageal lumen initially as the Combitube usually enters the oesophagus,7 with the distal cuff sealing the oesophagus and the proximal balloon sealing the proximal pharynx. Gas exits the perforations and enters the pharynx and larynx. In the event of failure of ventilation, tracheal intubation may have occurred and then the tracheal lumen is ventilated while the distal cuff seals the trachea. Although demonstrated to be a useful airway management adjunct, its role in resuscitation and management of the difficult airway in the ICU environment is yet to be established. Barotrauma, especially oesophageal rupture, has been reported.
INVASIVE TECHNIQUES
ENDOTRACHEAL INTUBATION
Endotracheal intubation remains the ‘gold standard’ of definitive airway management, allowing for spontaneous and positive-pressure ventilation, with good macroscopic protection from aspiration. Indications include acute airway obstruction, facilitation of tracheal suctioning, protection of the airway in those without protective reflexes, and respiratory failure requiring ventilatory support with high inspired concentrations of oxygen and PEEP.
Preparation
Prior to proceeding with any attempts at intubation, regardless of the technique chosen, preparation and checking of all relevant equipment are essential. Tracheal intubation should be preceded by adequate preoxygenation, particularly in ICU patients who frequently have pulmonary or cardiac pathology. Difficult airway management equipment (see Table 25.3) should also be accessible within a few minutes. Food, vomitus, blood or sputum may obstruct the airway and therefore suction, able to generate at least 300 mmHg (40 kPa) and a flow rate of 30 l/min, should always be available. Excessively vigorous suctioning should be avoided as it can cause laryngospasm, vagal stimulation, mucosal injury and bleeding.
Direct laryngoscopy
Although an essential skill for all intensivists, direct laryngoscopy and intubation is difficult to master.8 It can be learned by simulation, exposure to patients in a controlled environment such as the operating room and subsequently practised under supervision in the ICU setting. A detailed description of the technique is beyond the scope of this chapter; however certain problems and complications commonly encountered in ICU patients should be anticipated and prevented.
The route of intubation may be orotracheal or nasotracheal. The orotracheal route is preferred because it has fewer complications. Nasotracheal intubation is contraindicated in the presence of fracture of the base of skull. Other complications include epistaxis, turbinate cartilage and nasal septal damage, and in the long-term an increased risk of nosocomial pneumonia and sinusitis.9
Rigid indirect fibreoptic technique
The Bullard laryngoscope is a rigid, indirect fibreoptic instrument that is shaped to follow the hard palate. The learning curve appears reasonable and it has been shown to be a viable alternative for intubation in the difficult airway and reduces cervical spine movement during laryngoscopy compared with the Macintosh or Miller laryngoscope.10
Fibreoptic bronchoscopic technique
This technique offers advantages of direct visualisation, immediate diagnosis of upper-airway lesions and immobility of the neck during the procedure.11 It also allows reasonably comfortable intubation of a cooperative, awake patient under local anaesthesia, and use of the sitting position. Experience and skill are necessary, especially for dealing with emergent situations, but success rates > 96% are expected.12 Fibreoptic oral intubation may also be performed in anaesthetised patients, using a modified face mask with diaphragm. Nasal intubation is usually performed through an endotracheal tube placed in the nasopharynx, with the tip just above the glottis. The fibreoptic bronchoscope tip is guided into the trachea and the tube is advanced over the bronchoscope. Correct placement is visually checked before the scope is removed. In ICU the fibreoptic bronchoscope can be used to improve the safety of airway procedures such as endotracheal tube changes and percutaneous tracheostomy.13,14 A number of specially designed oral airways are available to assist oral fibreoptic intubation. The most common cause of failure is obstructed vision from blood or secretions.
Less commonly used techniques of endotracheal intubation
The retrograde intubation technique consists of the percutaneous introduction of a J-tip guidewire through the cricothyroid membrane, which is then advanced into the retropharynx. The tip is retrieved from the oral cavity, and the wire is used to guide an oral endotracheal tube past the obstruction and into the trachea.15 The procedure is a relatively simple and safe alternative if other techniques fail or are not possible. Commercial kits are available.
Confirmation of tracheal tube placement
Confirming correct intratracheal tube placement is essential. Direct visualisation and measurement of expired CO2 by capnography are the most reliable methods.16 Capnography may produce false-positive results with the first few breaths after oesophageal intubation (i.e. detectable end-tidal PCO2), if gastric insufflation from mask ventilation has occurred. A false-negative (decreased PCO2, despite correct position) may occur with cardiac arrest and low-cardiac-output states. Position can also be reliably confirmed by fibreoptic confirmation and the use of oesophageal detectors or self-inflating bulbs.1 Other clinical signs, such as auscultation of breath sounds over both sides of the chest and epigastrium, visualisation of condensed water vapour in the tube and chest wall movement, are less reliable.
TRANSTRACHEAL JET VENTILATION (TTJV)
Percutaneous TTJV, using a large-bore intravenous (IV) catheter inserted through the cricothyroid membrane, can be used to provide temporary ventilation when other techniques have failed.17 Ventilation through the cannula with a standard manual resuscitator bag is inadequate, and a jet ventilation system is necessary. A high-pressure (up to 50 psi or 344 kPa) oxygen source is required for adequate ventilation through a 14 FG IV cannula with a manually regulated jet injector. Expiratory gases must be able to escape via the glottis. Appropriate chest movements during expiration must be noted. The consequence of expiratory obstruction is severe and potentially fatal barotrauma.

Full access? Get Clinical Tree