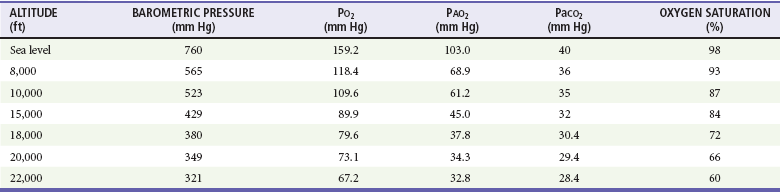
Chapter 191 The impact of AMT on the wounded soldier was clear. During World War II, the average time from injury to definitive care was 6 to 12 hours, with a mortality rate of 5.8%. In Korea, the time was 2 to 4 hours, with 2.4% mortality. In Vietnam, the time was 65 minutes, and mortality was less than 1%.1 Encouraged by the military experience, civilian AMT in the United States was propelled by the 1969 start of the first hospital-sponsored, fixed-wing air medical program. The first civilian helicopter emergency medical services (HEMS) program in the United States was established in 1972. A working knowledge of aviation physiology is vital to understanding of the effects of AMT on pilots, medical personnel, and patients.2 Physiologic difficulties from expansion and contraction of gases within the closed spaces of the body may occur with altitude change. Squeeze injuries from contraction of air and associated soft tissues within closed cavities occur on descent and are common causes of barotitis, barosinusitis, and toothache. Reverse squeeze injuries occur on ascent, as decreasing barometric pressure leads to an increased volume of the air trapped within the space, exerting pressure on structures. Ascent injuries can include conversion of a simple pneumothorax into a tension pneumothorax or rupture of a hollow viscus by expansion of intestinal gas. The operation of medical equipment containing closed air spaces, such as intravenous tubing and pumps, air splints, ventilators, and endotracheal tube and laryngeal airway cuffs, may also be affected by altitude.3–7 Dalton’s law states that the total barometric pressure at any given altitude equals the sum of the partial pressures of gases in the mixture (Pt = P1 + P2 + P3 … Pn). Whereas oxygen still constitutes 21% of the atmospheric pressure at altitude, Boyle’s law notes that each breath brings fewer oxygen molecules per breath to the lungs, and hypoxia results (Table 191-1). The clinical effect of Dalton’s law is manifested as a decrease in arterial oxygen tension with increasing altitude. Table 191-1 Effects of Altitude on Oxygenation PAO2, partial pressure of alveolar oxygen; PaCO2, partial pressure of arterial carbon dioxide. Air medical services may take several forms. Despite a tremendous growth of operations in the past 20 years, the most common type of HEMS program in the United States remains the hospital-sponsored operation transporting patients from outlying referral centers or accident scenes to tertiary care centers. A single hospital or a consortium of institutions may sponsor these flight programs. In 2011, there were more than 220 dedicated HEMS programs operating more than 750 dedicated aircraft throughout the nation.8 Approximately 54% of the programs were hospital sponsored, and the balance were operated by privately owned or publically traded companies. Whereas these for-profit companies represent 46% of the programs, they operate more than 61% of the dedicated helicopters in the United States.8 Public service agencies may also sponsor air medical services or partner with private companies; vehicles used by these programs are often multifunctional aircraft that serve in medical, search and rescue, fire suppression, and law enforcement roles. The Military Assistance to Safety and Traffic (MAST) program operated by the U.S. Armed Forces provides additional HEMS resources to the community,9 but in recent years their role for civilian support has been generally limited to Hawaii and Alaska.9 Together, the public service and MAST helicopters add more than 120 additional aircraft available for patient transport.8 There is no accurate accounting of the number of fixed-wing air ambulance companies or airplanes. Although some hospitals do sponsor fixed-wing AMT, it is more common for these programs to be private fee-for-service operations. Disadvantages to HEMS include noise, vibration, thermal variances, and other stressors on patients and crew exaggerated by rotor-wing flight. Weather considerations may significantly limit the availability of helicopter transport. In smaller aircraft, cramped spaces and weight limitations may limit the number of patients, transport personnel, or equipment that can be carried. This may sometimes compromise optimal patient care (Fig. 191-1). Air medical crew members represent the broad spectrum of health care providers. AMT services that provide critical care transport, advanced life support, or specialty care transport must staff the vehicle with a minimum of two medical personnel to provide direct patient care.10,11 The majority of AMT programs in the United States provide critical care transport teams composed of one registered nurse and an additional crew member (paramedic, respiratory therapist, physician, or a second nurse); most common is the nurse-paramedic crew.12 AMT crew configuration may also be mission dependent. A service may at times believe that it is appropriate to use a single medical crew member. For example, it may be appropriate while transporting a stable patient on a routine interfacility transport. Certain flight conditions and situations may also necessitate flying with a single crew member, including heat, humidity, altitude, distance, fuel on board, and weight of the patient.12 The AMT environment imposes unique considerations on the air medical flight crew that can influence their ability to provide patient care. Human factors work has shown that most medical care procedures are more difficult to perform in an AMT vehicle than in other ground-based settings.13 Auscultation of the heart and lungs, palpation of pulses, performance of cardiopulmonary resuscitation, endotracheal intubation, radio communications while using a respirator or face mask, and recognition of visual alarms may all be impaired while aloft.14–19 In addition, fatigue, motion sickness, exposure to engine exhausts, an erratic pattern of work activity, and the high risk involved in AMT operations may affect task performance significantly.20–22 Seizures from photic stimuli associated with rotor motion (“flicker illness”) has also been reported.23 High-fidelity simulation of air medical missions can acquaint flight crew to the novel environment, but fiscal and personnel costs may be prohibitive.24 All air medical services require the active involvement of a physician as medical director responsible for supervising, evaluating, and ensuring the quality of medical care provided by the AMT team.25 Emergency physicians play a significant role, with nearly 50% of all air medical directors having a background in emergency medicine.26 The medical director must have the final authority over all clinical aspects of the air medical service and should ensure that the flight crew have adequate training and qualifications to optimize patient care. Medical care policies and procedures should be established, including specific provisions for on-line and off-line medical control. The Air Medical Physician Association and the National Association of EMS Physicians have established guidelines for the medical director of an air medical service.27,28 Safety is the predominant concern of air medical operations, and ensuring safe flight is a fundamental part of every flight program.29 Safety must also be an overriding consideration in weighing the risks and benefits of AMT. The role of aircraft pilots and mechanics is essential to the airworthiness of the vehicle, and medical personnel must also be proficient in both routine and emergency operations in and around the aircraft. Checklists may aid in safety practices but alone may not detect significant operational concerns.30 Crew fatigue and other self-imposed stresses that could affect safety, such as the use of prescription or over-the-counter medications, tobacco, and alcohol, must be scrupulously avoided. The practice of “helicopter shopping” has been a major factor in a number of fatal HEMS events. Helicopter shopping refers to the practice of a requesting EMS agency or hospital calling numerous HEMS operators until one agrees to accept a flight without disclosure to the accepting HEMS operator that other programs have declined the flight because of bad weather or other safety concerns.31,32 The practice has been so common that in 2006, the Federal Aviation Administration issued a letter to all state EMS directors describing helicopter shopping and requesting that they take action to prohibit this practice.33 Many hospitals have designated landing areas that are appropriately lit and secured (Fig. 191-2), with fixed coordinates and predesignated liftoff and approach patterns. However, most primary (scene) responses occur at unmarked sites. Ground personnel must be trained to designate and secure a safe landing zone for helicopter operations. AMT programs have an obligation to help train ground staff on proper landing zone setup and conduct (Boxes 191-1 and 191-2).
Air Medical Transport
Perspective
Aviation Physiology
Boyle’s Law
Dalton’s Law
Principles of Air Medical Transport Systems
Air Medical Aircraft
Helicopters (Rotor-Wing Aircraft)
Air Medical Flight Crew
Medical Direction
Safety
Landing Zones
Air Medical Transport







