HPV-negative tumors
HPV-positive tumors
Decreasing incidence
Increasing incidence
Tobacco abuse common
Tobacco abuse less common
Alcohol abuse common
Alcohol abuse less common
Low oral sex exposure
High oral sex exposure
Marajuana use less common
Marajuana use more common
More advanced age
Less advanced age
Lower socioeconomic status
Higher socioeconomic status
All head and neck subsites
Predominantly oropharynx subsite
Relatively poor locoregional control
Excellent locoregional control
Poor disease-free and overall survival
Good disease-free and overall survival
Comorbid disease common
Comorbid disease less common
Improved technical precision, access, and visualization with minimally invasive surgical approaches have allowed for a reemergence of primary surgical therapy for many head and neck tumors, including that of OPSCC. Minimally invasive surgery of the head and neck consists of techniques that reduce the extent of surgery through the use of natural orifices, small incisions, and tools that enhance visualization. The proposed benefits of these approaches are to maintain or improve oncologic outcomes, reduce operative morbidity, improve patient function and quality of life, and decrease hospital stay and overall cost of care.
While these techniques have long been used for accessible oral cavity tumors, transoral surgery (TOS) has increasingly been utilized as a primary treatment modality for both early and late-stage OPSCC as well. The two most popular and proven techniques, transoral laser microsurgery (TLM) and transoral robotic surgery (TORS), are also sometimes utilized to treat oral cavity and laryngeal tumors of the head and neck (Table 18.2). There has been growing interest in these minimally invasive TOS techniques that avoid the morbidity associated with traditional open en bloc resections, which often included a mandibulotomy and extensive dissection of non-cancerous, normal tissues to gain access to the tumor.
Table 18.2
Differences between TLM and TORS for minimally invasive approaches to SCCHN
TLM | TORS | |
|---|---|---|
Advantages | Precise tissue differentiation with laser use | No line of sight limitations |
High resolution binocular visualization of tumor | High resolution 3D visualization of tumor | |
Relative ease in addressing larynx and hypopharynx tumors | Tremor-filtration and motion scaling | |
Tactile feedback | Instrument range of motion | |
Disadvantages | Laser safety considerations/risks | Cost of robotic system use |
Relative steep learning curve | Lack of tactile feedback | |
Line of site limitations | Credentialing and training requirements | |
Requirement for skilled pathologist to accurately assess piecemeal resection margins | Access: need to share with other services | |
Need for skilled surgical assistant at head of bed |
With the TLM technique, a modified mouth gag and/or expandable distending bivalved laryngoscope is used to expose the primary tumor (Figs. 18.1 and 18.2). As tumors extend more proximally into the upper aerodigestive tract, this process becomes more challenging, with tumors of the base of tongue (BOT) and vallecula requiring precise placement of these instruments for adequate tumor exposure and resection. A rigid telescope, or more commonly, high-magnification operating microscope, is then used to magnify and illuminate the exposed operative field (Figs. 18.3 and 18.4). This improved visualization of the tumor then provides the surgeon the ability to utilize either the line-of-site carbon dioxide (CO2) laser or handheld CO2 laser fiber for tumor resection. With the TLM technique, tumors are usually transected through the mid-portion to gain valuable and accurate information on depth of invasion and of the critical neurovascular structures adjacent to these tissues. Tumors are excised segmentally and ultimately removed piecemeal, mapping margins and paying close attention to both the peripheral and deep extension of the tumor as the procedure proceeds. This utilization of trans-tumoral cuts goes against the classic dogma within the surgical world of en bloc resection. However, long-term follow-up data from both Europe and the USA has shown that this method of tumor extirpation does not negatively impact local control.



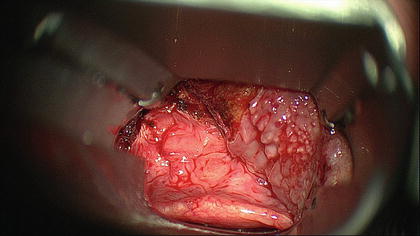

Fig. 18.1
In TLM, surgical exposure of the tumor within the upper aerodigestive tract is achieved with use of various oropharyngeal retractors, pharyngoscopes, and laryngoscopes

Fig. 18.2
Handpieces designed to transmit a flexible laser fiber can be then passed through the device used for surgical exposure. Pictured here is a bivalved expandable pharyngoscope with a laser handpiece

Fig. 18.3
Surgical exposure of the base of tongue tumor is obtained with use of a bivalved expandable pharyngoscope and patient is placed in suspension. Use of a rigid telescope or microscope allows for high magnification view of the tumor
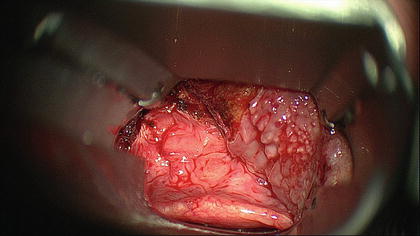
Fig. 18.4
High magnification view of right base of tongue tumor resection bed through a bivalved expandable pharyngoscope. Epiglottis is noted posteriorly with residual base of tongue tissue noted superiorly and laterally on the right. Evidence of tumor resection seen laterally on the left and superiorly
With the high-magnification operative view that the microscope provides, along with the distinct tissue characteristics that are seen when the laser cuts through cancerous and normal tissues, margin control has been shown to be excellent with this technique. A reasonable margin of normal-appearing tissue (usually 1 cm) is then excised beyond the invading front of the tumor. The resected tissues are then inked in the operating room by the surgeon, as the three-dimensional complexity of the tissues removed can lead to processing issues if precise orientation is not maintained. Intraoperative frozen section margins can be assessed from the tissues removed and/or additional margins can be sent for analysis as well.
The role of TLM has been expanding since the early 1980s, when Wolfgang Steiner in Goettingen, Germany described line-of-site laser ablation of upper aerodigestive tract tumors. The excellent oncologic and functional results from the TLM approach in Europe were reinforced in the USA with multi-institutional data showing excellent outcomes with primary TLM resections of advanced stage oropharyngeal malignancies [3, 4]. With TLM, oncologically sound tumor ablation can be accomplished with minimal collateral damage to adjacent soft tissues and neurovascular structures. This has ultimately led to excellent locoregional tumor control rates, with improved recovery of swallowing function, low rates of tracheotomy dependence, and decreased length of hospital stay [4]. TLM has been widely accepted for treatment of early-stage T1 and T2 tumors of the upper aerodigestive tract, and there is evidence to support its effectiveness for select advanced-stage T3 and T4 lesions of the oral cavity, larynx, and oropharynx as well.
TLM for BOT tumors can be quite challenging, however, and the technique requires specific training, patience, and experience to successfully gain access and remove many of these tumors. More recently, TORS has rapidly gained recognition as an effective minimally invasive modality for the surgical resection of upper aerodigestive tract cancers, with particular benefits in the treatment of BOT tumors. In 2009, the US Food and Drug Administration (FDA) approved the da Vinci® Surgical System (Intuitive Surgical, Inc, Sunnyvale, CA) for transoral surgical procedures restricted to early stage malignant and benign lesions.
The da Vinci® Surgical System was not the first robotic system developed for the use in the operative theater. While both the military and the National Aeronautics and Space Administration (NASA) were interested in developing a surgical robotic system, the first surgical application was in 1985 when the PUMA 560 performed a needle-guided biopsy of a brain tumor with CT guidance. In 1993, the FDA approved the first robotic system, known as Automated Endoscopic System for Optimal Positioning (AESOP), to assist with laparoscopic surgery, providing a robotic-controlled arm to “drive” the endoscope during these procedures. The FDA then approved the Da Vinci robotic system in 2000 for laparoscopic surgery, culminating in its eventual approval for head and neck surgery in 2009. Leading up to this approval, the safety and feasibility of TORS using the da Vinci® robotic system was reported in both preclinical and clinical work, mainly from the University of Pennsylvania [5, 6].
The surgical robotic system consists of a surgeon console, the surgical robotic device with associated specialized instrumentation, and a monitoring system for the remainder of the surgical team to view (Figs. 18.5 and 18.6). The main operative surgeon sits remotely from the patient at the surgeon console, while the surgical assistant sits at the head of the patient’s bed. The console provides the surgeon with three-dimensional (3D) images of spectacular high-definition quality, which is obtained through the use of either straight or angled endoscopes placed transorally. From this console, this endoscope is controlled, along with two transorally positioned robotic arms. The robotic arms hold a variety of specialized, wristed instruments with tremor filtration and seven degrees of freedom. This articulating freedom of motion within tight spaces, along with the visualization “around corners,” is what sets TORS apart from any other surgical approach to the BOT. The operative assistant typically utilizes a suction in hand to function as a retractor and suction the surgical smoke. The assistance role is critical for providing hemostasis as well with the use of surgical clips that must be exchanged with the suction as needed. Therefore, four instruments and an endoscope are transorally operating through the mouth of the patient at any given time. The CO2 laser fibers can be utilized with TORS as well, but more commonly, a Bovie cautery robotic handpiece is utilizes for resection of the tumor. Resection is usually performed en bloc with an appropriate margin of normal surrounding tissues. Intraoperative frozen section margins are then sent to ensure oncologically sound resections.



Fig. 18.5
Surgical assistant seated at the head of the patient during Transoral Robotic Surgery (TORS) while viewing primary surgeon’s view on monitor

Fig. 18.6
Two robotic arms with midline robotic endoscope placed through the mouth to gain access to the oropharynx for Transoral Robotic Surgery (TOS)
Regardless of technique utilized, TOS for the oropharynx, as well as for other subsites within the head and neck, has been thoroughly studied and oncologic results are comparable to nonsurgical modalities of therapy. Compared to open resections, TOS provides improved functional outcomes for patients, including swallowing and speech outcomes. Gastrostomy and tracheostomy tube dependency rates are lower as well, allowing for improved quality of life. Hospital stays have been shown to be lower, leading to an overall decreased cost of treatment [7]. If negative margin resections are obtained on final pathology, depending on tumor biology and stage, adjuvant radiation therapy can sometime be avoided, or at the very least, its dose can be decreased. In advanced stage disease, a primary surgical approach may also allow for the ability to omit chemotherapy from the multi-modality treatment regimen, thus eliminating its associated side effects and accompanying cost.
Minimally Invasive Approaches to the Skull Base
Advances in transnasal endoscopic techniques have dramatically changed the way in which skull base tumors have been approached over the last two decades. These techniques, initially developed for the treatment of benign paranasal sinus disease, have matured to become known as expanded endonasal approaches (EEA) to the skull base (Figs. 18.7 and 18.8). Open craniofacial resection (CFR) approaches to the skull base have traditionally been used to resect tumors of the anterior and anterolateral skull base. However, these approaches, while providing excellent surgical exposure, require large facial and/or cranial incisions, entail dissection through extensive “normal” soft tissues of the face, head, and neck, and often require sacrifice of important neurovascular anatomy. While at times necessary, these complex and highly technical approaches have the potential of leaving patients with long-term functional and cosmetic deficits.
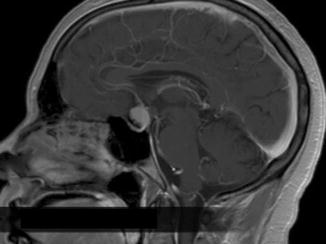

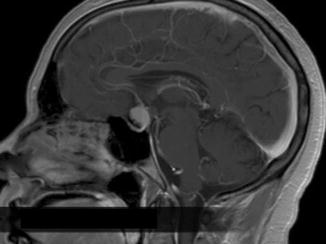
Fig. 18.7
Coronal MRI showing craniopharyngioma of the anterior skull base. (Used with permission of Dr. Adam Zanation)

Fig. 18.8



Intraoperative view of transnasal endoscopic resection of craniopharyngioma. Total resection was carried out without external incisions or craniotomy. (Used with permission of Dr. Adam Zanation)

Full access? Get Clinical Tree








