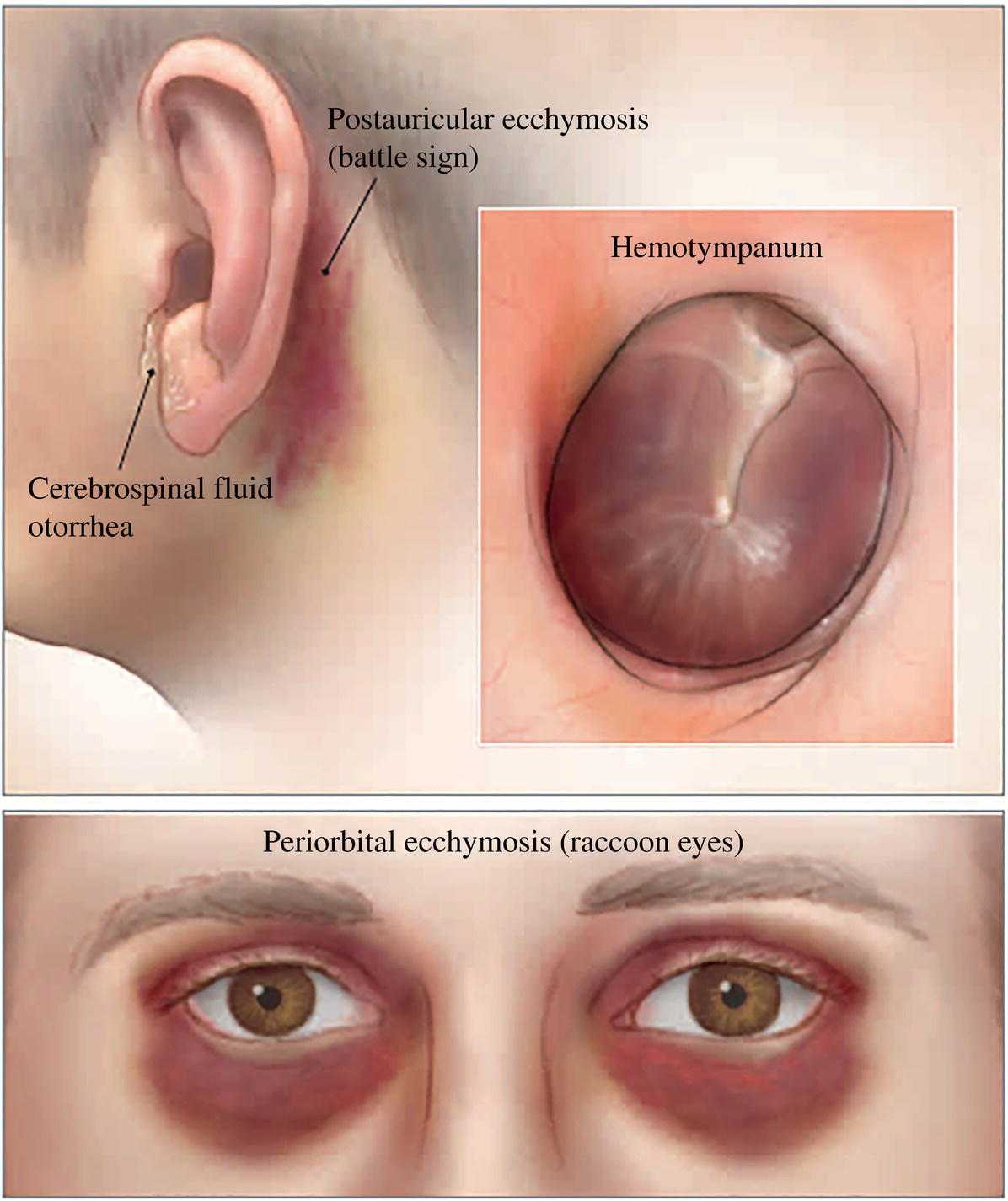
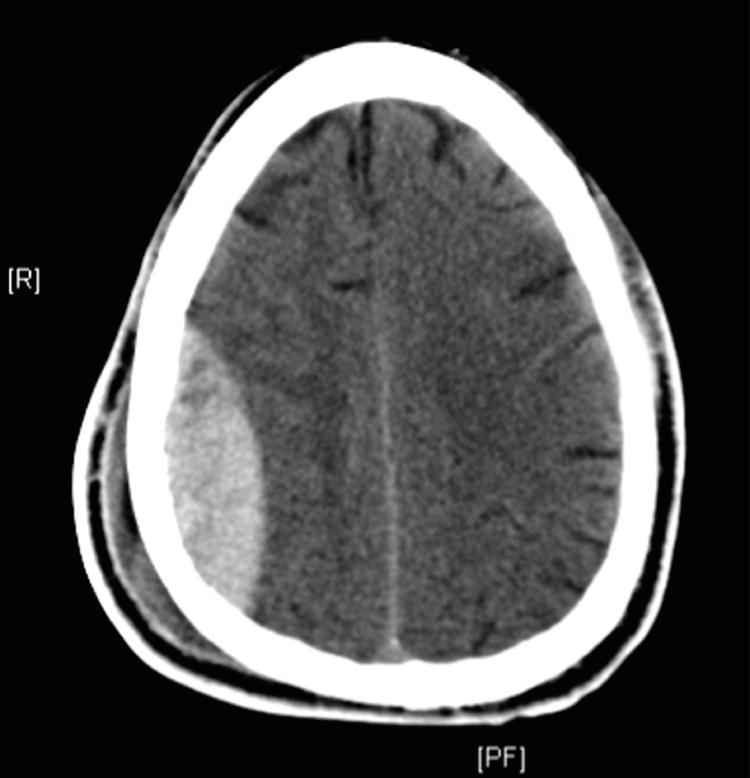
Ian T. Ferguson and Christopher R. Carpenter Department of Emergency Medicine, Washington University School of Medicine, St. Louis, MO, USA In 2013, 2.5 million traumatic brain injury (TBI)‐related emergency visits occurred in the United States with approximately 282,000 hospitalizations and 56,000 deaths.1Emergency department (ED) physicians must first recognize the possibility of TBI, which can be overlooked in multitrauma patients or in those who present remotely from their injury.2 For example, older adults who have fallen often fail to report the fall or related head trauma, yet approximately 5% of these patients will have intracranial bleeding.3 Patients with mild TBI, typically described as those having a Glasgow Coma Scale (GCS) score of 14–15 and a nonfocal neurological examination, comprise the majority of ED blunt head injury cases.4 Evaluation for operative or otherwise significant intracranial injuries using computed tomography (CT) increases radiation exposure, healthcare costs, and the risk of over‐diagnosis and over‐treatment.5 As discussed in Chapter 5, multiple stakeholders, including payers and guideline developers, increasingly promote appropriateness criteria to justify imaging decisions for common presentations such as blunt head injury.6,7 Adherence to appropriateness criteria varies widely between ED physicians with a skew toward over‐imaging.8 A number of clinical aids exist to standardize imaging decisions. In addition, TBI biomarker research is accelerating, although the practical application of these advances in ED settings is inconclusive. Can history, physical exam, and/or decision aids accurately and reliably identify adults with blunt head injury at low risk for intracranial injury? Based upon nine studies summarized in a 2015 meta‐analysis, history and physical exam have limited accuracy to identify the severe intracranial injury.9 In history, more than two episodes of post head injury vomiting most accurately increases the risk of severe intracranial injury, while the absence of any of these findings is inadequate to reduce the risk as summarized in Table 12.1. The most accurate physical exam finding to increase the risk of severe intracranial injury is the presence of a skull fracture as summarized in Table 12.2. Physical exam findings concerning for a skull fracture most accurately increase the risk of severe intracranial injury, but the absence of any of these findings does not significantly decrease the risk. Specific findings suggestive of a skull fracture include a bony depression on palpation. Basilar skull fractures are suggested by the presence of Battle sign, hemotympanum, cerebrospinal fluid otorrhea, or raccoon eyes (Figure 12.1). Three head injury decision aids exist. The New Orleans decision aid was the first one and is summarized in Table 12.3.10 In the original derivation/validation study, inclusion criteria included: ≥3 years old who had loss of consciousness or amnesia, a normal neurological examination, GCS of 15, and a presentation within 24 hours of injury. A total of 1429 patients were enrolled and all underwent head CT, with 520 patients included in the derivation phase. The primary outcome was the presence of an acute traumatic intracranial lesion (subdural, epidural, or parenchymal hematoma; subarachnoid hemorrhage; cerebral contusion; or depressed skull fracture). Figure 12.2 depicts an epidural hematoma on CT. The New Orleans decision aid was then validated on a separate cohort (n = 909) and demonstrated 100% sensitivity for any of the outcomes. Table 12.1 Accuracy of history for severe intracranial injury Source: Adapted from [9]. Dangerous mechanism is a pedestrian struck by a vehicle, an occupant ejected from a vehicle, or a fall from more than 5 stairs or 1 meter. Table 12.2 Accuracy of physical exam for severe intracranial injury Source: Adapted from [9]. In deriving the Canadian CT head decision aid (Table 12.4), investigators examined patients presenting to 10 Canadian EDs within 24 hours of blunt head trauma who had a loss of consciousness, amnesia, or disorientation and an initial GCS ≥13. Their primary outcomes included death, neurosurgical intervention, or clinically important brain injury requiring hospital admission and neurological follow‐up.12 Figure 12.1 Findings suggestive of basilar skull fractures are Battle sign, hemotympanum, cerebrospinal fluid otorrhea, or raccoon eyes. Table 12.3 The New Orleans criteria for patients with minor head injury Source: Data from [10]. Figure 12.2 Acute epidural hematoma. Table 12.4 The Canadian CT head rule Source: Data from [11].
Chapter 12
Adult Blunt Head Injury
Background
Clinical question
Risk factor
Positive likelihood ratio
Negative likelihood ratio
Dangerous mechanism
2.1 (1.5–2.9)
0.75 (0.61–0.92)
Pedestrian struck
3.0–4.3
0.87–0.93
Age ≥ 65 years
2.3 (1.8–3.1)
0.77 (0.72–0.82)
Age ≥ 60 years
2.2 (1.6–3.2)
0.78 (0.70–0.85)
Coagulopathy
2.2 (1.0–4.2)
0.97 (0.79–1.0)
Male
1.1–1.3
0.56–0.80
Vomiting ≥2 episodes
3.6 (3.1–4.1)
0.76 (0.61–0.95)
Any vomiting
2.3 (1.8–2.8)
0.89 (0.85–0.93)
Nausea
1.4–1.9
0.84–0.94
Postinjury seizure
2.5 (1.3–4.3)
0.98 (0.95–0.99)
Anterograde amnesia
2.2 (1.6–3.1)
0.75 (0.64–0.88)
Any amnesia
1.5 (0.81–2.8)
0.55 (0.31–0.97)
Loss of consciousness
1.6 (1.1–2.1)
0.60 (0.39–0.81)
Headache
1.2 (1.0–1.5)
0.84 (0.73–0.94)
Risk factor
Positive likelihood ratio
Negative likelihood ratio
Any skull fracture
16 (3.1–59)
0.85 (0.48–0.98)
Basilar skull fracture
6.0 (3.9–8.0)
0.84 (0.76–0.92)
Open skull fracture
4.6–5.0
0.90–0.91
GCS decline
3.4–16
0.76–0.80
GCS <15 at 2 hours
3.4 (1.4–8.4)
0.57 (0.34–0.96)
Initial GCS 13
4.9 (2.8–8.5)
0.88 (0.84–0.93)
Initial GCS 14
4.2 (0.85–7.6)
0.71 (0.60–0.83)
Focal neurological deficit
1.9–7.0
0.91–0.96
Trauma above clavicles
1.3 (1.1–1.5)
0.80 (0.62–1.0)
If none of the following are present, patients are unlikely to have a positive CT and do not need CT imaging:
CT imaging is indicated if any of the following are present:
High risk (for neurosurgical intervention)
Medium risk (for brain injury on head CT) 
Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access



