Chapter 40 Acute renal failure
Acute renal failure (ARF) remains a major diagnostic and therapeutic challenge for the critical care physician. The term ‘ ARF’ describes a syndrome characterised by a rapid (hours to days) decrease in the kidney’s ability to eliminate waste products. Such loss of function is clinically manifested by the accumulation of end-products of nitrogen metabolism such as urea and creatinine. Other typical clinical manifestations include decreased urine output (not always present), accumulation of non-volatile acids and an increased potassium and phosphate concentration.
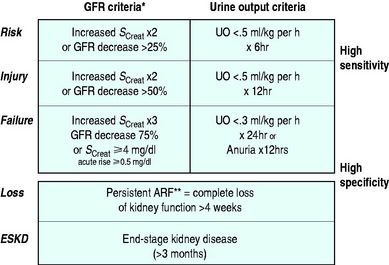
Depending on the criteria used to define its presence, ARF has been reported to occur in 15–20% of intensive care unit (ICU) patients.1 Recently a consensus definition and classification for ARF have been developed and validated in hospital and ICU patients.2–4 This definition, which goes by the acronym of RIFLE, divides renal dysfunction into the categories of risk, injury and failure (Figure 40.1) and is likely to be the dominant approach to defining ARF in ICUs for the next 5–10 years. Using this classification, the incidence of some degree of renal dysfunction has reported to be up to 67% in a recent study of > 5000 ICU patients.3 In hospital patients, the development of failure (in the RIFLE classification) increases the odds ratio of death 10 times.4
DIAGNOSIS AND CLINICAL CLASSIFICATION
PRERENAL RENAL FAILURE
This form of ARF is by far the most common in ICU. The term indicates that the kidney malfunctions predominantly because of systemic factors, which decrease GFR. For example, GFR may be decreased if renal blood flow is diminished by decreased cardiac output, hypotension or raised intra-abdominal pressure. Raised intra-abdominal pressure can be suspected on clinical grounds and confirmed by measuring bladder pressure with a urinary catheter. A pressure of > 25–30 mmHg above the pubis should prompt consideration of decompression. If the systemic cause of renal failure is rapidly removed or corrected, renal function improves and relatively rapidly returns to near-normal levels. However, if intervention is delayed or unsuccessful, renal injury becomes established and several days or weeks are then necessary for recovery. Several tests (measurement of urinary sodium, fractional excretion of sodium and other derived indices) have been promoted to help clinicians identify the development of such ‘ established’ ARF. Unfortunately, their accuracy is doubtful.5 The clinical utility of these tests in ICU patients who receive vasopressors, massive fluid resuscitation and loop diuretic infusions is low. Furthermore, it is important to observe that prerenal ARF and established ARF are part of a continuum, and their separation has limited clinical implications. The treatment is the same – treatment of the cause while promptly resuscitating the patient using invasive haemodynamic monitoring to guide therapy.
PARENCHYMAL RENAL FAILURE
This term is used to define a syndrome where the principal source of damage is within the kidney and where typical structural changes can be seen on microscopy. Disorders which affect the glomerulus or the tubule can be responsible (Table 40.1).
Table 40.1 Causes of parenchymal acute renal failure
| Glomerulonephritis |
| Vasculitis |
| Interstitial nephritis |
| Malignant hypertension |
| Pyelonephritis |
| Bilateral cortical necrosis |
| Amyloidosis |
| Malignancy |
| Nephrotoxins |
Among these, nephrotoxins are particularly important, especially in hospital patients. The most common nephrotoxic drugs affecting ICU patients are listed in Table 40.2. Many cases of drug-induced ARF rapidly improve upon removal of the offending agent. Accordingly, a careful history of drug administration is mandatory in all patients with ARF. In some cases of parenchymal ARF, a correct working diagnosis can be obtained from history, physical examination and radiological and laboratory investigations. In such patients one can proceed to a therapeutic trial without the need to resort to renal biopsy. However, if immunosuppressive therapy is considered, renal biopsy is recommended. Renal biopsy in ventilated patients under ultrasound guidance does not carry additional risks compared to standard conditions.
Table 40.2 Drugs which may cause acute renal failure in the intensive care unit
| Radiocontrast agents |
| Aminoglycosides |
| Amphotericin |
| Non-steroidal anti-inflammatory drugs |
| β-lactam antibiotics (interstitial nephropathy) |
| Sulphonamides |
| Acyclovir |
| Methotrexate |
| Cisplatin |
| Cyclosporin A |
| FK-506 (tacrolimus) |
HEPATORENAL SYNDROME
This condition is a form of ARF, which occurs in the setting of severe liver dysfunction in the absence of other known causes of ARF. Typically, it presents as progressive oliguria with a very low urinary sodium concentration (< 10 mmol/l). Its pathogenesis is not well understood. It is important to note, however, that, in patients with severe liver disease, other causes of ARF are much more common. They include sepsis, paracentesis-induced hypovolaemia, raised intra-abdominal pressure due to tense ascites, diuretic-induced hypovolaemia, lactulose-induced hypovolaemia, alcoholic cardiomyopathy, and any combination of these. The avoidance of hypovolaemia by albumin administration in patients with spontaneous bacterial peritonitis has been shown to decrease the incidence of renal failure in a recent randomised controlled trial (RCT).6 These causes must be looked for and promptly treated. Recent small studies suggest that a vasopressin derivative called terlipressin may improve GFR in this condition.7
RHABDOMYOLYSIS-ASSOCIATED ARF
This condition accounts for close to 5–10%8 of cases of ARF in ICU depending on the setting. Its pathogenesis involves prerenal, renal and postrenal factors. It is now typically seen following major trauma, drug overdose with narcotics, vascular embolism, and in response to a variety of agents which can induce major muscle injury. The principles of treatment are based on retrospective data, small series and multivariate logistic regression analysis, because no RCTs have been conducted. They include prompt and aggressive fluid resuscitation, elimination of causative agents, correction of compartment syndromes, the alkalinisation of urine (pH > 6.5) and the maintenance of polyuria (> 300 ml/h). The role of mannitol is controversial.

Full access? Get Clinical Tree