
ACUTE LIVER FAILURE AND PORTAL HYPERTENSION
ACUTE LIVER FAILURE
Fulminant hepatic failure is synonymous with acute liver failure (ALF), a rare disorder that often leads to devastating consequences. ALF is rapid deterioration of liver function resulting in altered mutation and coagulopathy in previously normal individuals. The loss of hepatic function quickly leads to multiorgan failure and frequently death. Approximately 2,000 cases of ALF occur in the United States per year.1 The clinical syndrome was originally described as “sudden severe impairment of hepatic function resulting in jaundice and followed by hepatic encephalopathy (HE) within 8 weeks of the onset, in the absence of prior liver disease.”2 The most widely accepted definition of ALF is the presence of coagulation abnormality and any degree of encephalopathy in a patient without preexisting cirrhosis and with an illness of <26 weeks duration.3 ALF can be classified according to the length of illness such as hyperacute (<7 days), acute (7–21 days), or subacute (>21 days and <26 weeks), but these terms are not helpful since there is no prognostic significance distinct from the cause of the illness.
The etiology of ALF provides one of the best indicators of prognosis4 and also dictates specific management options. ALF can be induced by viral (hepatitis A, hepatitis B, herpes, cytomegalovirus, Epstein-Barr virus), vascular (Budd-Chiari syndrome, right heart failure, shock liver), metabolic (Wilson’s disease, hemolysis–elevated liver enzymes–low platelet count syndrome, acute fatty liver of pregnancy, tyrosinemia), drugs and toxins (acetaminophen, Amanita phalloides , Bacillus cereus toxin, herbal remedies), or miscellaneous/indeterminate (malignant infiltration, autoimmune hepatitis, sepsis) causes. Acetaminophen toxicity is the leading cause of ALF in the United States, accounting for 40% of cases.1 Acetaminophen-induced ALF is suspected with evidence of excessive ingestion, usually because of a suicide attempt or supratherapeutic quantities of pain medication. Acetaminophen is a dose-related toxin with most ingestions which lead to ALF exceeding 10 g/day. Acetaminophen levels should be drawn on all patients presenting with ALF, and the agent N-acetylcysteine (NAC) started. Acetaminophen overdose leads to the accumulation of N-acetyl-p-benzoquinone imine, a metabolite normally conjugated by glutathione that is toxic to hepatocytes.5 Excessive ingestion of acetaminophen leads to depletion of glutathione stores, and NAC augments glutathione levels. NAC should be started as early as possible but may still be useful even 48 hours or more after ingestion. The oral dose of NAC is 140 mg/kg diluted to 5% solution, followed by 70 mg/kg by mouth q4h × 17 doses. NAC can also be administered intravenously in patients with worsening mental status or gastrointestinal (GI) bleeding. The loading dose is 150 mg/kg in 5% dextrose over 15 minutes; maintenance dose is 50 mg/kg given over 4 hours followed by 100 mg/kg administered over 16 hours.3 Numerous clinical trials have established the efficacy of NAC for the treatment of acetaminophen-induced ALF. ALF patients are heterogeneous but share the common disease process of acute hepatocyte necrosis and its sequelae. Presenting symptoms are often nonspecific, including fatigue,malaise, anorexia, nausea, abdominal pain, fever, and jaundice.1 Often these symptoms progress to severe coagulopathy and encephalopathy and/or coma. The patient’s clinical condition should be monitored regularly including frequent vital signs, blood glucose, and neurologic status. Initial laboratory testing should include a complete blood count, biochemical, hematologic, immunologic, hepatitis panel, and toxic drug screens. An arterial blood gas and lactate levels should be checked to assess metabolic disturbances. Radiographic tests include an abdominal ultrasound to evaluate hepatic and portal venous flow patterns, and triphasic CT to evaluate the hepatic parenchyma (unless renal insufficiency or failure is present in which case intravenous contrast use is precluded). Clinical deterioration is often rapid and any worsening in the patient’s condition should warrant urgent referral to a transplant center. Patients who present in full-blown ALF often have severe metabolic acidosis, hypoglycemia, coagulopathy, and encephalopathy or coma.6 Stabilization of these patients includes volume resuscitation, mechanical ventilation, and hemodynamic support. Appropriate candidates should be urgently listed for liver transplantation as quickly as possible. Next, we will discuss the systemic effects of ALF by going through each organ system in detail.
Encephalopathy and Intracranial Hypertension (IH)
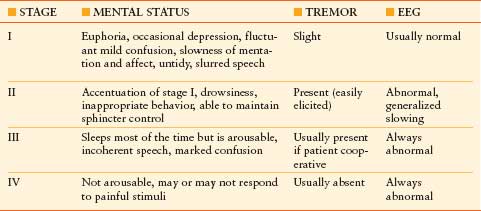
The neurologic effects of ALF range from minimal to striking. Encephalopathy, the hallmark feature of ALF, may vary from subtle changes in affect, insomnia, and difficulties with concentration (stage I), to deep coma (stage IV).1 The prognosis of ALF is inversely correlated with the degree of encephalopathy. Table 51.1 illustrates the grades of encephalopathy. The most serious complication of ALF is cerebral edema and intracranial hypertension (ICH) which affects approximately 50%-80% of patients with severe ALF (grade III or IV coma).7 Uncal herniation can result and is uniformly fatal. Patients with grade I-II encephalopathy seldom show signs of cerebral edema. The risk of edema increases to 25%-35% with progression to grade III, and 65%-75% or more in patients reaching grade IV coma.3 Patients with grade I-II encephalopathy should be managed in a quiet environment to minimize agitation, and sedation should be avoided. Frequent mental status checks should be performed and head imaging with CT obtained to exclude other causes of encephalopathy. Lactulose can reduce elevated ammonia levels which may play a pathogenic role in the development of cerebral edema/ICH. As patients progress to grade III or IV encephalopathy, intubation for airway protection must be undertaken. The patients should be positioned with the head elevated at 30 degrees and efforts made to avoid patient stimulation. Propofol is often used as the choice of sedation because it may reduce cerebral blood flow (CBF)3; however, its effectiveness has not been shown in controlled studies.
TABLE 51.1
STAGES OF ENCEPHALOPATHY IN ALF
Two theories have been proposed to account for intracranial hypertension in ALF: (1) brain edema due to osmotic astrocyte swelling secondary to ammonia-induced accumulation of glutamine, and (2) alteration of CBF regulation with increased intracranial blood volume.8 The typical course of grade III or IV HE includes a reduction in CBF coupled with a reduction in cerebral metabolic rate early on, followed by gradual cerebral vasodilatation due to the loss of cerebral autoregulation. This results in increased cerebral blood volume and edema. The preterminal phase shows a marked reduction in CBF resulting from cerebral edema, with cerebral herniation as the end result.7
Clinical signs of IH include systemic hypertension, bradycardia, abnormal pupillary signs, aggravation of HE, epileptiform activity, and decerebrate posturing. However, most of these clinical signs are nonspecific. The most accurate method to diagnose IH is intracranial pressure (ICP) monitoring. Although the advantages of ICP monitoring in ALF patients have not been demonstrated by a randomized study, ICP monitoring may be helpful to establish the presence of IH and guide specific therapy.8 ICP transducers can be placed in the brain parenchyma, epidural, or subdural spaces. Epidural devices have lower complication rates (3.8%) than subdural bolts (20%) or parenchymal monitors (22%).9,10 In ALF, epidural transducers may be the safest choice to monitor ICP even though they are less precise than the other devices.10 Although placement of these invasive monitors is associated with the risk of hemorrhage, the use of recombinant factor VIIa (rFVIIa) before the procedure appears to minimize this risk11; a single dose of 40 µg/kg of rFVIIa is recommended prior to placement.
Transcranial Doppler is a noninvasive measurement of the systolic flow velocity of the middle cerebral artery. Attenuation of the diastolic flow signal may be a sign of IH and decreased cerebral perfusion. A pulsatility index (systolic velocity–diastolic velocity/systolic velocity) >1.6 is a poor prognostic sign.7 Jugular venous oximetry measures venous oxygenation in the superior jugular bulb of the internal jugular vein, which is representative of cerebral oxygen consumption and delivery. If one assumes that the cerebral metabolic rate remains constant, the arteriojugular venous oxygen difference (AVjDO2) will change in response to changes in CBF; this will essentially be a reflection of the ratio of the flow to metabolism. A normal AVjDO2 is 5–6 mL/100 mL; a narrow AVjDO2 difference is suggestive of cerebral hyperemia and a widened AVjDO2 difference is suggestive of cerebral ischemia. AVjDO2 measurements can be obtained at two different levels of pCO2 to see the variability in CBF in response to CO2 reactivity. If the AVjDO2 difference normalizes from a low value, hyperventilation may be effective to decrease cerebral hyperemia. Alternatively, an AVjDO2 difference >6 when the pCO2 is low suggests cerebral ischemia, and elevating the pCO2 is needed to maintain adequate CBF.
The treatment of elevated ICP involves decreasing the brain volume or decreasing the CBF and intracranial blood volume (or both). Mannitol and hypertonic saline increase blood osmolarity, thereby inducing fluid movement from the brain to the vascular space. Mannitol (0.5–1 g/kg IV) repeated once or twice as needed, provided serum osmolality does not exceed 320 mOsm/L, is recommended to treat ICH.3 The efficacy of mannitol is affected by acute renal failure, and hemodialysis may also be needed to remove fluid. A recent controlled trial of 30% hypertonic saline to maintain serum sodium levels of 145–155 mEq/L suggests that induction and maintenance of hypernatremia may be used to prevent the rise in ICP.12 Survival benefits could not be demonstrated in this trial however, and the role of hypertonic saline as a prophylactic measure requires larger studies.
Hyperventilation, indomethacin, thiopental, and induced hypothermia reduce ICP through vasoconstriction of cerebral blood vessels, thereby decreasing CBF. The American Association for the Study of Liver Diseases (AASLD) position paper on the management of ALF does not support prophylactic hyperventilation in patients with ALF.3 If ICH cannot be controlled with mannitol and other general management guidelines; hyperventilation may be instituted temporarily in an attempt to acutely lower ICP and prevent impending herniation. Indomethacin induces cerebral vasoconstriction through inhibition of the endothelial cyclooxygenase pathway, alterations in extracellular pH, and reduction in cerebral temperature.13 Studies using indomethacin are of small scale, and its use should be evaluated in a randomized, controlled study before wider use. Thiopental induces cerebral vasoconstriction possibly by inhibition of nitric oxide synthase, which is thought to be important in the pathogenesis of increased ICP in ALF. A continuous infusion is started and titrated based upon the EEG (5–10 second EEG burst suppression), ICP, and hemodynamics. Most systemic hypotension limits its use and may necessitate additional pressors or inotropes to maintain adequate mean arterial pressures. Patients who develop worsening encephalopathy and those with signs of IH must be urgently listed for liver transplantation if they are appropriate candidates; needless to say, the workup should be expeditious.
Nausea, vomiting, and loss of appetite are part of the prodrome of ALF, and patients may present with profound dehydration. Most patients will require fluid resuscitation initially with colloids primarily and complemented with crystalloid solutions.6 Systemic vasodilation, low systemic vascular resistance, hypotension, and a compensatory increase in cardiac output are the notable clinical cardiovascular sequelae of ALF. Abnormal oxygen transport and utilization is also present; delivery of oxygen to the tissues is adequate but there is a decrease in tissue oxygen uptake,1 resulting in tissue hypoxia and lactic acidosis.14 Low systemic vascular resistance results in hypotension even in the volume-resuscitated patient, and a pulmonary artery catheter is often useful to assess volume status and guide further management. Inotropic or pressor support may be required to maintain an adequate mean arterial pressure. Norepinephrine and dopamine are generally used if needed to maintain vital organ perfusion.1,3,6 Vasoconstrictive agents such as vasopressin (VP) are generally avoided unless major systemic hypotension is present.3
Respiratory
Patients often hyperventilate and develop a respiratory alkalosis before a metabolic acidosis as liver failure progresses.2 Mortality in ALF escalates with the presence of pulmonary edema and acute respiratory distress syndrome (ARDS).1,2 ARDS is present in as many as one-third of patients.15 Ventilation–perfusion mismatch may develop acutely and worsen as the liver function deteriorates, and resulting hypoxia can contribute to neurologic injury. Positive end-expiratory pressure may compromise cardiac output and oxygen delivery, and result in increased ICP and hepatic congestion.1,2 Treatment with increased FiO2 is the most appropriate intervention. Patients who develop ARDS in the setting of ALF can successfully undergo liver transplantation, but the risk of death is high.16
Gastrointestinal/Metabolic
Upper GI bleeding is a recognized complication and often stress related. Histamine-2 receptors blocking agents and proton pump inhibitors have been shown to be efficacious in several trials. Numerous metabolic derangements are common in ALF including alkalosis, acidosis, hypoglycemia, hypophosphatemia, and hypokalemia. Hypoglycemia, seen in up to 45% of ALF patients,1 is an indicator of major hepatic necrosis which leads to defective glycogenolysis, gluconeogenesis, and insulin metabolism. Treatment is with continuous glucose infusion. Electrolytes should be supplemented and followed closely. Enteral nutrition should be started early when feasible.
Renal Failure
Renal failure is common, with the reported incidence varying from 40% to 85%.6 It is often multifactorial, with prerenal azotemia, renal ischemia, acute tubular necrosis, and hepatorenal syndrome (HRS) as common causes. Although few patients die of renal failure alone, it often contributes to mortality and suggests a poorer prognosis.3 Avoidance of nephrotoxins and maintenance of adequate intravascular volume are important to maintain renal function. When hemodialysis is needed, continuous venovenous hemodialysis (CVVHD) is the preferred mode.2,3,6,17 CVVHD tends to be better tolerated and may have more beneficial effects on ICP.17,18 Intermittent hemodialysis has been associated with increases in ICP and decreases in CPP, whereas the opposite has been shown in patients receiving CVVHD.18,19
Hematologic
The normal liver is responsible for the synthesis of several clotting factors involved in the clotting cascade. The primary hematologic derangements seen in ALF include platelet dysfunction and thrombocytopenia, reduced fibrinogen, and a prolonged prothrombin time (PT).1,3,6,18 However, spontaneous, clinically meaningful bleeding is uncommon in ALF patients (<10%).18 The PT is used as a prognostic indicator as well as a tool to follow the progress of the liver injury; thus, correction of the PT is not necessary unless there is clinical bleeding or an invasive procedure is planned. Complete correction of the coagulopathy and thrombocytopenia is generally not achievable and can lead to volume overload and oxygenation issues, as well as exacerbation of ICH. The use of rFVIIa has been examined in treatment of the coagulopathy in ALF and may be useful in facilitating performance of invasive procedures (such as intracranial monitoring devices) in these patients, especially in the setting of renal failure and volume overload.20 Further studies and analysis of cost–benefit ratio are needed prior to becoming standard therapy.
Infection
The liver is the site of complement synthesis, with low levels of complement reported in ALF.6 Reduced complement has been associated with impaired opsonization1,6 leading to sepsis. The most common pathogens are Staphylococcal species, streptococcal species, and gram-negative rods.1,6,18 Fungal infections (particularly Candida albicans) occur in up to one-third of ALF patients with risk factors including renal failure and prolonged antibiotic therapy for existing bacterial infections. Common sites of infection include pneumonia (50%), bacteremia (20%), and urinary tract infection (25%).17 Prophylactic antimicrobial therapy reduces the incidence of infection in certain groups of patients with ALF, but no actual survival benefit has been shown. If prophylactic antibiotics are not given, surveillance for infection including chest x-rays and periodic cultures of sputum, blood, and urine should be done.
Transplantation and Prognosis
Orthotopic liver transplantation (OLT) remains the only definitive therapy for patients who have sustained massive hepatic necrosis without regeneration of enough hepatocytes to sustain life. Overall survival rates in ALF have improved from 15% in the pretransplant era to >60% with transplantation.3 Advances in critical care and trends toward etiologies such as acetaminophen have helped improve survival. A delay in a patient getting on the transplant list can lead to the probability of a complication precluding transplant. Contraindications to transplant include an extrahepatic malignancy, uncontrolled sepsis, irreversible brain damage, or unresponsive cerebral edema with a sustained elevation of ICP (>50 mm Hg) and a decrease in CPP (<40 mm Hg).17
Accurate prognosis for survival in ALF is important, given the limited organ supply and lack of good alternative therapies. The most commonly utilized and most frequently tested of the many prognostic criteria for ALF are from the King’s College (Table 51.2).21 More published data exist to support the use of acetaminophen than the nonacetaminophen criteria.Other criteria including the patient’s MELD score on admission and APACHE II scores have been looked at in several studies. Currently, available prognostic scoring systems do not adequately predict outcome and determine candidacy for liver transplantation, therefore, decisions on whether to transplant a patient or not should look at the whole picture and not rely on these guidelines entirely.
TABLE 51.2
KING’S COLLEGE CRITERIA
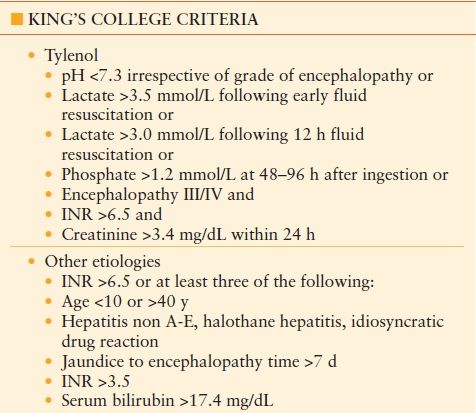
From O’Grady J, Alexander G, Hayllar K, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology , (1989);97(2): 439–455 with permission

Full access? Get Clinical Tree








