Chapter 54 Acute calcium disorders
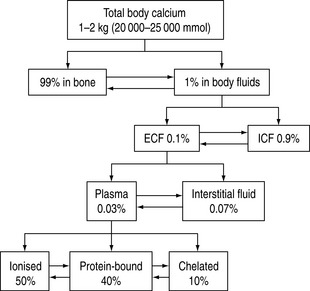
Calcium is an important cation and the principal electrolyte of the body. A total of 1–2 kg is present in the average adult, of which 99% is found in bone. Of the remaining 1%, nine-tenths is present in the cells and only a tenth in the extracellular fluid. In plasma, 50% of the calcium is ionised, 40% bound to plasma proteins, mainly to albumin, and the remaining 10% is chelated to anions such as citrate, bicarbonate, lactate, sulphate phosphate and ketones.1 The chelated fraction is usually of little clinical importance, but is increased in conditions where some of these anionic concentrations might be elevated, as in renal failure. Whilst most calcium inside the cell is in the form of insoluble complexes, the concentration of intracellular ionised calcium is about 0.1 μmol/l, creating a gradient of 10 000:1 between plasma and intracellular fluid levels of ionised calcium.2 A schematic illustration of calcium distribution within the various body compartments is shown in Figure 54.1.
Because ionised calcium is the biologically active component of extracellular fluid calcium with respect to physiological functions (Table 54.1) and is also the reference variable for endocrine regulation of calcium homeostasis, its measurement is recognised as being one of prime importance in the management of disorders of calcium homeostasis.
Table 54.1 Functions of calcium1,15
| Excitation – contraction coupling in cardiac, skeletal and smooth muscle |
| Cardiac action potentials and pacemaker activity |
| Release of neurotransmitters |
| Coagulation of blood |
| Bone formation and metabolism |
| Hormone release |
| Ciliary motility |
| Catecholamine responsiveness at the receptor site7 |
| Role as a strong cation |
| Regulation of cell growth and apoptosis |
METABOLIC FACTORS INFLUENCING CALCIUM HOMEOSTASIS
Changes in pH alter calcium protein binding. An increase in pH by 0.1 pH units results in a decrease in ionised calcium by approximately 0.1 mmol/l.4
As magnesium is required for PTH secretion and end-organ responsiveness, alterations in serum magnesium have an impact on serum calcium concentration.
Turnover of calcium in the bone is predominantly under the control of PTH and calcitriol, although prostaglandins and some of the cytokines also play a role in it. Bone resorption is mediated by osteoclasts, whereas osteoblasts are involved in bone formation. The daily calcium balance is summarised in Table 54.2.
Table 54.2 Daily calcium balance
| Gastrointestinal tract | |
| Diet | 600–1200 mg/day |
| Absorbed | 200–400 mg/day |
| Secreted | 150–800 mg/day |
| Renal | |
| Filtered | 11 000 mg/day |
| Reabsorbed (97% in the proximal convoluted tubule) | 10 800 mg/day |
| Urinary calcium | 200 mg/day |
| Bone | |
| Turnover | 600–800 mg/day |
MEASUREMENT OF SERUM CALCIUM
Most hospital laboratories measure total serum calcium. The normal plasma concentration is 2.2–2.6 mmol/l. However, the ionised form (1.1–1.3 mmol/l) is the active fraction and its measurement is not routine in many laboratories, although most state-of-the-art blood gas analysers can measure serum ionised calcium concentrations. Estimation of ionised calcium from total serum calcium concentration using mathematical algorithms is unreliable in critically ill patients.5–7 Heparin forms complexes with calcium and decreases ionised calcium.8 A heparin concentration of < 15 units/ml of whole blood is therefore recommended for the measurement of ionised calcium.9 Anaerobic collection of the specimen is recommended, as CO2 loss from the specimen may result in alkalosis and reduction in ionised calcium concentration. Calcium levels are also reduced by a concomitant lactic acidosis owing to chelation by lactate ion.10 Free fatty acids (FFAs) increase calcium binding to albumin and may form a portion of the calcium-binding site.11 Increases in FFAs may be seen in relation to stress, use of steroids, catecholamines and heparin. The impact of pH on calcium measurements has been described above. The normal reference levels of serum calcium are reduced in pregnancy and in the early neonatal period.12
HYPERCALCAEMIA IN CRITICALLY ILL PATIENTS
The frequency of hypercalcaemia in critically ill patients is not well established, although it is not as common as hypocalcaemia. Depending on the patient population, the reported incidence ranges from 3–5% to as high as 32%.13,14 Admission to the intensive care unit (ICU) with a primary diagnosis of a hypercalcaemic crisis is uncommon. Although a number of aetiologies has been described (Table 54.3), in the critical care setting it is usually due to malignancy-related hypercalcaemia, renal failure or posthypocalcaemic hypercalcaemia.15 Before undertaking a work-up for hypercalcaemia, it is important to exclude false-positive measurements. This is usually the result of inadvertent haemoconcentration during venepuncture and elevation in serum protein, although ionised calcium levels are not reported to be affected by haemoconcentration.16Pseudohypercalcaemia has also been described in the setting of essential thrombocythaemia. The erroneous result is thought to be due to in vitro release of calcium from platelets, analogous to the pseudohyperkalaemia seen in the same condition.17
Table 54.3 Causes of hypercalcaemia
| Common causes of hypercalcaemia in the critically ill patient |
| Complication of malignancy |
| Bony metastases |
| Humoral hypercalcaemia of malignancy |
| Posthypocalcaemic hypercalcaemia |
| Recovery from pancreatitis15 |
| Recovery from acute renal failure following rhabdomyolysis37–41 |
| Primary hyperparathyroidism |
| Adrenal insufficiency23,24 |
| Prolonged immobilisation18–21 |
| Disorders of magnesium metabolism |
| Use of total parenteral nutrition42 |
| Hypovolaemia |
| Iatrogenic calcium administration |
| Less common causes of hypercalcaemia in the critically ill patient |
| Granulomatous diseases – sarcoidosis, tuberculosis, berylliosis |
| Vitamin A and D intoxication |
| Multiple myeloma |
| Endocrine |
| Thyrotoxicosis |
| Acromegaly |
| Phaeochromocytoma |
| Lithium – chronic therapy |
| Rare association between drugs and hypercalcaemia |
| Theophylline, omeprazole and growth hormone therapy |
From a pathophysiological standpoint, hypercalcaemia may be due to an elevation in PTH, in which case the homeostatic regulatory and feedback mechanisms are preserved, and this is termed equilibrium hypercalcaemia. Alternatively, it could be a non-parathyroid-mediated hypercalcaemia with associated breakdown of homeostatic mechanisms, and this situation is termed dysequilibrium hypercalcaemia.
MECHANISMS OF HYPERCALCAEMIA
Posthypocalcaemic hypercalcaemia is a transient phenomenon seen in patients following a period of hypocalcaemia.15 This has been attributed to a parathyroid hyperplasia which develops during the period of hypocalcaemia, resulting in a rebound hypercalcaemia following resolution of the underlying hypocalcaemic disorder.
Immobilisation hypercalcaemia results from an alteration in balance between bone formation and resorption.18–21 This leads to loss of bone minerals, hypercalcaemia, hypercalciuria and increased risk of renal failure. In patients with normal bone turnover, immobilisation rarely causes significant hypercalcaemia. However, in patients with rapid turnover of bone (children, postfracture patients, hyperparathyroidism, Paget’s disease, spinal injuries and Guillain–Barré syndrome), this may result in severe hypercalcaemia.
Extrarenal production of calcitriol by lymphocytes in granulomata is thought to be the predominant mechanism of hypercalcaemia in granulomatous diseases.22
Only 10–20% of patients with adrenal insufficiency develop hypercalcaemia.23,24 The aetiology of this is thought to be multifactorial: intravascular volume depletion, haemoconcentration of plasma proteins and the loss of antivitamin D effects of glucocorticoids.
For rarer causes of hypercalcaemia, the reader is referred to a recent review.25

Full access? Get Clinical Tree