ACUTE APPENDICITIS
CASE SCENARIO
A 27-year-old woman with no past medical history presents to the emergency room with 24 hours of abdominal pain. The day prior to presentation, she developed diffuse, vague abdominal discomfort. She lost her appetite and went to bed early secondary to malaise. The following morning, the pain worsened in intensity, became sharp, and localized to the right lower quadrant.
The patient is afebrile, with normal vital signs. On examination, she is focally tender to palpation in the right lower quadrant with voluntary guarding. Palpation of the left lower quadrant reproduces pain on the right. Her lab work is unremarkable with the exception of a mild leukocytosis to 13.
EPIDEMIOLOGY
Acute appendicitis is one of the most common surgical diagnoses presenting to the emergency room. It occurs most frequently among patients between their teens and thirties, with a slight male predominance (1.4:1) and with the highest proportion of cases affecting patients aged 10 to 19 years.1,2 Prompt recognition is paramount to prevent appendiceal perforation; however, appendicitis in women, children, and the elderly may present with an atypical constellation of signs and symptoms that delays diagnosis.
PATHOPHYSIOLOGY
The appendix is a blind-ending pouch arising from the cecum at the point where the taenia coli converge. A true diverticulum, it contains all layers of the colonic wall. In appendicitis, a fecalith, tumor, or lymphocyte proliferation blocks the lumen, and the appendix distends with mucus. Distension compromises blood supply to the appendiceal wall, and stasis within the appendix allows for bacterial overgrowth. Bacteria then invade the compromised wall of the appendix, producing an inflammatory exudate that irritates the peritoneum. Local ischemia follows initial inflammation and progresses to perforation with the development of contained abscess, phlegmon, or generalized peritonitis.
CLINICAL PRESENTATION
The hallmark of appendicitis is abdominal pain that starts in the peri-umbilical region and is described as dull or cramping, followed by migration of discomfort to the right lower quadrant with a sharpening in quality. The peri-umbilical pain arises secondary to stimulation of visceral afferent nerve fibers at T8-T10 as intraluminal pressure increases. Pain becomes localized and sharp when inflammation extends to the serosa and irritates the parietal peritoneum. Other associated symptoms are nonspecific and may include anorexia, nausea, vomiting, diarrhea, and low-grade fever. Patients may complain of dysuria if the appendiceal tip assumes a pelvic location.
On examination, the classic finding is tenderness at McBurney’s point, a location one-third along a line drawn from the anterior superior iliac spine to the umbilicus. However, this right lower quadrant tenderness may be subdued if the tip of the appendix is retrocecal, or if it dives into the pelvis. In these circumstances, other physical examination findings may aid diagnosis. A positive Rovsing’s sign, when palpation of the left lower quadrant reproduces abdominal pain on the right, signifies peritoneal irritation in the right lower quadrant. Patients with a positive psoas sign have pain in the right abdomen with passive extension of the hip, suggesting a retrocecal appendix. With the obturator’s sign, flexion of the knee and internal rotation of the right hip reproduces pain and denotes a possible pelvic appendix. Although these tests are specific, their sensitivity is quite low, and they are frequently absent.
Fever, leukocytosis, and a left shift are later manifestations of appendicitis and may not appear until later in a patient’s course. If a patient presents with more than 48 hours of symptoms, the likelihood of perforation is high; these patients are often ill appearing and have more pronounced tenderness than in cases of early appendicitis.
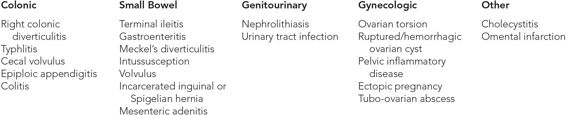
DIFFERENTIAL DIAGNOSIS
See Table 7–1.
WORKUP AND CHOICE OF IMAGING
In young, healthy men, who have a low incidence of diverticulitis and obviously no ovarian pathology, a history and examination consistent with appendicitis are often sufficient for diagnosis. Such patients can proceed to the operating room for appendectomy without further studies. However, in women of childbearing age, in patients older than 40 years, and in patients with significant comorbidities such as immunosuppression or diabetes, the similar presentation of other pathology necessitates an imaging study. Research has found that among such patients, advanced diagnostic imaging reduces the frequency of negative appendectomy by nearly fourfold, without an associated increase in the incidence of perforation.3,4
The most commonly obtained diagnostic study for acute appendicitis is an abdominal and pelvic computed tomography (CT) scan. Specific “appendicitis protocol” scans utilizing rectal contrast and focusing on the pelvis can be helpful in young patients, but in patients older than 20 years who may have other abdominal pathology, a full abdominal and pelvic CT with intravenous (IV) and oral contrast yields more data. The sensitivity of CT scan for the diagnosis of appendicitis is estimated at 93% to 94%, with a positive predictive value of 98%.3,5
Ultrasound is commonly obtained to diagnose appendicitis in pediatric patients in an attempt to limit ionizing radiation. However, results are operator dependent, and although the specificity for appendicitis is high, the sensitivity with ultrasound is significantly lower than CT at an estimated 48% to 83%.3,5
Magnetic resonance imaging (MRI) offers pregnant patients an alternative to CT.4,6 Gadolinium-based contrast is not approved for pregnant patients, so MRI in pregnancy should be obtained without contrast. The sensitivity and specificity of MRI for appendicitis is 99% to 100%.4 Despite this high degree of diagnostic accuracy, the high cost and low acquisition speed of MRI render it a less favorable technique than CT for nonpregnant patients.
IMAGING FINDINGS
 CT Scan
CT Scan
Normal Appendix
The appendix is identified on CT scan as a tubular, blind-ending structure arising from the cecum. Although classically located in the right lower quadrant, the tip of the appendix may course into the pelvis, the mid-abdomen, or even the right upper quadrant, beneath the liver. A normal appendix is <6 mm in diameter, has no stranding or wall thickening, and often fills with air or contrast.
Acute Appendicitis
The hallmarks of acute appendicitis are listed in Table 7–2. Compared with normal images, the appendix appears dilated with wall thickening and fat stranding. It does not fill with air or contrast, secondary to obstruction of the appendiceal lumen (Figures 7–1 through 7–8).