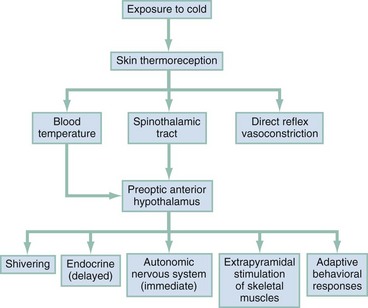
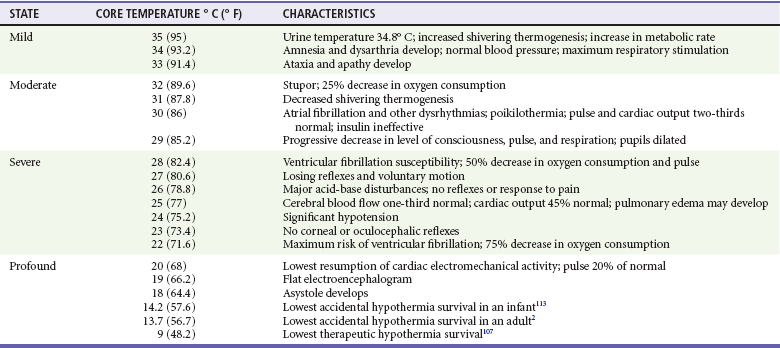
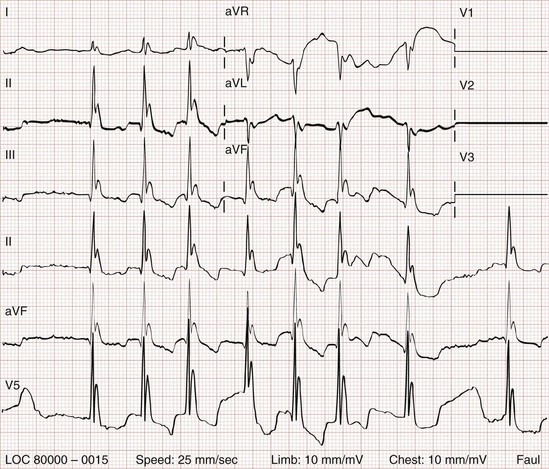
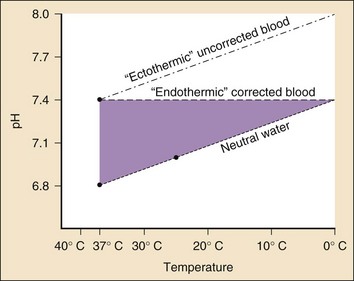
Chapter 140 The “reanimations” of profoundly cold victims in prolonged cardiac arrest and the emergence of therapeutic hypothermia after cardiac arrest help explain the contemporary allure of hypothermia. A 29-year-old Norwegian physician was successfully resuscitated from accidental hypothermia at 13.7° C after a 9-hour resuscitation.1 This included cardiopulmonary resuscitation initiated at the scene and 179 minutes of cardiopulmonary bypass.2 Cold weather has had a major impact on military history.3,4 Hannibal lost nearly half of his army of 46,000 while traversing the Alps in 218 BCE. The winter of 1777 took its toll on Washington’s troops at Valley Forge. Napoleon’s chief surgeon, Baron Larrey, reported that only 350 of the 12,000 men in the 12th division survived the cold during their retreat from Russia in 1812. Those soldiers who were rapidly rewarmed closest to the campfire died. The French subsequently suffered heavy losses in the Crimean War (1845-1855). These lessons were relearned during both world wars. Many pilots and U-boat crews perished from the cold water in the North Atlantic. Approximately 10% of the U.S. casualties in Korea were cold related. Innumerable cold-related tragedies affect both military personnel and civilians, in particular hunters, sailors, skiers, climbers, boaters, swimmers, and survivors of some natural disasters. Widespread participation in outdoor winter sports increases the number of patients who have hypothermia. Hypothermia is geographically and seasonally pervasive.5–7 Most cases occur in urban settings. “Primary” hypothermia fatalities are classified as accidental, homicidal, or suicidal. Death certificate data, however, under-report secondary hypothermia deaths, in which cold complicates many systemic diseases. The effect of cold on mortality from cardiovascular and neurologic disorders is greatly underestimated.8 Hypothermia is defined as a core temperature below 35° C. Many variables contribute to the development of accidental hypothermia. Exposure, age, health, nutrition, medication, and intoxicants can decrease heat production, increase heat loss, or interfere with thermostability.9 The healthy individual’s compensatory responses to heat loss through conduction, convection, radiation, and evaporation are often overwhelmed by exposure. Medications can also interfere with thermoregulation. Central nervous system (CNS) problems commonly decrease the efficiency of thermoregulation.10 Physiology of Temperature Regulation The preoptic anterior hypothalamus orchestrates nonshivering heat conservation and dissipation. Serotonergic and dopaminergic neurons are pivotal. They exert immediate control through the autonomic nervous system and delayed control through the endocrine system. Thermal suppression or activation of the sympathetic nervous system with cold-induced release of norepinephrine also occurs. Cold stimulates the hypothalamus to release thyrotropin-releasing hormone. This activates the anterior pituitary gland, which releases thyroid-stimulating hormone and results in the release of thyroxine from the thyroid gland.11 Cutaneous and respiratory heat loss is markedly influenced by the ambient temperature, air motion, and relative humidity. Greater losses occur in a cool, dry, windy environment (windchill index). When the body is not perspiring, most heat loss is through radiation and convection. Convective losses become significant in immersion-induced hypothermia. Children cool faster than adults do because of the elevated ratios of surface area to mass. Chronic cold exposure may result in gradual evolutionary adaptations and thermal acclimation (Fig. 140-1). The physiologic characteristics of hypothermia are described in Table 140-1. The bradycardia of hypothermia results from decreased spontaneous depolarization of the pacemaker cells. As a result, the bradydysrhythmia is refractory to atropine. The electrocardiographic features of hypothermia are unique.12,13 Initially described by Tomaszewski in 1938, the Osborn (J) wave is seen at the junction of the QRS complex and ST segment (Fig. 140-2). J waves are potentially diagnostic but not prognostic. They may appear at any temperature below 32° C. The size of the J wave is not related to arterial pH but does increase with temperature depression. J waves are normally upright in the aVL, aVF, and left precordial leads.14 The J deflection may be a result of hypothermic ion flux alterations, with delayed depolarization or early repolarization of the left ventricular wall. It can also be seen during local cardiac ischemia and with sepsis or CNS lesions, hypercalcemia, and the Brugada syndrome. Some J waveform abnormalities simulate a myocardial injury current. Hypothermic electrocardiographic changes are not easily recognized by computer programs. Reliance on computer interpretations can result in mistaken thrombolysis, which would be expected to exacerbate preexistent coagulopathies.15 The development of ventricular fibrillation (VF) or asystole in hypothermia is multifactorial. Putative explanations include tissue hypoxia, physical jostling, electrophysiologic or acid-base disturbances, and autonomic dysfunction. Asystole and VF can occur spontaneously when the core temperature falls below 25° C.16,17 Hypothermia causes a decrease in transmembrane resting potential, which in turn decreases the threshold for ventricular dysrhythmias. VF can also result from an independent focus or a reentrant phenomenon. When the heart is cold, a large dispersion of repolarization exists, which facilitates the development of a conduction delay. The action potential is also prolonged. The term core temperature afterdrop refers to a further decline in an individual’s core temperature after removal from the cold. The two processes that contribute to afterdrop are simple temperature equilibration across a gradient and circulatory changes. Countercurrent cooling of the blood, which is perfusing cold tissues, results in a temperature decline until the gradient is eliminated.18 Active external rewarming of the extremities obliterates peripheral vasoconstriction and reverses arteriovenous shunting. This was most vividly demonstrated by Hayward, who measured his own esophageal, rectal, tympanic, and cardiac temperatures (by use of a flotation tip catheter) after cooling in 10° C water on three different days.19 Warm bath immersion rewarming caused a 30% fall in mean arterial pressure coupled with a 50% decline in peripheral vascular resistance. Simple exposure to cold induces a diuresis regardless of an individual’s state of hydration. Hypothermia depresses renal blood flow, reducing it by 50% at 27 to 30° C. The kidneys then excrete a large amount of dilute urine, termed cold diuresis. Cold diuresis is essentially glomerular filtrate, which does not clear nitrogenous waste products. Severe hypothermia causes an initial relative central hypervolemia as a consequence of peripheral vasoconstriction. Cold diuresis may act as a volume regulator to diminish the vasoconstriction-induced capacitance vessel overload. Cold-water immersion can further increase urinary output by 3.5 times. Ethanol doubles that increase.20 Hypothermia initially stimulates respiration. This is followed by a progressive decrease in the respiratory minute volume. Carbon dioxide production decreases 50% with an 8° C fall in temperature. The normal stimuli for respiratory control are altered in severe hypothermia, and carbon dioxide retention with respiratory acidosis can occur. Hypercapnia increases core temperature cooling during snow burial.21 Predisposing factors that contribute to the pathophysiologic changes accompanying core temperature depression can be categorized as those that decrease heat production, increase heat loss, or impair thermoregulation (Box 140-1). Hypoglycemia with central neuroglycopenia also predisposes to hypothermia. Another cause of decreased heat production is malnutrition, which causes a decrease in subcutaneous fat. Severe malnutrition, as with marasmus, contributes to heat loss. Kwashiorkor is less commonly associated with hypothermia because of the insulating effect of the hypoproteinemic edema.11 Homeostatic capability progressively decreases with aging. Thermal perception is altered and elderly people manipulate the indoor ambient temperature less precisely. Most elderly patients are capable of normal thermoregulation but are prone to conditions, including immobility and systemic diseases, that interfere with heat production and conservation. Inability to sense cold, abnormal adaptive behavioral responses, and decreased peripheral blood flow reflect geriatric autonomic dysfunction.22 Ethanol is metabolized at a slower rate in hypothermic individuals and interacts with every putative thermoregulatory neurotransmitter. It may directly suppress the activity of the posterior hypothalamus and the mammillary bodies. Cutaneous heat loss increases through vasodilation, and shivering thermogenesis is decreased.23 Ethanol is the most common cause of excessive heat loss in urban settings.7,16 Intoxicated persons often lack protective adaptive behavior to avoid the cold. “Paradoxical undressing,” which is the removal of clothing in response to a cold stress, is common.24 Aging is associated with an increased sensitivity to the hypothermic actions of ethanol. Hypothermic alcoholic ketoacidosis also occurs. Hypothermia is common in patients with Wernicke’s encephalopathy. Hypothermia can mask the usual clinical triad of ophthalmoplegia, confusion, and truncal ataxia. Intravenous thiamine can be both diagnostic and therapeutic. In therapeutic or toxic doses, antidepressants, antimanic agents, antipsychotics, anxiolytics, and general anesthetics interfere with thermoregulation by impairing centrally mediated vasoconstriction. Overdosage of these medications and others (e.g., the organophosphates, heroin, glutethimide, and carbon monoxide) predisposes to hypothermia.25 Peripheral thermoregulatory failure classically occurs in neurogenic shock after acute spinal cord transection. The interruption of the autonomic nervous system eliminates vasoconstrictive control. The patient effectively becomes poikilothermic and can rapidly become hypothermic. Neuropathies and diabetes are additional peripheral causes of heat loss. An abnormal plasma osmolality may explain hypothalamic interference in uremia, lactic acidosis, diabetic ketoacidosis, and hypoglycemia.26 After trauma, hypotension and hypovolemia jeopardize thermostability.27 In patients with major injuries, a fall in core and skin temperature with no compensatory shivering thermogenesis occurs. Thermoregulation is impaired, and heat production decreases. Hypothermia may exacerbate blood loss by inducing a coagulopathy through three mechanisms: the coagulation cascade of enzymatic reactions is impaired, plasma fibrinolytic activity is enhanced, and platelets are sequestered and poorly functional.28 Hypothermia can protect the brain from ischemia only when it is induced before shock develops. This reduces adenosine triphosphate (ATP) use while the ATP stores are nearly normal. In traumatized patients, the ATP stores are already depleted.29 Appreciation of subtle presentations helps facilitate the early diagnosis of mild to moderate hypothermia. Vague symptoms include hunger, nausea, confusion, dizziness, chills, pruritus, and dyspnea (Box 140-2). During outdoor activities, individuals may simply become uncooperative, uncoordinated, moody, or apathetic. Indoors, elderly patients may exhibit confusion or simply become less communicative and display lassitude or a peculiar “flat” affect. Subtle progression of mental deterioration or motor skill impairment may mimic dementia. Symptoms such as slurred speech and ataxia may resemble symptoms of a cerebrovascular accident or intoxication.26 Some elderly people have a decreased ability to sense cold and thus fail to take appropriate adaptive action. The maladaptive phenomenon of paradoxical undressing is not uncommon.24 This last preterminal effort of the victim may be related to the peripheral vasoconstrictive changes of profound hypothermia. The patient can be mistaken for a victim of sexual assault. In urban settings, hypothermia is most commonly associated with ethanol ingestion or underlying illness. Other common causes include strokes, overdoses, psychiatric emergencies, and coexistent major trauma.16 No psychiatric disorder improves when the patient is cold. Mental status alterations include anxiety, perseveration, neurosis, and psychosis. Many individuals who are functional in temperate climates decompensate in colder weather. Hypothermia-induced psychiatric presentations and suicide attempts are commonly misdiagnosed.11 Blood gas analyzers warm blood to 37° C, which increases the partial pressure of dissolved gases. This results in an arterial blood gas report showing higher oxygen and carbon dioxide levels and a lower pH than the patient’s in vivo values.30–32 In fact, attempting to maintain a corrected pH at 7.4 and arterial partial pressure of carbon dioxide (PaCO2) at 40 mm Hg during hypothermia depresses cerebral and coronary blood flow and cardiac output and increases the incidence of VF.33 The ideal acid-base strategy is the ectothermic alpha-stat approach.10 Simply put, the goal is an uncorrected pH at 7.4 and PaCO2 at 40 mm Hg. Cold blood buffers poorly. In normothermia, when the PaCO2 increases 10 mm Hg, the pH decreases 0.08 unit. At 28° C, the decrease in pH doubles. Because the neutral point of water at 37° C is a pH of 6.8, the normal 0.6-unit pH offset between blood and intracellular water should be maintained at all temperatures (Fig. 140-3). Intracellular electrochemical neutrality ensures optimal enzymatic function at all temperatures.31 Relative alkalinity affords myocardial protection and improves the heart’s electrical stability.33 Carbogen could prove valuable in the treatment of accidental hypothermia because it flattens and shifts the oxyhemoglobin dissociation curve to the right. Frequent evaluation of serum electrolytes during rewarming is essential. There are no safe predictors of their values or trends.16 Changes occur in membrane permeability and in the sodium-potassium pump. The patient’s preexisting physiologic status, the severity and chronicity of hypothermia, and the method of rewarming alter the serum electrolyte values. The blood glucose level may also provide a subtle clue to the type of hypothermia. Acute hypothermia initially elevates blood glucose levels through catecholamine-induced glycogenolysis, diminished insulin release, and inhibition of cellular membrane glucose carrier systems. On the other hand, subacute and chronic hypothermia produce glycogen depletion, leading to hypoglycemia. Symptoms of hypoglycemia can be masked by hypothermia. A cold-induced renal glycosuria does not imply hyperglycemia or guarantee normoglycemia.26 Ischemic pancreatitis may result from the microcirculatory shock of hypothermia. The decreased pancreatic blood flow then activates proteolytic enzymes.7
Accidental Hypothermia
Perspective
Principles of Disease
Pathophysiology
Cardiovascular
Renal System
Respiratory System
Predisposing Factors
Decreased Heat Production
Increased Heat Loss
Impaired Thermoregulation
Traumatic Factors
Clinical Features
Diagnostic Strategies
Acid-Base Balance
Hematologic Evaluation

Full access? Get Clinical Tree


Accidental Hypothermia
Only gold members can continue reading. Log In or Register to continue