CHAPTER 68
Abnormal Uterine Bleeding and Menstrual Disorders
Winifred C. Connerton, PhD, CNM
The menstrual cycle begins with menarche between ages 12 and 15 years and ends with menopause between ages 45 and 55 years. The normal menstrual cycle is approximately 21 to 35 days in length, and will vary across a woman’s life span (usually shortening with age). Abnormal uterine bleeding (AUB) is any bleeding outside of the normal menstrual cycle, and it accounts for nearly one third of all visits to gynecologic providers annually. Disturbances to the timing and amount of uterine bleeding are multicausal, and vary in significance. For example, heavy uterine bleeding can indicate normal changes such as perimenopause, benign uterine growths such as fibroids, or life-threatening conditions such as endometrial cancer or ectopic pregnancy. Although AUB may have several potential causes, practitioners will find that many competing diagnoses are eliminated during the history taking. For example, bleeding preceded by regular molimina (premenstrual symptoms) will be very different than bleeding in the absence of such symptoms.
The average woman spends 30 to 43 years tracking, enduring, or otherwise living with her own version of the menstrual cycle. Each individual woman has her own experience, often with positive and negative aspects combined. Many women appreciate the regularity of their cycles, and view their menses as their body’s cleaning process or as an important aspect of their womanhood (Bushnell et al., 2010; Garside, Britten, & Stein, 2008; Geller, Harlow, & Bernstein, 1999). The menstrual cycle is a window into a woman’s underlying health, and the American Academy of Obstetricians and Gynecologists in conjunction with the American Academy of Pediatrics have stated that the menstrual cycle is a vital piece of health information, and consider it an additional vital sign (ACOG Committee on Adolescent Health care, 2006; Diaz, Laufer, & Breech, 2006).
Most women seek medical care for menses only when they experience a change in their bleeding. In the context of “usual bleeding” women may not recognize their personal menstrual experience as out of the norm, and consequently may not seek care for long-standing problems. Thus, an important question when beginning an evaluation of AUB is to ask “what is your normal pattern?”
The menstrual cycle is a self-perpetuating feedback loop of hormones generated by the hypothalamus, pituitary, and ovaries. Disruptions at any point in the cycle can lead to abnormal bleeding patterns. Understanding the cycle and associated symptoms can help practitioners identify the underlying cause. AUB causes include:
 Organic gynecologic conditions, both benign and malignant (e.g., reproductive tumors, infection, pregnancy complications)
Organic gynecologic conditions, both benign and malignant (e.g., reproductive tumors, infection, pregnancy complications)
 Systemic disease (e.g., hypothyroidism, hepatic disorders, diabetes, adrenal disorders, pituitary tumors)
Systemic disease (e.g., hypothyroidism, hepatic disorders, diabetes, adrenal disorders, pituitary tumors)
 Blood dyscrasias (e.g., thrombocytopenia, aplastic anemia, von Willebrand syndrome)
Blood dyscrasias (e.g., thrombocytopenia, aplastic anemia, von Willebrand syndrome)
 Iatrogenic causes (e.g., contraceptives, androgens, anabolic agents, hypothalamic depressants)
Iatrogenic causes (e.g., contraceptives, androgens, anabolic agents, hypothalamic depressants)
 Trauma (e.g., sexual assault, foreign bodies)
Trauma (e.g., sexual assault, foreign bodies)
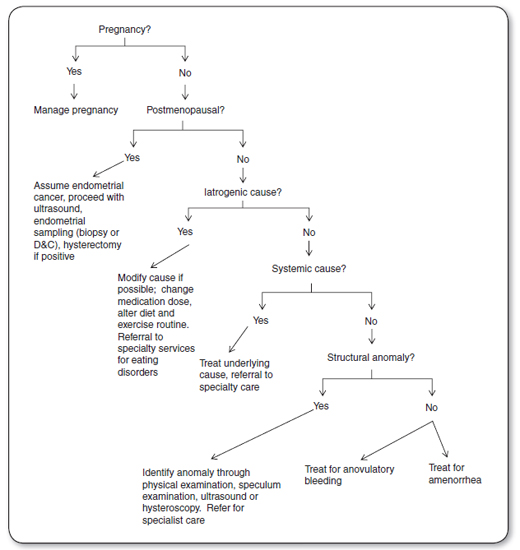
This chapter addresses AUB in the order in which a clinical assessment progresses, beginning with pregnancy, then iatro-genic causes, systemic causes, pelvic or genital tract abnormalities, and finally anovulatory bleeding (AB; also called dysfunctional uterine bleeding [DUB]) and amenorrhea. The process of diagnosis is achieved through history, and physical examination, augmented by laboratory tests and visualization. The investigative path is straightforward, and the findings from the history guide the physical examination and testing.
 ANATOMY AND PHYSIOLOGY
ANATOMY AND PHYSIOLOGY
Interaction between the pelvic anatomy and the brain determines the success or failure of the menstrual cycle. Making an accurate diagnosis of AUB requires an understanding of endocrine biochemistry, reproductive neuroendocrinology, the menstrual cycle and its unique phases, and the subsequent impact and response on different organ systems. What follows is an abbreviated description of the menstrual cycles. Readers interested in a more in-depth discussion of the biochemistry of menstruation will find more detail in a gynecological endocrine textbook (see References list).
The Normal Menstrual Cycle
The ovaries and the uterus each have unique phases within the menstrual cycle. The ovaries proceed through follicular, ovulatory, and luteal phases, while the uterus undergoes menstrual, proliferative, and secretory phases. The follicular phase typically lasts 10 to 14 days, although this is the most variable phase in the individual woman’s menstrual cycle. The follicular phase begins with a release of GnRH from the hypothalamus, which then triggers a release of FSH and some LH from the anterior pituitary. The rise in FSH prompts one to four follicles to develop. By the mid-follicular phase (days 5–7), a single follicle has matured for ovulation. This follicle begins secreting estrogen which works synergistically with FSH to stimulate the maturation of a single follicle. By day 9 FSH causes LH receptors on the follicle to multiply in preparation for an LH surge that will cause ovulation. Concurrent with the follicular phase of the ovary, the uterus enters the proliferative phase, having shed its lining in menstruation as a result of a loss of hormonal support in the previous cycle. By day 7, rising estrogen levels are sufficient to influence secretory changes on the endometrium, and by midcycle, the lining is 5 to 10 times its original size (Fritz & Speroff, 2011).
Ovulation occurs approximately 10 to 12 hours after a surge in LH. After ovulation the luteal phase begins, and the preovulatory follicle becomes the corpus luteum. The length of the luteal phase is between 11 and 17 days. The corpus luteum becomes a significant source of estrogen and progesterone under the ongoing influence of LH with a peak in progesterone production by days 22 to 23. In the absence of implantation, the corpus luteum develops into the corpus albicans and begins a rapid breakdown. As it undergoes slow atresia, LH production diminishes, along with estrogen and progesterone production.
The uterus enters the secretory phase during the ovary’s luteal phase. Under the influence of progesterone, cell reorganization produces mucus-secreting glands, increased arterial flow into the lining, and numerous thick cell layers. The loss of hormonal support induces both immunoreactive changes and rhythmic vasoconstriction of the spiral arteries within the endometrium. In a normal menstrual cycle, this process results in an orderly separation of the outer layer of the endometrium, and bleeding ensues. The fall in progesterone exerts a positive effect on GnRH, and another cycle begins (Fritz & Speroff, 2011).
Pathophysiology of AUB—Anovulation
AUB can manifest in several different ways, from profuse, frequent bleeding, to a complete absence of bleeding. Causes for AUB are varied and include disturbances in the hypo-thalamus-pituitary-ovarian axis, mechanical disruption in the reproductive tract, and sometimes are the result of an unrelated systemic problem (such as a clotting disorder or liver disease).
Any disruption of the steps in the hypothalamic–pituitary–ovarian axis can lead to anovulation and AUB. For example, estrogen is essential to follicle maturation for ovulation, but in too high levels estrogen inhibits FSH, yet in too low levels LH is not produced (Fritz & Speroff, 2011). Systemic disease, stress, abrupt weight fluctuations, body-fat composition, ovarian disease, infection, or medications can induce changes that are crucial in the maturation of a follicle. In the case of obesity, extraovarian production of estrogens from androgens in adipose tissue act on the feedback mechanisms in the hypothalamus and pituitary, shutting off FSH prematurely and condemning developing follicles to atresia. Alternatively, in the case of the female athlete, ongoing exercise depletes the “energy state” of the body and disrupts the pulsatile production of GnRH, FSH, and LH necessary for follicle maturation and ovulation (Nattiv et al., 2007; Warren, 1999).
When a primary follicle fails to emerge despite ongoing recruitment of primordial follicles, the subsequent absence of progesterone production then prevents ovulation. Anovulation results in chronic stimulation of the endometrium as a result of unopposed estrogen. Endometrial thickening under the influence of estrogen causes its supportive base to become less adhesive. As a result, the endometrium may begin to slough off in an incomplete and irregular fashion, or in a prolonged, profuse pattern. Without treatment, exposure to unopposed estrogen can cause endometrial hyperplasia and neoplasm.
 EPIDEMIOLOGY
EPIDEMIOLOGY
AUB is estimated to affect 11% to 13% of reproductive-age women, and accounts for one of the most common gynecologic complaints seen in outpatient clinics (Hartman et al., 2013). The prevalence of AUB increases with age, though specific causes of AUB (particularly AB) are more common at the age extremities of the menstrual cycle: menarche and menopause. Approximately half of all women presenting with AUB have no underlying cause (Fraser, Langham, & Uhl-Hochgraeber, 2009). In 2000, approximately 633,000 hysterectomies were performed, of these 90% were performed for AUB and other non-life-threatening reasons (Kuppermann et al., 2004).
AUB can make a serious impact on all aspects of women’s lives, through lost work, medical treatment, social isolation, and the cost of menstrual supplies. One study estimated the direct and indirect costs of AUB treatment to be upward of $1.55 billion annually, not accounting for personal costs to individual women (Liu, Doan, Blumenthal, & Dubois, 2007). Other studies have noted significant loss of work time due to heavy uterine bleeding, accounting for over 3 weeks of work lost per year, at an estimated $1,692 lost annual wages (Côté, Jacobs, & Cumming, 2002). Women with AUB have significantly lower scores on all quality of life domains in measures of health-related quality of life (Fraser et al., 2009).
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
The diagnostic approach to AUB includes a detailed history and physical examination, followed by appropriate diagnostic tests. Abnormal bleeding can be a sign of endometrial cancer, thus it is important to maintain a high index of suspicion in women at risk for endometrial cancer. Figure 68.1 details the diagnostic progression that moves from pregnancy to the final diagnoses of AB and amenorrhea.
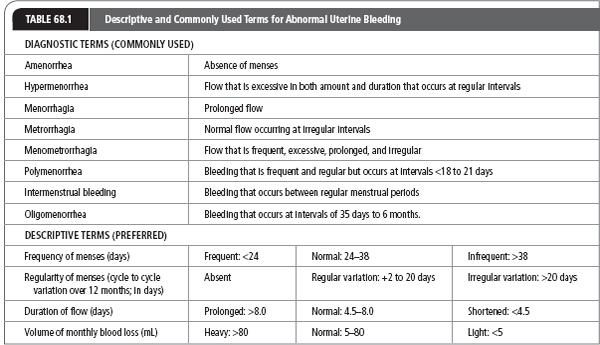
The language of abnormal bleeding is often a source of confusion, with some terms used as both descriptors and diagnoses (such as DUB and menorrhagia), and considerable overlap between the terms. There is an international movement to standardize the terms used with AUB to focus more on description of the woman’s actual experience, rather than less exact or descriptive phrases (Dueholm, 2008; Fraser, Critchley, Munro, & Broder, 2007; Fraser, Critchley, & Munro, 2007). The description of bleeding should include: menses frequency, regularity, duration, and volume. Table 68.1 includes the older, less-exact terms for reference as these are still widely used, as well as the more accurate descriptive terms.
 HISTORY AND PHYSICAL EXAMINATION
HISTORY AND PHYSICAL EXAMINATION
AUB can present as acute hemorrhage with several different causes. In the event of acute bleeding with changes in vital signs, immediate transfer to an acute care setting is mandatory.
History
The history should include the woman’s age, age at menarche, and a thorough history of menses (flow pattern, frequency, and duration). The patient should be questioned about any associated symptoms she experiences with menses or any abnormal bleeding, including molimina (premenstrual syndrome, premenstrual breast tenderness, bloating, and cramps).
When eliciting descriptions of the bleeding investigate descriptions of “heavy” or “normal” because these quantities are very personal. Ask about clots, numbers of tampons or pads used (or if used in combination), over what period of time, and any associated symptoms such as cramping or severe abdominal pain. Also inquire about the impact of this bleeding on the patient’s life. Is she able to go to work on the heaviest days, does she stay at home to manage the flow? It is important to note that only approximately 50% of women reporting heavy menstrual bleeding meet the criteria for menorrhagia (>80 mL loss; Bongers, Mol, & Brölmann, 2004). Women’s subjective experience of AUB is important, thus women who do not meet the diagnostic criteria for menorrhagia may still require treatment to manage their experience of heavy menstrual bleeding.
Obtain a pregnancy and sexual history and inquire about contraceptive use. The patient should be asked if she has experienced violence, or sexual assault. Other historical data that should be obtained from the patient and the medical record should include a history of gynecologic problems, including infections and sexually transmitted infections. A surgical history should include an inquiry into whether the patient has experienced excessive bleeding after operative procedures. The family history should be reviewed with a focus on gynecologic conditions, including endometrial cancer, prolonged bleeding, or a family history of heavy menses. Medication use should be carefully reviewed. The patient’s use of contraceptives, hormonal treatments, recreational drugs, prescription drugs, antiretroviral, nonsteroidal anti-inflammatory drugs (NSAIDs), and vitamins and other over-the-counter drugs or complementary therapies should all be evaluated as possible factors in the abnormal bleeding pattern.
Other lifestyle factors that can help inform the differential diagnosis include exercise patterns; alcohol, caffeine, and tobacco use; and stress management and coping mechanisms.
Physical Examination
A thorough physical examination with careful overall visual inspection reveals many clues to the diagnosis. Height, weight, and body mass index (BMI) calculation begin the assessment. Note signs of hyperandrogenic disorders such as intensified hair growth on the upper lip, chin, cheeks, and chest and from the pubic crest to the umbilicus. Scalp hair may exhibit asymmetric or patchy balding (alopecia). Acne may be present on the face as well as the back, and skin may be excessively oily. Signs of anemia include pale skin, and slow capillary refill. Palpation of the neck may reveal an enlarged thyroid, suggesting a thyroid disorder. Breast examination is performed to rule out galactorrhea which is a sign of a pituitary tumor in a nonlactating woman.
 DIAGNOSIS
DIAGNOSIS
Diagnosis of the underlying cause of AUB is made through a combination of serologic tests, tissue sampling, and visualization. The combination of tests is chosen after the history and physical examination to complete the diagnosis. See Table 68.2 for a list of laboratory and visualization examinations for specific diagnoses.
Endometrial Biopsy
Several office procedures can aid in the task of finding a cause for AUB, and are essential in the diagnosis of endometrial cancer. Endometrial biopsy is used to evaluate the endometrium when the woman has risk factors for endometrial hyperplasia (patients with breakthrough bleeding while receiving hormone replacement therapy, AB in patients older than 40, or in patients older than 35 with risk factors for endometrial cancer such as obesity, hypertension, and family history).
Diagnostic Tests for AUB |
TEST | DIFFERENTIAL DIAGNOSIS |
Pregnancy test (β-HCG) | Diagnose pregnancy related bleeding |
CBC, including MCV, MCH | Identify anemia |
Wet prep | Cervicitis, bacterial vaginosis |
STI screening | Evaluate for cervicitis and PID |
TSH, free T4 | Thyroid function |
FSH, LH, and prolactin | Endocrine disorder |
Pap smear, colposcopy | Cervical neoplasm |
Ultrasound | For identification of uterine or ectopic pregnancy, structural abnormalities |
Ristocetin cofactor assay | Von Willebrand disease |
Endometrial biopsy | Uterine pathology |
Liver function tests | Liver disease |
Renal function tests | Kidney disease |
CBC with platelet count and coagulation studies | Coagulopathy |

Full access? Get Clinical Tree