Fig. 3.1
The four scanning windows of the E-FAST abdominal examination
Recent bleeding is represented by an anechoic “dark line” in these spaces, yet older blood may have a heterogeneous echogenicity owing to clots.
Attaining E-FAST views requires basic knowledge of ultrasound physics and knobology of ultrasound machines. We prefer the use of curved probes with a frequency between 3 and 5 MHz. Optimal depth settings will depend on patient body habitus, but a setting of 8–15 cm is usually sufficient. Adjust gain settings in a way that blood vessels are black and the surrounding tissues are not too bright. Hold the probe like you hold a pen or a pencil. Grasp it with the first three fingers of the dominant hand, and use the remaining fingers to stabilize the probe touching the patient if needed avoiding inadequate pressure. Do not forget the basic transducer movements known as ART (alignment for sliding movements, rotation, and tilting).
The patient must be in a supine position, and the operator should stand to the right.
According to international ultrasound consensus, the transverse view of our patients is a perspective from the feet (Fig. 3.2). Therefore, the images on the right of the patient should show on the left of the monitor. The sagittal and coronal views also corresponds to an image on the left of the monitor which corresponds to the cranial direction (Fig. 3.3). The scanning probe has a marker on the probe which helps keep the proper orientation as referred. One can also assure this by pressing on the surface of the probe’s marker just to guarantee its correct position by viewing movement on the left side of the monitor. All obtained ultrasound images should be correlated with the clinical situation. Please remember that this type of ultrasound is more focused on a clinical basis rather than the traditional anatomically oriented ultrasound that is performed in the radiology unit.
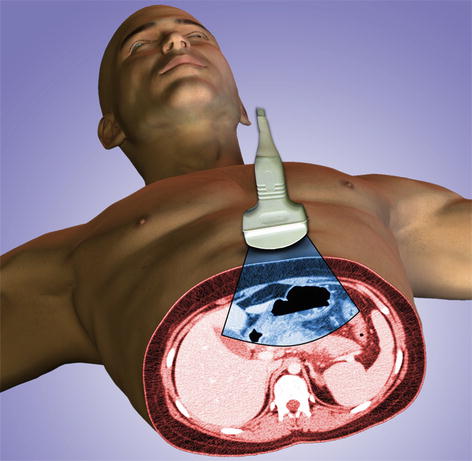
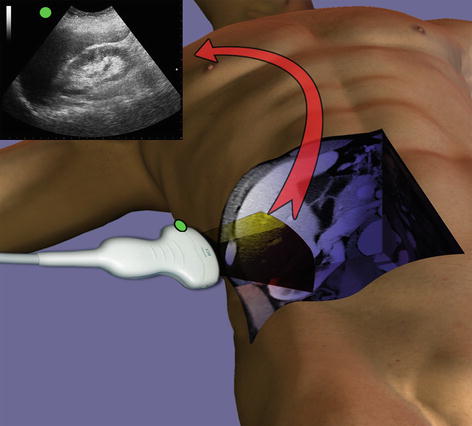
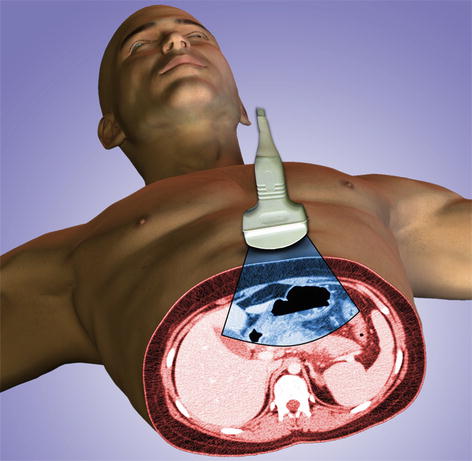
Fig. 3.2
The ultrasound transverse caudal to cranial view
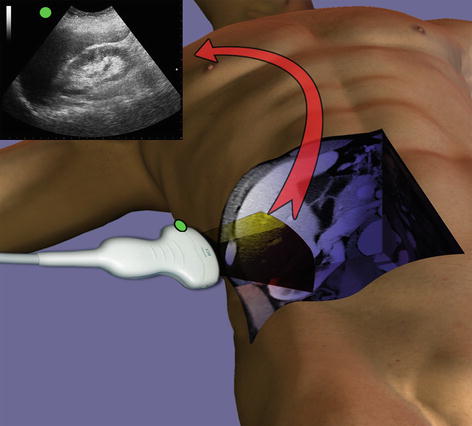
Fig. 3.3
Green marker pointing toward the patient’s head in coronal view
3.2.2 Normal Anatomy
The order of the E-FAST views is not standardized although many surgeons argue that in cases of thoracic trauma, one should begin with a pericardial view. The perihepatic view may first be performed in abdominal trauma since it is where blood primarily deposits in the peritoneum.
Pericardial View
The subcostal view is also known as subxiphoid; this permits the visualization of the heart as well as part of the liver and diaphragm. Usually, a very small amount of physiological fluid exists between the parietal and visceral pericardium that is non-circumferential and that is rarely seen. The probe should be placed with the pointer directed toward the patient’s right. The convex surface of ultrasound probe should be placed in the midline, angled slightly upward toward the left shoulder, and insinuated under the ribcage to minimize thoracic ribcage shadow, until a view of the heart and left lobe of the liver is obtained (Fig. 3.4). Normal pericardium is seen as a hyperechoic (white) line surrounding the heart below the left lobe of the liver (Figs. 3.5 and 3.6). To enhance imaging ask the patient to bend his knees and hold his breath or make an end–inspiratory pause if on mechanical ventilation. The intercostal or parasternal view is also a valid option if the subcostal view is not adequate owing to obesity, protuberant abdomen, abdominal tenderness, and gas or epigastric lesions.

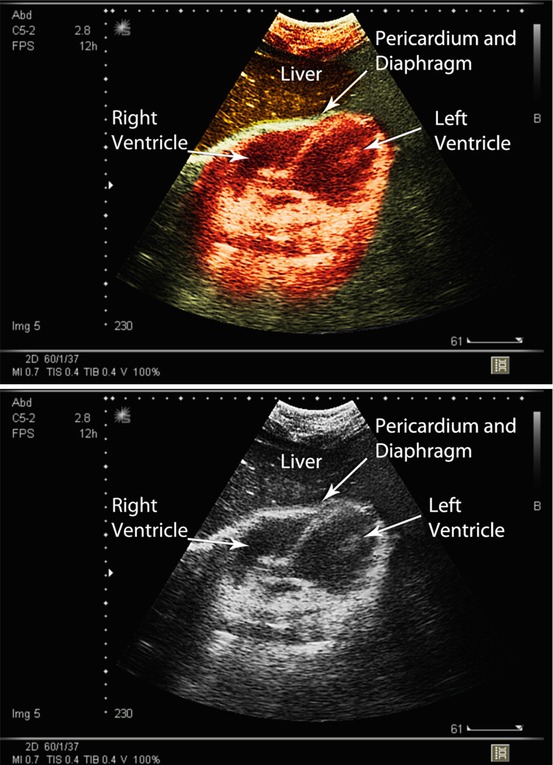

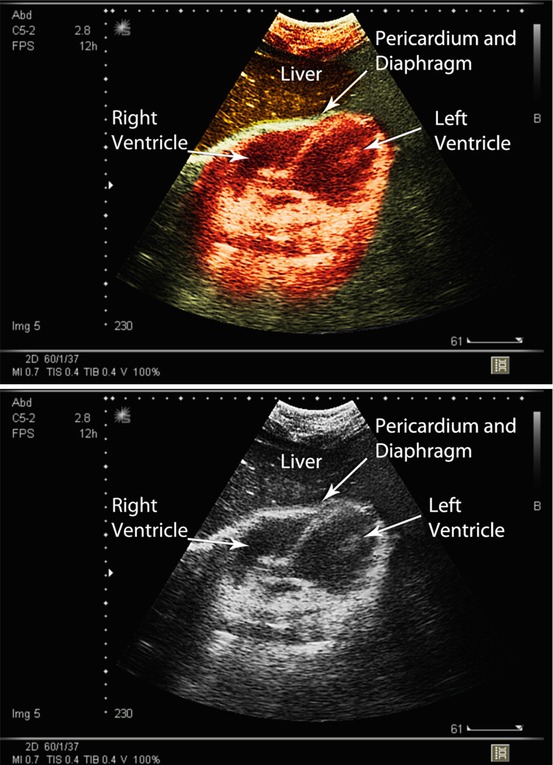
Fig. 3.4
Position for pericardial subxiphoid view
Figs. 3.5 and 3.6
Normal subcostal echocardiographic view
Perihepatic View
The perihepatic or right upper quadrant view permits the surgeon to acquire a partial image of the liver, the right kidney, the subphrenic space, and the right pleural space. The right subcostal technique is obtained with the probe at the right infracostal margin, just lateral to the midclavicular line (Fig. 3.7). Angle the probe until the hepatorenal space (Morison’s pouch) is seen. In a normal view, the liver and kidney are closely aligned separated by a brightly echogenic surface (Gerota’s fascia) (Figs. 3.8 and 3.9). To better visualize the subphrenic space, one should gradually move the probe in a more cranial direction and laterally closer to the posterior clavicular line allowing for a more coronal perspective. Right intercostal oblique or transverse views can be obtained rotating the probe counterclockwise (Fig. 3.10). This allows a better visualization of the right pleural space, Morison’s pouch, and right paracolic gutter. As mentioned, to enhance imaging, have the patient hold his breath or make an end–inspiratory pause if on mechanical ventilation.
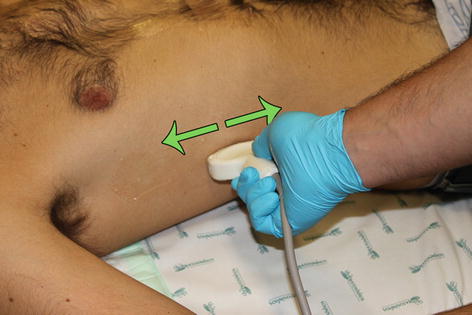
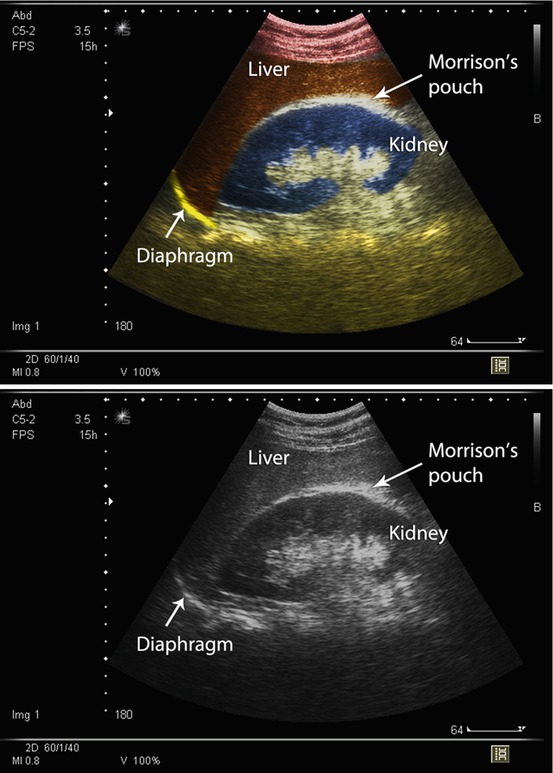

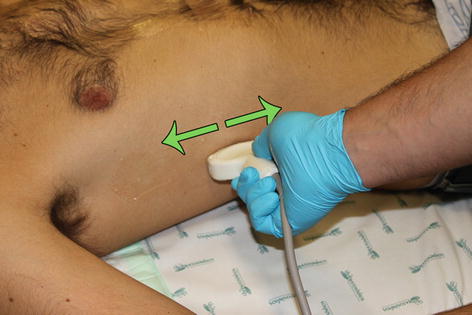
Fig. 3.7
Position for perihepatic E-FAST view
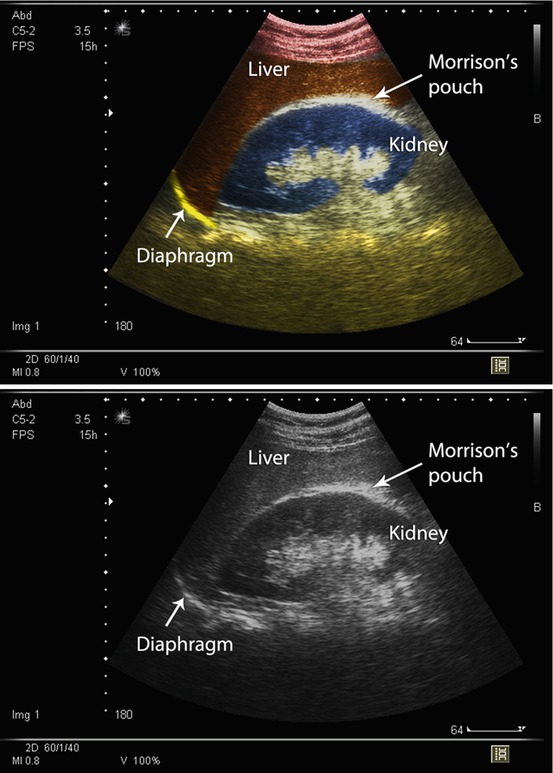
Figs. 3.8 and 3.9
Normal view of hepatorenal interface

Fig. 3.10
Probe rotation for intercostal view
Perisplenic View
The perisplenic or left upper quadrant view may be considered more challenging since the spleen is smaller and located more posteriorly than the liver. This approach requires that the placement of the probe be intercostal and as close to the posterior axillary line as possible between the 10th and 11th ribs angled to achieve a view of the spleen, the left kidney, the subphrenic space, and the left pleural space (Figs. 3.11, 3.12, and 3.13). The spleen has a homogeneous cortex that is more echogenic than the left kidney cortex. To better visualize the subphrenic space, one should position the probe marker upward pointing toward the left posterior axilla and gradually move the probe in a more cranial direction laterally closer to the posterior clavicular line allowing for a more coronal perspective.









