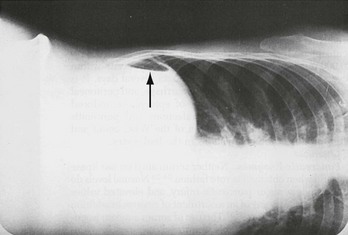
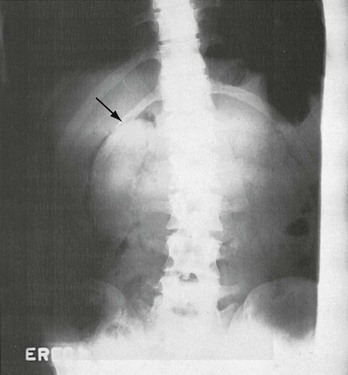
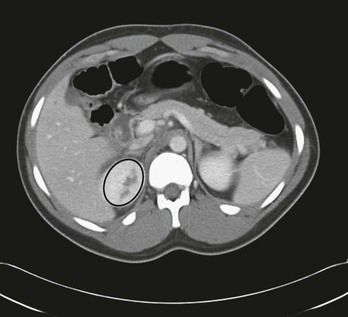
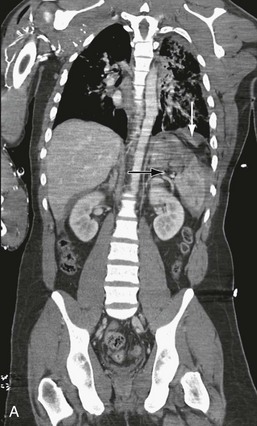
Chapter 46 The management of abdominal trauma should be approached in an organized, vigilant, and knowledgeable manner. Reliance on key clinical features and the timely use of diagnostic procedures tremendously alter morbidity and mortality. Advancements in imaging have helped to decrease missed or delayed diagnoses, yet they remain the most serious pitfalls in the management of abdominal injuries.1 Whether by accident or intention, penetrating trauma can result from a wide variety of weapons or instruments, and certain elements of therapy vary accordingly. The management of patients with penetrating trauma has changed dramatically since 1960, when Shaftan introduced the concept of selective laparotomy and serial observations.2 Before that time, surgery was mandatory. The careful integration of physical examination and certain diagnostic procedures, notably local wound exploration (LWE), ultrasonography, computed tomography (CT), laparoscopy, and in rare instances, diagnostic peritoneal lavage (DPL), now provides the emergency physician and trauma surgeon with an accurate means of determining whether laparotomy should be undertaken. The approach varies according to the clinical status of the patient, the instrument responsible for injury, and the site of penetration. Nonoperative management has gained favor predominantly for stab wounds, though also for carefully selected gunshot wounds (GSWs), with the intent to reduce the incidence of and morbidity from nontherapeutic laparotomies.3,4 Wounds from stabbing implements occur nearly three times more often than wounds from firearms, but the latter have a significantly greater mortality rate and are responsible for 90% of penetrating trauma mortality.5 The small intestine, colon, and liver are, successively, the most likely organs to sustain injury after penetrating trauma.5 The highest risk of death from penetrating abdominal injury occurs among African Americans in the 15- to 34-year-old age range, followed by Hispanic persons in that same age group. The rate for non-Hispanic whites is greatest at 75 years of age and older. The predominant intent is homicide among African Americans and suicide among non-Hispanic whites.6 The use of firearms in the United States contributes heavily to the morbidity and mortality of trauma. The current U.S. civilian population is the most heavily armed in history. Over 42 million U.S. households have firearms, and there are more than 57 million gun owners.7 The number of homicides committed with firearms exceeds the number of homicides resulting from all other forms of violence combined. More than 850,000 American civilians were killed by bullets in the 20th century, and mortality from GSWs accounts for 12 per 100,000 deaths in urban areas.8 The automobile is the major cause of blunt abdominal trauma (BAT). Motor vehicle collisions (MVCs) and auto-pedestrian crashes have been cited as causes in 50 to 75% of cases, blows to the abdomen in approximately 15% of cases, and falls in 6 to 9%.9 Each year in this country, trauma results in approximately 22,000 deaths and accounts for $160 billion of health care expenditures for children to the age of 16 years. Nearly 13% of children admitted to pediatric trauma centers are proven to have abdominal injury, and this category follows only head, neck, and thoracic trauma as the cause of injury-related death.10 Blunt mechanism causes approximately 85% of pediatric injury, although penetrating violence is becoming a greater concern. As is true with adults, MVCs are responsible for most of the morbidity and mortality in cases of trauma in children.8 Auto-pedestrian accidents and falls out of cars cause a significant percentage of these injuries. The abdominal cavity and its contents can be reached not only through the anterior abdominal wall and lower chest but also through the flank, back, and buttocks. Missiles can also lodge intraperitoneally after traversing proximal extremities. The anterior abdomen is defined as that region between the anterior axillary lines from the anterior costal margins to the groin creases. The low chest begins at the nipple line or fourth intercostal space anteriorly and the inferior scapular tip or seventh intercostal space posteriorly, and then extends down to the inferior costal margins. The flank is between the anterior and posterior axillary lines bilaterally from the inferior scapular tip to the iliac crest. The back is between the posterior axillary lines, beginning at the inferior scapular tip and extending down to the iliac crest. The intraperitoneal cavity is vulnerable when penetration occurs as high as the fourth intercostal space anteriorly and the sixth or seventh laterally and posteriorly because the diaphragm can ascend to this level during expiration. Likewise, simultaneous thoracic abdominal penetration has been found in 20 to 40% of cases of abdominal thoracic trauma.11 Scrutiny of entrance and exit sites, as well as wound tracts, is imperative. The liver, followed by the small bowel, is the organ most often damaged by stab wounds, in keeping with the surface area each of these structures presents.4 The frequency of organ injury caused by GSWs is greatest for small bowel, followed by the colon and then the liver.5 Typically, multiple organ injuries are sustained, notably perforations to bowel. This same pattern is seen in the pediatric patient. Stab Wounds.: Knives are not the sole implements used in stabbings. Ice picks, pens, coat hangers, screwdrivers, and broken bottles, to name a few, have been used by assailants. Stab wounds of the abdomen occur most commonly in the upper quadrants, the left more commonly than the right. They are multiple in 20% of cases and involve the chest in up to 10% of cases. Most stab wounds do not cause an intraperitoneal injury, and the incidence varies with the direction of entry into the peritoneal cavity. Anterior stab wounds penetrate the peritoneum in approximately 70% of cases but inflict a visceral injury in only half of these.4 Left lower chest wounds are associated with a 17% incidence of intraperitoneal damage in addition to the expected high rate of thoracic and diaphragmatic injuries. Right lower chest wounds have a much lower incidence of 0% to 4%.12 Abdominal entries from the flank and back have reported incidences of up to 44% and 15%, respectively.13,14 The organ injured cannot be well predicted by the site of entry in the abdominal wall. The liver and spleen are the viscera most commonly damaged in cases of back and flank wounds. Gunshot Wounds—Ballistics.: The science of ballistics is complex, but a few basic principles are helpful in understanding the pathophysiologic processes of these injuries. The magnitude of the injury is proportional to the amount of kinetic energy imparted by the bullet to the victim, according to the following equation: where E is the kinetic energy (in foot-pounds), m is the mass of the bullet, v is the velocity of the bullet (in ft/s), and g is gravitational acceleration (in ft/s). In other words, the degree of injury depends on the mass of the bullet and the square of its velocity.15 Additional factors that affect injury created by a missile include the resistance and viscoelastic properties of the tissue through which it passes, as well as the stability of the missile in this medium. Missile velocities are categorized as low (slower than 1100 ft/s), medium (1100-2000 ft/s), and high (faster than 2000-2500 ft/s); the impact velocity is the most important determinant of wounding capability. The impact velocity depends on the distance between the firearm and the victim, the muzzle velocity, and various characteristics of the missile. At medium and high velocities, the missile has an explosive effect and creates a temporary passage in the tissue along its course. The size of this passage is directly proportional to the specific gravity of the penetrated tissue. This sudden formation of a tract displaces nearby organs and vascular structures, and bone and viscera may be fractured or torn without being directly struck by the missile. Several cases of an intraperitoneal injury caused by a bullet that remained extraperitoneal throughout its entire course have been reported.16 Solid viscera, such as the liver and spleen, are more vulnerable to this effect. High-Velocity Missiles.: Wounds from high-velocity missiles involve additional problems. First, external contaminants tend to be dragged into the wound. Second, the closure of the tract immediately after the bullet’s passage may lead to an underestimation of tissue damage. Finally, high-velocity bullets can fragment internally. In fact, a missile at any velocity can fragment after contact with bone and cause additional multiple trajectories and injuries. Civilian wounds have usually resulted from low-velocity handguns, but unfortunately a trend toward more destructive weapons, such as the .38 and .357, may be occurring. Shotgun Wounds.: The shotgun was designed to strike a small, fast-moving target at close range. Because of the ballistic shape of the individual pellets, a rapid falloff in velocity occurs, making this weapon ineffective in producing severe wounds at long distances. An initial muzzle velocity of 1300 ft/s drops to 950 ft/s within 20 yards, a decrease of 25%. At close range (<15 yards), however, the shotgun is extremely lethal. Shotgun wounds have been previously classified in three groups according to the range and pattern of distribution. More recently, classification has been according to the pattern of injury on the victim. Based on distance from the weapon to the victim, type I wounds involve a long range (>7 yards) and a penetration of subcutaneous tissue and deep fascia only. Type II wounds occur at a distance of 3 to 7 yards and may create a large number of perforated structures. Type III wounds occur at point-blank range (<3 yards) and involve a massive destruction of tissue. When categorized by pattern, type I wounds produce a spread greater than 25 cm in diameter; type II, 10 to 25 cm in diameter; and type III, less than 10 cm in diameter.17 The tissue damage is proportional to the specific gravity and inversely proportional to the elastic properties of the affected organ. Thus the liver is more vulnerable than the lungs to this injury. Close-range shotgun wounds, in addition to the shot, force external contaminants (e.g., clothing and parts of the shell wadding) into the wounds. Type III wounds carry a substantial mortality risk. Seatbelt Injuries.: Unrestrained front and rear seat passengers are at unequivocally greater risk of intra-abdominal injury than their restrained counterparts.18 The three-point shoulder-lap belt is the most effective restraining system and is associated with the lowest incidence of abdominal injuries, compared with older systems. However, abdominal injuries are still ascribed to combined shoulder-lap and lap-belt systems. The shoulder belt component can lead to right-sided and left-sided rib fractures for the driver and front seat passenger, respectively, with potential for injury to underlying abdominal viscera. Improper underarm usage of the shoulder belt increases compressive forces to the upper abdomen, particularly in the event of a front-end crash. Clinically, two symptom patterns emerge. Approximately one fourth of these patients develop evidence of a hemoperitoneum secondary to mesenteric lacerations. In the remainder, the intestinal injury most commonly involves the jejunum, and the initial signs and symptoms are often absent or considered insignificant. Subsequent delays in diagnosis of up to 8 weeks have rarely been reported. The “seatbelt sign,” contusion or abrasion across the lower abdomen, is found in less than one third of patients with abdominal injuries caused by lap belts. Its presence, however, is highly correlated with intraperitoneal pathologic lesions.19 Rupture of the diaphragm can also occur. Rare cases of acute abdominal aortic dissection with incomplete or complete occlusion have also been described, and injuries to the lumbar spine are not uncommon.20 Iatrogenic Injuries.: Although well intentioned, diagnostic and therapeutic efforts in patient care are not risk-free. Abdominal injuries may be sequelae of various medical procedures and in certain instances not only are extremely difficult to recognize but may contribute to or cause pronounced morbidity or death. Numerous procedures may cause an iatrogenic injury. Artificial ventilation can lead to gastric distention, particularly in children. Besides compromising ventilation and increasing the risk of vomiting and aspiration, a significant distention may lead to an esophageal or gastric laceration and perforation. These may occur with bag-mask ventilations, an inadvertent esophageal intubation with a nasotracheal or endotracheal tube, or the mistaken connection of the nasogastric tube to oxygen rather than suction. Esophageal, gastroesophageal junction, and gastric lacerations are evidenced by bloody emesis or nasogastric return. If a gastric perforation occurs and positive-pressure breathing is maintained, a tension pneumoperitoneum or abdominal compartment syndrome may ensue with inferior vena cava compression and decreased cardiac output. External cardiac compressions have produced splenic, hepatic, and gastric injuries. Manual thrusts to clear an airway obstruction, as taught in basic life support courses, and the Heimlich maneuver have caused rib fractures with lacerations and the rupture of abdominal viscera. In cases of a cardiac arrest, these injuries may be occult but life-threatening. If hypotension occurs after cardiopulmonary resuscitation, an abdominal injury and hemorrhage are considered along with cardiogenic shock.21 A liver biopsy can lead to a hemoperitoneum or hemobilia. Endoscopic procedures of the bowel may cause a hollow viscus perforation and peritonitis, particularly when a biopsy is performed, although they can result from rapid retraction of the endoscope without biopsy, as well.22 Peritoneoscopy has been reported to cause small bowel perforations and iliac vessel lacerations. Barium enemas have an extremely low incidence of perforation but can be another cause of unexplained peritonitis and pneumoperitoneum. Stab Wounds.: It is helpful to obtain information regarding the mode of injury from the patient, paramedic, or witnesses. The number of stabs inflicted, type and size of the instrument, posture of the victim relative to the direction of assault, estimated blood loss at the scene, time of injury, and response to fluids should be sought. However, a significant proportion of victims of stab wounds are found under the influence of alcohol or another drug. This state can make obtaining an accurate history a futile effort and further compromises the validity of symptoms and signs. Gunshot Wounds.: As initial stabilization measures are instituted in the emergency department, the emergency physician can elicit certain facts that can contribute greatly to the evaluation of the patient. These include the weapon used, its distance from the victim when shot, the position of the victim in relationship to the weapon when fired, the suspected number of shots, the blood loss at the scene, the amount and type of field fluids administered, and the vital signs during the prehospital course. Hypotension in the acute stage results from hemorrhage that is most often from a solid visceral or vascular injury. Traumatic pancreatitis may produce significant third-space fluid loss, but hours to days are usually required for this to appear, and shock is an uncommon presentation.23 When hypotension accompanies significant multiple blunt trauma and is unexplained, one should assume the presence of intraperitoneal hemorrhage until it is excluded. However, a known extra-abdominal source of hemorrhage does not mitigate the need to evaluate the peritoneal cavity. A head injury alone does not explain shock except in cases of profound head injury or in the very small infant, in whom traumatic intracranial or extracranial (e.g., cephalohematoma) blood loss may be proportionally substantial.24 Palpation elicits local or generalized tenderness in approximately 90% of alert patients with an intra-abdominal visceral injury. Local and generalized rebound tenderness and rigidity can be signs of peritoneal irritation and occur less commonly. These signs lack specificity, however, and can be found with lower rib fractures and contusions of the thoracoabdominal wall. These findings or, more important, their absence, are more reliable in alert patients. However, false-positive and false-negative abdominal manifestations have been well demonstrated even in conscious, responsive patients.25,26 A rectal examination rarely reveals blood or subcutaneous emphysema, but the presence of either is highly correlated with abdominal injuries. The rectal examination is now considered less helpful than clinical indicators such as blood at the meatus or scrotal hematoma in urethral injuries, or evidence of paralysis. The rectal examination can be eliminated or deferred in many patients, as the clinical indicators noted earlier appear to be more sensitive than the rectal examination.27–29 Notable exceptions may include suspected cauda equina syndrome or penetrating trauma to the perirectal area. Stab Wounds.: Serial physical examinations performed by the same observer are gaining acceptance in certain centers where these have been found useful, particularly with patients who are alert, communicative, and neurologically intact. The presence of intoxicants does not necessarily preclude reliance on examination but may undermine its value.30 In other series, patients with impressive physical findings after penetrating trauma to the abdomen have undergone exploratory laparotomy, with negative results in 14 to 28% of cases.31 Moreover, up to one third of patients with significant intra-abdominal injuries have no suggestive physical signs, particularly when a retroperitoneal injury has occurred.32 Therefore serial clinical evaluations typically involve physical examinations to include trending of vital signs, laboratory testing including serial hemoglobin measurement, and repeated focused assessment with sonography in trauma (FAST) examinations. Gunshot Wounds.: As with blunt or other modes of penetrating trauma, there is dispute regarding the value of the physical examination of patients with abdominal GSWs. In various series, 20% of patients with a documented intraperitoneal injury had no peritoneal signs before exploration.32 Moreover, objective physical findings suggestive of intra-abdominal damage have been misleading and falsely positive in 15% of patients in whom laparotomy revealed no injury. Other authors contend that selective management can be undertaken safely when physical examination is the fundamental evaluative measure.30 Overall, the accuracy of the physical examination in patients with BAT is 55 to 65%.25 The initial presentation may be exceptionally benign in cases of blunt intra-abdominal injury. The most reliable symptoms and signs in alert patients are pain, tenderness, and peritoneal findings, particularly when risk factors for abdominal injury are present. When altered sensorium intercedes, the physical signs become less reliable. Frequent evaluations by the same examiner are indicated even in alert patients, but especially in sensorium-altered patients, particularly as their mental status and sensorium normalize. Hematologic and chemical values are of limited use in the management of the acutely traumatized patient.33 They should be considered adjuncts to diagnosis and not substitutes for clinical assessment. Hematocrit.: The hematocrit reflects baseline value, extent of and time from hemorrhage, exogenous fluid administration, and endogenous plasma refill. The last of these is a physiologic compensatory shift of extracellular fluid into the intravascular space, the intent of which is to restore the original blood volume. Based on a study of volunteers sustaining a 10 to 20% blood loss, this restoration proceeds at a rate of only 40 to 90 mL/hr for the first 10 hours and requires 30 to 40 hours for completion.34 However, patients evidencing hemorrhagic shock with a blood loss of at least 40% demonstrate much faster plasma refill rates, estimated as high as 1500 mL in the first 90 minutes after injury, with significant decreases in hematocrit within this period. Although the hematocrit is an easily acquired measure, it is often a conundrum when viewed in isolation, and serial determinations are more helpful. White Blood Cell Count.: The white blood cell (WBC) count has little discriminatory value in cases of abdominal trauma, particularly its acute phase.33 The WBC count may be normal or may show a modest leukocytosis (12,000 to 20,000/mm3 with or without left shift), which can occur in the setting of multisystem trauma as a result of stress-induced demargination in the absence of any intra-abdominal process, or as a result of tissue injury, acute hemorrhage, or peritoneal irritation. Pancreatic Enzymes.: Neither serum amylase nor lipase is useful in the evaluation of acute abdominal trauma. Normal levels do not exclude a major pancreatic injury, and elevated values may be caused by any of an assortment of reasons in addition to an injured pancreas. The use of serum amylase isoenzymes has not appreciably improved accuracy. Nontraumatic causes of hyperamylasemia include several diseases and the use of alcohol, opioids, and various other drugs. Amylase or lipase may also be elevated with pancreatic ischemia produced by the systemic hypotension that often accompanies trauma. Clearly, these enzymes are neither highly specific nor sensitive for pancreatic injuries. Elevated or rising levels may indicate damage but in themselves are not conclusive.35 In these cases, clinical correlation and further investigation are indicated. Base Deficit.: Metabolic acidosis in the setting of trauma can suggest the presence of hemorrhagic shock. This can be witnessed chemically as a decreased serum bicarbonate level, increased base deficit, or elevated serum lactate level. Although normal values do not exclude abdominal injury, substantive abnormalities, such as a base deficit greater than or equal to 6, may be predictive. These findings should be considered in clinical context, because the resolution of the laboratory findings will lag behind the clinical improvement of the patient. Liver Function Tests.: Elevated serum transaminases can result from hepatic trauma but do not distinguish minor contusions from severe injury.36 Alternatively, these may be symptomatic of alcohol-induced liver damage. Elevated liver transaminase levels may be useful for screening pediatric patients for intentional trauma (see Chapter 38). They may also play a role in pediatric patients in combination with a FAST examination as a screening tool to decrease the use of CT scanning, although serial physical examination is still required.37 Toxicology Analysis.: Screens for ethanol and drugs are often used in trauma centers. Their utility in the management of abdominal trauma, per se, has not been established, particularly in patients with normal mental status.38 Positive study findings may prompt the emergency physician to interdict and the patient to decrease the recidivistic use of ethanol or drugs, and physician intervention during this “teaching moment” has been shown to be effective. Very small quantities of readily detectable free intraperitoneal air are present in most patients with gastric, duodenal bulb, and colonic perforations but in fewer than one fourth of those with jejunal and ileal perforation. These are seen more readily on CT than plain films. Free intraperitoneal air uncommonly can be generated by mediastinal or pulmonary injury, as well as by barotrauma, and thus its presence is not pathognomonic of hollow viscus perforation. Intraperitoneal air is mobile, and to maximize visualization the patient should be kept in the appropriate upright or decubitus position for 10 to 15 minutes, if this is tolerable, before upright chest or decubitus abdominal radiographs are obtained. In upright films, air is located under the diaphragm or the central tendon of the diaphragm anteriorly. In supine films, air tracks under peritoneal attachments, such as the falciform ligament and urachus, up to the anterior abdominal wall. On films in which the patient is in a lateral decubitus position, air is located in the superior flank and outlines the lateral liver edge (Fig. 46-1). In cases of gastric perforations, air may be limited to the lesser sac. A rupture of a retroperitoneal hollow viscus can be detected by a stippling pattern outlining the duodenum, kidney, or psoas muscle (Fig. 46-2). Extraperitoneal colonic perforations may extravasate air, which outlines the psoas muscle and perinephric region. All of these injuries are much more readily identified and localized on abdominal CT. Over the last 35 years, CT scanning has continued to advance its place among diagnostics for trauma. Evolution to higher multislice helical and spiral scanners has improved resolution and greatly decreased the time required for the scan itself.39 Advantages.: In most situations, CT scanning has supplanted DPL because of its higher predictive ability for operative lesions and because it is noninvasive. CT scanning can define the injured organ and the extent of the injury. It is most accurate for solid visceral lesions and accurately discerns the presence, source, and approximate quantity of intraperitoneal hemorrhage (Fig. 46-3). It can demonstrate active bleeding from the liver or spleen and can be used to determine whether therapeutic angiographic embolization is indicated.40 CT scanning also evaluates the retroperitoneum (Fig. 46-4), an area not sampled by DPL, as well as the vertebral column, and can be readily extended above or below the abdomen to visualize the thorax or pelvis.41 CT scanning also provides definitive evaluation for most possible injuries to the urinary tract, including renal artery injury.42 It can also detect other vascular hemorrhage and obviate the need for angiography in some patients.43 CT scanning is particularly helpful in guiding nonoperative management of solid organ damage.44,45 This includes as-needed follow-up studies of convalescing patients with these injuries. It has also proven effective when incorporated in delayed fashion for patients with decreasing hematocrit, increasing base deficit, or subtle examination changes. By minimizing the incidence of nontherapeutic laparotomies for self-limited injury to the liver or spleen, it decreases morbidity and cost attendant to this operation.46 Increasingly, trauma centers are using CT with intravenous contrast only, as it has been shown that little additional information is provided by the addition of oral contrast, which delays scanning and may pose an aspiration risk for the patient.47,48 Disadvantages.: Disadvantages of CT scanning include relative insensitivity for injury of the pancreas, diaphragm, small bowel, and mesentery, although detection of these injuries is improving47,48 (Fig. 46-5). The last two are particularly worrisome because isolated coincidental hollow viscus injury in patients with blunt trauma, although uncommon, is not rare, and increased morbidity and death can ensue if diagnosis is missed or the condition goes undetected for a prolonged period. Findings on CT scans, including the suspected quantity of hemoperitoneum or the presence of isolated free fluid, are not able to forecast well the need for operative intervention.49 Complications can result from intravenous contrast administration or uncommonly from contrast material administered orally. Moreover, oral contrast delivery to opacify bowel is infrequently useful and typically omitted.47,50 Finally, patients must be temporarily removed from the resuscitation area for the study to be accomplished, which can put the patient at risk in the case of rapid clinical deterioration. However, CT scanning remains the cornerstone of diagnosis. In cases with equivocal CT scan results, such as more than physiologic fluid, or a worrisome history and physical examination findings, serial examinations or further diagnostic testing should be strongly considered, including DPL, particularly to evaluate for missed hollow viscus injury (Table 46-1). Table 46-1 Preferred Site of Diagnostic Peritoneal Lavage C, closed (percutaneous Seldinger technique); FO, fully open; SO, semiopen. *The stab wound or gunshot wound site should be avoided. Adapted from Runyon, M, Marx JA: Peritoneal procedures. In Roberts JR, Hedges JR (eds): Clinical Procedures in Emergency Medicine, 5th ed. Philadelphia, WB Saunders, 2009.
Abdominal Trauma
Perspective
Penetrating Abdominal Trauma
Epidemiology
Penetrating Abdominal Trauma
Blunt Abdominal Trauma
Pediatrics
Principles of Disease
Pathophysiology
Blunt Abdominal Trauma
Clinical Features
Penetrating Abdominal Trauma
Physical Examination
Penetrating Abdominal Trauma
Blunt Abdominal Trauma
Diagnostic Strategies
Hematology
Chemical
Radiology
Plain Radiographs
Computed Tomography
CLINICAL CIRCUMSTANCE
SITE
METHOD
Standard adult
Infraumbilical midline
C or SO
Standard pediatric
Infraumbilical midline
C or SO
Second- and third-trimester pregnancy
Suprauterine
FO
Midline scarring
Left lower quadrant
FO
Pelvic fracture
Supraumbilical
FO
Penetrating trauma
Infraumbilical midline*
C or SO
< div class='tao-gold-member'>

Full access? Get Clinical Tree


Abdominal Trauma
Only gold members can continue reading. Log In or Register to continue