Abdominal Pain, Vomiting, and Diarrhea
Samuel Sandowski MD
Rosemary M. Jackson MD
INTRODUCTION
“Mommy, my tummy hurts!” is a complaint heard frequently from children. Abdominal pain plagues almost all children at some point in their lives. For some, the pain is an acute, limited experience of viral gastroenteritis; others experience recurrent or chronic pain, such as in Familial Mediterranean Fever or Henoch-Schönlein purpura. Most cases require nothing more than observation and reassurance, although some require extensive evaluations or surgical interventions. Regardless of etiology, the provider will face the challenge of determining the best course of action for each patient with abdominal pain.
PATHOLOGY
All people perceive pain differently. The perception of pain varies among individuals and cultures. The perception of pain may even vary for the same individual from one day to the next. Though perceptions and responses to pain vary, however, the pain stimulus is the same. Abdominal pain is caused by stimulation of afferent fibers within cells in the dorsal root ganglia. Some fibers cross the midline and ascend to the medulla, midbrain, and thalamus. The pain is perceived in the post-central gyrus of the cerebral cortex.
Organs in the abdomen do not detect painful stimuli caused by cutting or burning; yet they are sensitive to distention, compression, and torsion. It is the peritoneal covering and the skin and muscles overlying the abdomen that detect painful stimuli as a sharp sensation. Inflammation and infarction also cause pain when they affect the peritoneum.
The peritoneum, of mesodermal origin, covers the organs within (visceral layer) and the inner surface (parietal layer) of the abdominal cavity. Autonomic nerves innervate the visceral layer, and the pain detected tends to be midline. Somatic nerves of spinal origin innervate the parietal layer, and the pain is perceived at its location (Martin & Rossi, 1997). Additionally, different types of nerve fibers, originating at T7-L2, innervate the two peritoneal layers. The visceral peritoneum contains C fibers, which are slow and give the sensation of dull, aching pain. A-λ fibers innervate the parietal peritoneum; these fibers are much quicker and cause the sensation of sharp, severe pain. Thus, in early appendicitis, abdominal pain first is dull and central due to visceral peritoneal inflammation. As the process progresses, the parietal peritoneum becomes inflamed. The pain localizes to the right lower quadrant and becomes sharper and more severe.
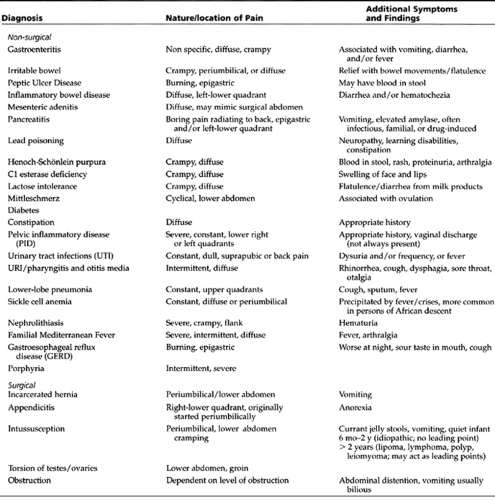
The etiologies of abdominal pains can be divided into acute, chronic, and acute on chronic. They also can be divided into surgical, medical, and idiopathic. They may further be subdivided into age groupings, such as infant, toddler, and adolescent (Table 38-1).
EPIDEMIOLOGY
Gastroenterological complaints are found in 5.4% to 13% of all children ages 17 years and younger [Centers for Disease Control and Prevention, 1994]. Abdominal pain may be acute, chronic, or recurrent. Recurrent abdominal pain is defined as three or more episodes of abdominal pain over a 3-month period (Seller, 1996). Patients with recurrent abdominal pain, however, may present with a new episode as “acute abdominal pain”.
Acute abdominal pain usually is defined as abdominal pain lasting less than 3 days. It accounts for approximately 5% of all unscheduled visits to primary care providers, urgent care centers, and emergency rooms (Scholer, Pituch, Orr, & Dittus, 1996). Fever, vomiting, anorexia, cough, and sore throat often accompany it. Most often, a “self-limiting” or medical condition such as “abdominal pain of uncertain etiology,” gastroenteritis, or constipation causes acute abdominal pain (Mason, 1996).
• Clinical Pearl
Often, extra-abdominal sources cause abdominal pain, including pharyngitis (especially cases caused by group A β-hemolytic streptococci), otitis media, pneumonia, lead poisoning, and diabetes (see Table 38-1).
In most cases, medical treatment, supportive therapy, appropriate antibiotics, and observation are sufficient. In 1% to 2% of cases, however, surgical intervention is necessary (Scholer, Pituch, Orr, & Dittus, 1996).
Appendicitis is the most common reason that older children with abdominal pain require surgical intervention (74%). In 50% to 60% of cases of children admitted for possible appendicitis, however, observation and further evaluation preclude the need for surgical intervention. When surgery is performed, 10% of cases reveal no pathology (Holland & Gollow, 1996). In children younger than age 4 years, diagnosing appendicitis is often more difficult. In children younger than age 5 years, incarcerated hernias and intussuception are the most common reasons for abdominal pain requiring surgical intervention.
HISTORY AND PHYSICAL EXAM
As with all diseases, the history and the physical exam are the guides to establishing a clinical diagnosis. Common questions to answer are the “PQRSTs” of pain:
P—place of pain. Where is it? Can the child point to it with one finger? Surgical etiologies tend to be more localized.
Q—quality of pain. Is it sharp? dull? aching? burning? colicky? crampy?
R—radiation of the pain. Does the pain stay in one place or go to the back? to the chest? Has the pain itself migrated?
S—symptoms associated with the pain. Is there vomiting? fever? anorexia? diarrhea? sore throat? The provider must explore a sexual history in all patients (including abuse as well as consensual activities).
T—timing of the pain. When did it start? How long does it last? How often does it occur? Has it happened before?
—things that make the pain better or worse. Does position, bowel movement, or medication affect the pain?
The provider must do the physical exam carefully and kindly, remembering that the patient is in pain. Since the abdomen is hurting, it is often best to examine it last. A thorough exam, starting with vital signs and including respiratory rate, pulse, blood pressure, and temperature, is essential. Tachypnea is seen with pneumonia. Tachycardia and hypotension occur with sepsis, peritonitis, or profound anemia and hemorrhage. Observing the skin, looking for any rash or pallor, may help identify hemolytic or sickle cell anemia, as well as purpura. A cardiac evaluation may reveal a murmur secondary to anemia (from GI bleeding, sickle cell
disease, or other etiologies). Auscultation of the lungs may uncover lower lobe pneumonia.
disease, or other etiologies). Auscultation of the lungs may uncover lower lobe pneumonia.
The abdominal exam should begin with observation. The provider should approach the child gently. This is best done after first talking with the child and parent and establishing trust. The clinician should note the child’s facial expression, so he or she can compare it to a “grimace” while palpating the abdomen. A grimace is often a more sensitive tool than any verbal acknowledgment of pain (Wagner, McKinney, & Carpenter, 1996). The clinician should observe the patient’s position, noting if he or she is bent over or writhing with pain. The provider should note the skin over the abdomen. Discoloration of the flank (Gray-Turner sign) or periumbilical discoloration (Cullen sign) occurs with hemorrhagic pancreatitis.
Auscultation should precede palpation; palpation that elicits pain may cause a paralytic ileus, and the provider may not be able to hear bowel sounds. The absence of bowel sounds indicates ileus and thus requires hospital admission. High pitched/hyperperistaltic sounds suggest mechanical obstruction. Prior to auscultation, allowing the child to touch the stethoscope and even place it on his or her abdomen eases anxiety.
The provider should perform palpation gingerly, starting with an area that is not painful and moving clockwise toward the painful area. The patient should lie supine, with knees slightly flexed. Engaging the child in conversation helps to distract him or her from the pain and the exam. Superficial palpation should precede deep palpation.
• Clinical Pearl
Instead of palpating with the hands, palpating with the stethoscope head may reduce fear and anxiety in a young child, since the stethoscope is not expected to produce as much pain as does manual palpation. This technique also may aid in identifying an exaggerated pain response. Patients expect pain when someone presses the abdomen with the hand and thus may exaggerate their response. They may not do so, however, when the abdomen is pressed with the head of the stethoscope, because they think that the provider is auscultating and not palpating.
The clinician should note signs of guarding, rebound, and any masses. The cough test (in which voluntary coughing elicits abdominal pain) has a sensitivity of 78% and a specificity of 79% for diagnosing peritonitis (Bennett, Tambeur, & Campbell, 1994) and is more sensitive than the manual test for rebound. The “heel drop jarring test,” in which the patient drops onto his or her heels after standing on the toes for 15 seconds, or to have the patient hop on one leg several times also may be used to diagnose peritonitis.
A rectal exam is part of the routine exam when the provider suspects a diagnosis of an acute abdomen. It may not aid in diagnosis, however, and is not always necessary (Mason, 1996). Though generally the rectal exam is uncomfortable, reproducing the pain on rectal exam when pressing on the appendix increases the suspicion of appendicitis. Stool guaiac testing reveals occult blood. Sexually active females should have a gynecological (speculum and bimanual) exam.
DIAGNOSTIC STUDIES
After performing the history and physical exam, the provider should begin a diagnosis-specific approach. He or she may treat obvious etiologies for abdominal pain, such as simple gastroenteritis, irritable bowel syndrome (IBS), upper respiratory illness, and otitis media without further testing. When testing is appropriate, the clinician should perform tests to confirm or exclude specific diagnoses.
Laboratory Testing
In children with pharyngitis, the provider should obtain a rapid strep test or throat culture. He or she should do blood testing methodically, not with a “shotgun” approach. In children with recurrent vomiting and diarrhea, the provider should draw an “SMA 6” or “Astra 7”. Electrolyte abnormalities may occur, and a measurement of blood urea nitrogen (BUN) and serum creatinine may help assess levels of dehydration. Elevated glucose levels suggest diabetes mellitus, and low serum bicarbonate (CO2) suggests sepsis or dehydration with secondary metabolic acidosis.
When the provider suspects hepatic involvement, he or she should evaluate liver function tests. Elevation of serum transaminases indicates hepatitis, which may be Hepatitis A, B, C, or numerous other viruses, such as Epstein-Barr. When the provider suspects pancreatitis, amylase levels usually are elevated.
Providers should routinely check lead levels on all young children, especially those who live in housing where leaded paint and dust continue to pose environmental hazards. Providers should query children with elevated levels about abdominal pains as a manifestation of lead poisoning. Additionally, older children with known exposures to lead require testing as well. Clinicians must report cases of elevated lead levels to the local Health Department.
The complete blood count (CBC) is not specific for identifying the etiology of abdominal pain but aids in evaluation. A low hematocrit suggests anemia (sickle cell or from GI bleeding). An elevated white blood cell (WBC) count suggests an inflammatory or infectious process, such as pelvic inflammatory disease (PID), gastroenteritis, mesenteric adenitis, or surgical emergencies, such as appendicitis and peritonitis.
The urine analysis (UA) may reveal blood (urolithiasis) or WBCs (urinary tract infections/pyelonephritis). Proteinuria found on UA may suggest target organ damage secondary to diabetes mellitus or connective tissue disorders (eg, Henoch-Schonlein purpura). The UA is normal in appendicitis but checked routinely to exclude genitourinary causes of abdominal pain.
Imaging
Plain Films
Plain x-rays are often the first imaging studies performed in patients with abdominal pain (Lee, 1976). While often unrevealing, a collection of plain films of the abdomen, such as the kidney-ureters-bladder (KUB), an upright abdomen, and an upright chest film, can identify emergent, potentially fatal conditions. The provider should note air distribution. Free intraperitoneal air (often seen as a crescent of lucency under the diaphragm) or air in the retroperitoneum suggests perforation of a viscus. If a child is unable to maintain the position required for an upright film or even a decubitus film, a supine film may suggest free intraperitoneal air in 59% of cases (Levine, Scheiner, & Rubesin, 1991). Common signs on these supine films include Riglers sign (air on both sides of the intestinal wall) and the right upper quadrant sign (air outlining the peritoneal cavity) (Gupta & Dupuy, 1997).
Air fluid levels, especially in a “ladder fashion,” suggest obstruction. The lack of air may represent late stages of obstruction. Excessive amounts of air in the colon (toxic megacolon) could be found in ulcerative colitis.
Foreign bodies and stones can be seen on plain films. Stones may be gallstones in the gallbladder or bile ducts, kidney stones in the kidney or ureter, or appendicoliths, which may correlate with appendicitis (Martin & Rossi, 1997).
Ultrasonography
Ultrasonography (US) has become a common imaging modality for patients with acute abdominal pain. It is the modality of choice for gynecological and obstetric imaging (Gupta & Dupuy, 1997). However, it is only useful in adding to the diagnosis in 50% of cases of acute abdominal pain (Walsh, Crawford, & Crossing, 1990). For appendicitis, US is highly specific (about 90%) and sensitive (about 95%). The provider’s clinical suspicion, however, always should guide treatment and decision making. US is best used as an adjunct when the provider’s clinical findings and suspicion are equivocal (Wilcox & Traverso, 1997). Therefore, in younger children in whom the diagnosis of appendicitis may be more difficult to make, US may play a larger role in establishing a diagnosis. Other diseases in which ultrasonographic findings may help establish or confirm a diagnosis in patients with abdominal pain are noted in Table 38-2.
When requesting US, providers must convey clinical questions and concerns to the sonographer, because not all US is the same. Regular/abdominal sonography looks at solid viscera, including the liver, spleen, pancreas, and kidneys, but usually not the appendix. Graded-compression sonography evaluates the GI tract only and measures “compressibility” of the bowel. Doppler flow sonography measures blood flow.
Computed Tomography
The use of Computed Tomography (CT) is useful in the diagnosis of appendicitis, diverticulitis, intestinal ischemia, pancreatitis, intestinal obstruction, and perforated viscus (Gupta & Dupuy, 1997). It is associated with greater cost and radiation exposure than US. The introduction of the helical CT, which images the patient during a single spiral scan and then reconstructs the images by computer, has eliminated the need for repeat images and additional radiation.
CT is a useful adjunct to US, and providers should consider it when the diagnosis remains equivocal. They also should use it as a guide to medical management of complications of appendicitis (such as evaluation and treatment of abscesses and phlegmon), especially when perforation occurrs (Sivit, 1997).
MANAGEMENT
Treatment of acute abdominal pain depends on its etiology. First and foremost is the necessity to identify the causes and development of the pain. Even if a diagnosis is not possible, the provider must determine a disposition. Is the patient stable enough to be sent home, or does he or she require hospitalization? If a child is found to have signs of an acute abdomen, then hospitalization, observation, and consultation with a surgeon is needed. If symptoms seem benign and recurrent (as suggestive of irritable bowel), then counseling and reassurance are appropriate. In all cases, the clinician must address severity of the pain, employ appropriate analgesics (when warranted), and correct and maintain hydration status. Specific treatments are described below for each disease.
APPENDICITIS
Appendicitis is the most common diagnosis considered when children younger than age 14 years present with abdominal pain to the emergency room or provider’s office (Simpson & Smith, 1996). Only a small percentage of patients, however, actually have appendicitis. Because of the high morbidity and mortality that can result from a perforated appendix, it is a diagnosis that must not be missed. The incidence of pediatric patients with perforated appendices at the time of diagnosis ranges from 30% to 65%. The diagnosis becomes even more difficult when the child is younger (Mason, 1996).
History and Physical Exam
The typical history is abdominal pain that starts periumbilically, migrates to the right lower quadrant, and gradually intensifies. The pain is constant, though sometimes the patient feels slight relief when flexed at the waist. The patient’s gait may be stooped. He or she may have anorexia and vomiting. Classically, the patient will present with fever and an acute abdomen, including rebound tenderness (called Rovsing’s sign), guarding, a positive cough test, and tenderness over the right lower quadrant on rectal exam.
Diagnostic Criteria
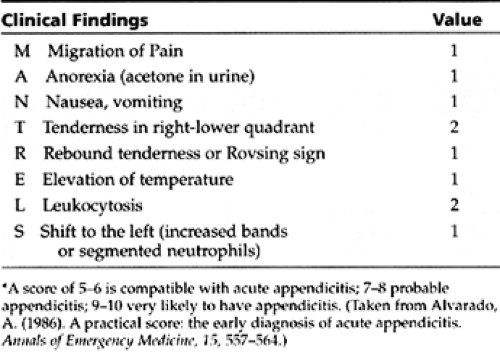
The diagnosis of appendicitis is challenging because not all patients present with typical and classical features. Often the history is vague and the physical exam findings are equivocal. Scoring systems have been created to help guide providers to the probability of making a diagnosis (eg, the MANTRELS Score – Table 38-3). The diagnosis of appendicitis is based on pathological examination of the removed appendix, but the decision to operate is based on clinical findings.
• Clinical Pearl
Persistent right lower quadrant tenderness in a child is the most specific, important, and diagnostic clinical finding.
Diagnostic Studies
Laboratory tests are used to support or aid in the direction of a diagnosis when clinical findings are equivocal. The WBC count usually is elevated, with an increased percentage of neutrophils and immature bands, “a shift to the left.” Though appendicoliths, also known as fecoliths, may suggest appendicitis, plain x-ray films usually yield little diagnostic value, unless a perforation has occurred, revealing free air.
Advanced imaging procedures have been used more commonly over the past decade. For all ages, US was found to have a sensitivity and specificity of 85% and 92% respectively (Orr, Porter, & Hartman, 1995). In children, however, sensitivity is about 90% and specificity is 97% (Ramachandran, Sivit, Newman, et al., 1996). The classic finding on US is that of a non-compressible, inflamed (> 6 mm) appendix. Computerized tomography (CT), especially spiral or helical CT, has proven to be a useful and accurate method of diagnosing appendicitis, with even higher sensitivities and specificity than US.
Management
Treatment of appendicitis is surgical. A false positive (white appendix) rate of less than 15% is often considered acceptable.
• Clinical Pearl
A surgeon should promptly evaluate all suspected cases. If unsure, the patient is probably best served by being admitted and observed, especially very young children, in whom the diagnosis is very difficult to make.
IRRITABLE BOWEL SYNDROME
Up to 22% of the U.S. adult population has irritable bowel syndrome (IBS). Most of these individuals are diagnosed in young adulthood and adolescence (Lynn & Friedman, 1995). These patients comprise up to 25% of referrals to gastroenterologists. The condition is twice as common in females than in males (except in India and Sri Lanka, where it is more common in males). Ten to 15% of school-aged children have recurrent abdominal pain, 52% of whom were diagnosed with IBS (Hyams, 1995).
Pathology
Patients with IBS have increased bowel motility and altered bowel contractions in response to stress. Some patients (often those who complain of pain) tend to have increased activity in the distal colon and rectum, while others (often those of who complain of diarrhea) have increased transit time of the colon with less water resorption. No one finding, however, has proved to be a consistent marker for the disease.
Patients with IBS may have different thresholds for pain. In these patients, balloon distention of the rectum, sigmoid colon, and small intestine causes pain at lower volumes as compared to controls. This observation led to the theory that patients with IBS have a lower threshold for visceral pain but not necessarily somatic pain (Accarino, Azpiroz, & Malagelada, 1995). It is still unclear, however, if this is normal perception to abnormal physiology, or abnormal perception to normal physiology. This question is further confused by not knowing if certain medications, such as serotonin inhibitors that are sometimes used in treatment, are acting centrally, altering the perception of pain, or locally on the gut at yet unidentified sites.
History and Physical Exam
In neonates, colic may be the first symptom. Young children may display frequent bouts of loose and watery stools, lasting for weeks, labeled as chronic diarrhea of childhood or “toddler’s diarrhea.” Others may have functional constipation. Chronic recurrent abdominal pain is also a frequent finding. Older patients usually complain of altered bowel habits, diarrhea alternating with constipation, and abdominal pain. In this age group, stress often aggravates and bowel movements or flatulence often relieve symptoms. The reader is referred to Chapter 57 for a complete discussion of IBS.
Signs and symptoms of weight loss, fever, rectal bleeding, and abdominal pain while sleeping suggest a diagnosis other than IBS.
PEPTIC ULCER DISEASE
Peptic ulcer disease most frequently occurs in adults. It may afflict adolescents and children but is rare in toddlers. The bacteria Helicobacter pylori usually is found. Research shows it to be more common in patients from lower socioeconomic status, but some studies have challenged this finding (Macarthur, Saunders, & Feldman, 1995). Symptoms range from chronic abdominal pain to GI bleeding. Treatment consists of eradication of H. pylori with proton pump inhibitors and antibiotics. Short-term continuation of acid reduction (with proton pump inhibitors, H2 blockers or antacids) is usually necessary. If the diagnosis is questionable, treatment seems suboptimal, or complications are suspected, a gastroesophagoduodenoscopy (EGD) or an upper GI series is warranted.
PANCREATITIS
Pancreatitis may occur throughout childhood and most commonly results from a mumps infection. When secondary to other etiologies, pancreatitis in childhood is rare and often associated with trauma, medications (eg, thiazides, steroids, estrogens), diseases (eg, diabetes mellitus, cystic fibrosis, hemolytic uremic syndrome, or liver diseases), or familial causes.
The pain is usually epigastric, and boring, drilling straight to the back. Nausea and vomiting are often present. Laboratory evaluation must include a CBC, amylase, lipase, serum glucose, BUN, electrolytes (SMA 6), liver function tests, and calcium. Additionally, an arterial blood gas is warranted. Treatment includes appropriate anal-gesia and sufficient hydration. Hospitalization, with intravenous hydration and bowel rest with nasogastric suction, is usually necessary. Complications include pseudocysts, abscesses, thrombosis, and necrosis of intraabdominal vessels and organs.
HENOCH SCHÖNLEIN PURPURA
Henoch Schönlein Purpura—also known as anaphylactoid purpura or nonthrombocytopenic purpura—is a vasculitis of unknown etiology. Children present with abdominal and joint pain and a characteristic rash. The rash classically begins as large patches of urticaria predominantly on the lower extremities but also on the arms and ears. The trunk is relatively spared. The rash then progresses to purpuric lesions, which become edematous, hence the term, palpable purpura. Gross hematuria and bloody stools also may be seen. Intussusception, as a result of edematous nubbins of intestinal mucosa acting as leading points, is a dangerous complication. Evaluation of the urine may reveal signs of a glomerulonephritis (proteinurea and hematuria); fortunately, this resolves without permanent renal damage in the vast majority of cases. Treatment with systemic steroids is useful for the child with severe GI symptoms but does not appear to help either the arthritis or nephritis. Nor does treatment appear to alter the natural course of the illness, which may last for 3 to 4 weeks. Fortunately, the prognosis in almost all children is uniformly excellent.

Full access? Get Clinical Tree