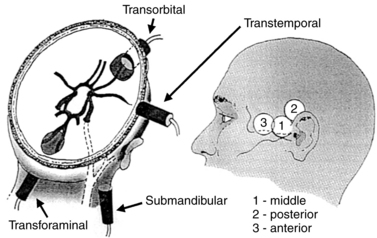
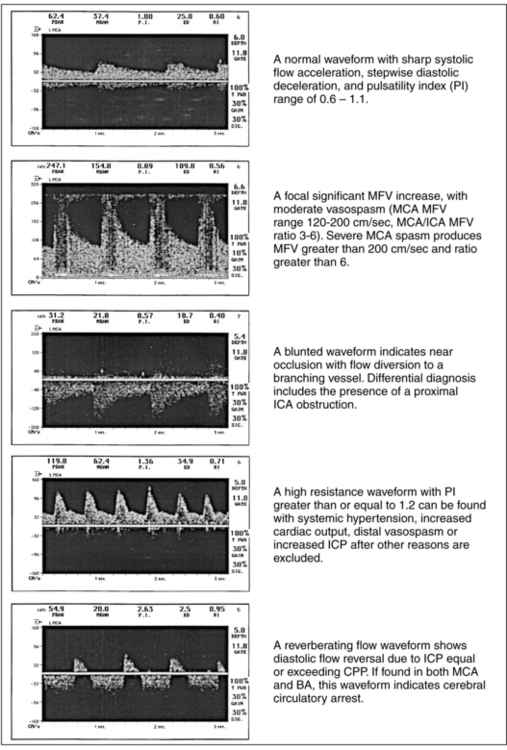
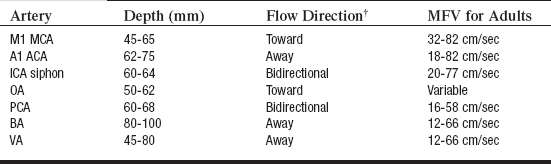
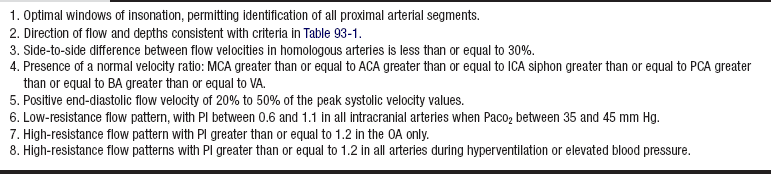
PROCEDURE 93 Transcranial Doppler scan measures blood flow velocities in the major branches of the circle of Willis through an intact skull. This measurement supports the grading of vasospasm severity, localization of intracranial stenoses or occlusions, detection of cerebral emboli, monitoring of hemodynamic changes with impaired intracranial perfusion, and assessment of the impact of therapeutic interventions on intracranial hemodynamics.7–9,18,24 • Knowledge of neuroanatomy and physiology is needed. • Clinical and technical competence related to transcranial Doppler (TCD) ultrasound scan is necessary. • Noninvasive assessment of the intracranial vasculature is indicated for patients with a subarachnoid hemorrhage, ischemic stroke, sickle cell disease, cerebral emboli, impaired vasomotor reactivity, cerebral circulatory arrest, and other neurovascular disorders.15,21 • Successful ultrasound penetration through the skull is possible through intracranial windows, which either lack bone (burr holes, flaps) or consist of thinner bone structure compared with the overall cranial bone thickness. Four windows are available for insonation: temporal, orbital, foraminal, and submandibular (Fig. 93-1).1–4 • The transtemporal window allows insonation of the middle cerebral artery (MCA), the anterior cerebral artery (ACA), the posterior cerebral artery (PCA), and the anterior and posterior communicating arteries (AComA and PComA).1–4 • The transorbital window allows insonation of the ophthalmic artery (OA) and the internal carotid artery (ICA) siphon.1–4 • The transforaminal window allows insonation of the vertebral arteries (VAs) and the basilar artery (BA).1–4 • The submandibular window allows insonation of the ICA as it enters the skull.1–4 TCD scan locates both the depth and direction of arterial blood flow relative to the transducer position and the ultrasonic beam direction. Flow moving toward the transducer is displayed as a waveform with a positive velocity spectrum, whereas flow moving away from the transducer is displayed as a waveform with a negative velocity spectrum.1–4,12,16 • The TCD scan measures cerebral blood flow velocities that should not be equated to cerebral blood flow (CBF) volume. TCD is an indirect reflection of CBF.4,15,21 • The examination should begin with maximal power and gate settings (e.g., power, 100%; gate, 10 to 15 mm) to expedite identification of the temporal window and various arterial segments. Once a good temporal window is established, the power may be reduced to adhere to the U.S. Food and Drug Administration (FDA) principles of (1) “as low as reasonably achievable” (ALARA) and (2) minimization of overall time of patient exposure to ultrasound scan. Transorbital examination should always be performed with minimal power (e.g., 10%) to avoid potential side effects from the heating of orbital structures.1–4 • The highest velocity signals for each arterial segment studied, and any abnormal or unusual waveforms, should be measured and stored in the system’s computer.3 • Criteria for normal insonation depths, flow direction, and mean flow velocities are used for appropriate identification of arteries and diagnosis of abnormalities (Fig. 93-2 and Table 93-1).2,15,18,21 Table 93-1 Depth, Direction, and Mean Flow Velocities for Circle of Willis Arteries* *Depth and MFV ranges may vary slightly between reference studies. †Toward the probe indicates a positive (+) waveform; away from the probe indicates a negative (–) waveform. (Adapted with permission from Alexandrov AV: Transcranial Doppler sonography: principles, examination technique and normal values, Vasc Ultrasound Today 10:141-160, 1998.) • Criteria for determination of a normal examination are listed in Table 93-2.2,15,18,21 Table 93-2 Criteria for Normal TCD Scan Findings (Reprinted with permission from Alexandrov AV: Transcranial Doppler sonography: principles, examination technique and normal values, Vasc Ultrasound Today 10:141-160, 1988.) • Criteria supporting differential diagnosis are listed in Table 93-3.2,15,18,21 Table 93-3 BA, Basilar artery; EDV, end-diastolic velocity; FV,
![]() Transcranial Doppler Monitoring
Transcranial Doppler Monitoring
PREREQUISITE NURSING KNOWLEDGE
Problem
Findings
Differential Diagnosis
Arterial stenosis
Focal MFV increase above normal values, turbulence, bruits
Flow diversion to adjacent arteries
Flow alteration distal to site of stenosis (deceleration, low PIs)
Primary arterial stenosis
Compensatory flow increase
Adjacent artery occlusion
Hyperemia
Arterial near occlusion
Blunted waveform
Focal decrease in MFV
Slow systolic acceleration
Slow flow deceleration
Flow diversion to adjacent arteries
Near occlusion at the site of insonation
Arterial occlusion proximal to insonation site
Incorrect vessel identification
Arterial occlusion
No detectable flow
Good unilateral window of insonation
High-resistance flow proximal to occlusion
Flow diversion to adjacent arteries
Primary arterial occlusion
Incorrect vessel identification
Mass effect
Arterial vasospasm*
Proximal vasospasm:
Focal or diffuse elevation of MFV without parallel FV increase in feeding extracranial arteries; HI greater than 3
Distal vasospasm:
Focal increase in flow pulsatility (PI greater than or equal to 1.2), indicating increased resistance distal to site of insonation
Increase in MFV in the involved and adjacent arteries may not be present
Vasospasm
Hyperemia
Vasospasm with hyperemia
Altered cerebral autoregulation
Increased intracranial pressure
Increased intracranial pressure
Decreased EDV or absent end-diastolic flow
Rapid flow deceleration
PI greater than or equal to 1.2
Note that these findings may be present in patients with increased cardiac output or elevated blood pressure and in elderly individuals
The presence of PI greater than or equal to 1.2 and positive end-diastolic flow in all arteries may be caused by the following:
Hyperventilation
Hypertension
Increased ICP
Unilateral PI greater than or equal to 1.2 may be caused by the following:
Compartmental ICP increase
Stenoses distal to the site of insonation
PI greater than or equal to 2.0 associated with absent end-diastolic flow is caused by extreme elevations in ICP and possible cerebral circulatory arrest
Cerebral circulatory arrest
Reversed end-diastolic flow or reverberating flow pattern or
Minimal systolic flow acceleration with no end-diastolic flow or
Absent flow signals in all intracranial arterial systems
Possible or probable circulatory arrest; measure both MCA and BA for 30 minutes; then reassess (transient arrest may occur during transient ICP increase or low blood pressure values)

Full access? Get Clinical Tree


93: Transcranial Doppler Monitoring