PROCEDURE 54 • Knowledge of the normal anatomy and physiology of the cardiovascular system, principles of cardiac conduction, and basic dysrhythmia interpretation is necessary. • Understanding of temporary pacemakers is needed to evaluate pacemaker function and the patient’s response to pacemaker therapy. • Clinical and technical competence related to use of temporary pacemakers is needed. • Advanced cardiac life support knowledge and skills are necessary. • Basic principles of hemodynamic monitoring are essential in assessment of the efficacy of temporary pacing therapy. • Knowledge of the pulmonary artery (PA) catheter function and its use relative to hemodynamic monitoring is a necessity with use of a PA catheter with pacing function (see Procedure 73). • Knowledge of the care of the patient with central venous catheters (see Procedure 70) is needed. • Principles of general electrical safety apply with use of temporary invasive pacing methods. Gloves always should be worn when handling electrodes to prevent microshock. In addition, the exposed proximal ends of the pacing wires should be insulated when not in use to prevent microshock.9–11 • The insertion of a temporary pacemaker is performed in emergent and elective clinical situations. • Temporary pacing may be used to stimulate the myocardium to contract in the absence of an intrinsic rhythm, establish an adequate cardiac output and blood pressure to ensure tissue perfusion to vital organs, reduce the possibility of ventricular dysrhythmias in the presence of bradycardia, supplement an inadequate rhythm with transient decreases in heart rate (e.g., chronotropic incompetence in shock), or allow the administration of medications (e.g., beta blockers) to treat ischemia or tachydysrhythmias in the presence of conduction system dysfunction or bradycardia. • Temporary invasive pacing is indicated for the following4,6,8: • The three primary methods of invasive temporary pacing are: transvenous endocardial pacing, pacing via a PA catheter, and epicardial pacing.
Temporary Transvenous and Epicardial Pacing
PREREQUISITE NURSING KNOWLEDGE
 Symptomatic third-degree atrioventricular (AV) block
Symptomatic third-degree atrioventricular (AV) block
 Symptomatic second-degree heart block
Symptomatic second-degree heart block
 Dysrhythmias that complicate acute myocardial infarction
Dysrhythmias that complicate acute myocardial infarction
 Symptomatic bradycardia or bradydysrhythmias
Symptomatic bradycardia or bradydysrhythmias
 New bundle-branch block with transient complete heart block
New bundle-branch block with transient complete heart block
 Alternating bundle-branch block
Alternating bundle-branch block
 Symptomatic sinus node dysfunction
Symptomatic sinus node dysfunction
 Treatment of bradycardia-tachycardia syndrome (sick sinus syndrome)
Treatment of bradycardia-tachycardia syndrome (sick sinus syndrome)
 Ventricular standstill or cardiac arrest
Ventricular standstill or cardiac arrest
 Long QT syndrome with ventricular dysrhythmias
Long QT syndrome with ventricular dysrhythmias
 Medication toxicity or adverse effects of a medication
Medication toxicity or adverse effects of a medication
 Prophylaxis with cardiac diagnostic or interventional procedures
Prophylaxis with cardiac diagnostic or interventional procedures
 Chronotropic incompetence in the setting of cardiogenic shock
Chronotropic incompetence in the setting of cardiogenic shock
 In temporary transvenous pacing, the pulse generator is externally attached to a pacing lead that is inserted through a vein into the right atrium or ventricle.
In temporary transvenous pacing, the pulse generator is externally attached to a pacing lead that is inserted through a vein into the right atrium or ventricle.
 Veins used for insertion of the pacing lead are the subclavian, femoral, brachial, internal jugular, or external jugular veins.
Veins used for insertion of the pacing lead are the subclavian, femoral, brachial, internal jugular, or external jugular veins.
 Single-chamber ventricular pacing is the most common method used in an emergency because the goal is to establish a heart rate as quickly as possible.
Single-chamber ventricular pacing is the most common method used in an emergency because the goal is to establish a heart rate as quickly as possible.
 Temporary atrial or dual-chamber pacing can be initiated if the patient needs atrial contraction for improvement in hemodynamics.
Temporary atrial or dual-chamber pacing can be initiated if the patient needs atrial contraction for improvement in hemodynamics.
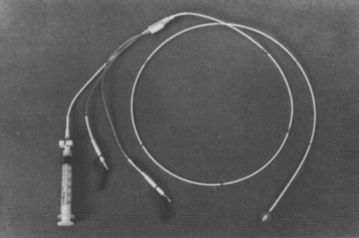
 The pacing lead is an insulated wire with one or two electrodes at the tip of the wire (Fig. 54-1).
The pacing lead is an insulated wire with one or two electrodes at the tip of the wire (Fig. 54-1).
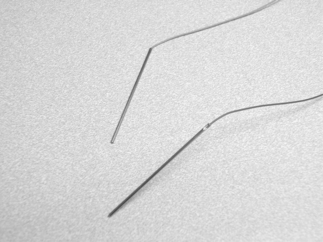
 The pacing lead can be a hard-tipped or balloon-tipped pacing catheter that is placed in direct contact with the endocardium. Most temporary leads are bipolar, with the distal tip electrode separated from the proximal ring by 1 to 2 cm (see Fig. 53-1).
The pacing lead can be a hard-tipped or balloon-tipped pacing catheter that is placed in direct contact with the endocardium. Most temporary leads are bipolar, with the distal tip electrode separated from the proximal ring by 1 to 2 cm (see Fig. 53-1).
 An external temporary pulse generator is connected to the transvenous pacing wire via a bridging or connecting cable.
An external temporary pulse generator is connected to the transvenous pacing wire via a bridging or connecting cable.
 Temporary atrial or ventricular pacing via a thermodilution PA catheter can be done with combination catheters that are specifically designed for temporary pacing.
Temporary atrial or ventricular pacing via a thermodilution PA catheter can be done with combination catheters that are specifically designed for temporary pacing.
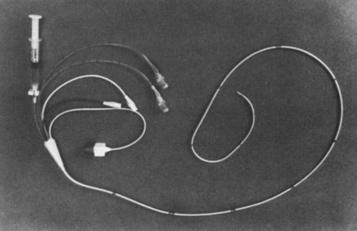
 PA pacing catheters feature atrial and ventricular ports for the introduction of the pacing lead wires (Fig. 54-2).
PA pacing catheters feature atrial and ventricular ports for the introduction of the pacing lead wires (Fig. 54-2).
 Use of a PA catheter combines the capabilities of PA pressure monitoring, thermodilution cardiac output measurement, fluid infusion, mixed venous oxygen sampling, and temporary pacing.
Use of a PA catheter combines the capabilities of PA pressure monitoring, thermodilution cardiac output measurement, fluid infusion, mixed venous oxygen sampling, and temporary pacing.
 One limitation of these multifunction catheters is that the simultaneous measurement of pulmonary artery occlusion pressure (PAOP) and pacing is usually not possible. Balloon inflation can cause repositioning of the pacing electrode with catheter movement; measurement of the PAOP may cause pacing to become intermittent.8
One limitation of these multifunction catheters is that the simultaneous measurement of pulmonary artery occlusion pressure (PAOP) and pacing is usually not possible. Balloon inflation can cause repositioning of the pacing electrode with catheter movement; measurement of the PAOP may cause pacing to become intermittent.8
54: Temporary Transvenous and Epicardial Pacing