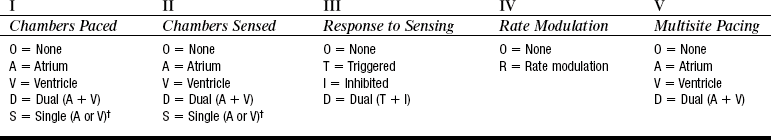
PROCEDURE 51 • Knowledge of the normal anatomy and physiology of the cardiovascular system, cardiac conduction, and basic dysrhythmia interpretation is necessary. • Knowledge of pacemaker function and patient response to pacemaker therapy is needed. • Advanced cardiac life support knowledge and skills are needed. • Permanent pacing is indicated for the following clinical conditions5: • Relative contraindications to permanent pacemakers include the following: • Components of the pacemaker are the pulse generator and the leads. The pulse generator weighs about 1 oz and is typically implanted subcutaneously in a pectoral pocket. The outer casing is made of titanium and contains the electronic components and the battery necessary to sustain pacing for years (Fig. 51-1). Typical battery life is 5 to 10 years and is dependent on variables such as output values, impedance, and percentage pacing. A transvenous pacing lead may be positioned in the right atrium, the right ventricle, or the left ventricle (or a combination of these), depending on the type of pacing needed. • Unipolar pacing involves a relatively large electrical circuit. The distal tip of the pacing lead is the negative electrode and is in contact with the myocardium. The positive electrode encompasses the metallic pacemaker case, located in the soft tissue. Energy is delivered from the negative electrode to the positive electrode, causing myocardial depolarization. The electrocardiogram (ECG) tracing shows a large, easily visible spike. • Bipolar pacing uses a smaller electrical circuit in which the distal tip of the pacing lead is the negative electrode in contact with the myocardium. The pacing lead has a second positive electrode that is located within 1 cm of the negative electrode. Energy is delivered from the negative electrode to the positive electrode, causing myocardial depolarization. The ECG tracing may show small spikes, or the spikes may not be visible on a surface ECG. • Basic principles of cardiac pacing include sensing, pulse generation, capture, and impedance (Table 51-1 lists definitions). Table 51-1 Pertinent Definitions Related to Pacemakers • Depending on the type of pacemaker, the pacemaker lead may be placed in the atrium, the right ventricle, or the left ventricle. A standard code exists to describe pacemakers (Table 51-2).2 The nurse must know the programmed mode with the pacemaker code to determine whether the device is functioning appropriately. Refer to Table 51-3 to review different programmed modes for pacemakers. Table 51-2 Revised NASPE/BPEG Generic Code for Antibradycardia Pacing* †Manufacturer’s designation only. NASPE, North American Society of Pacing and Electrophysiology; BPEG, British Pacing and Electrophysiology Group. (From Bernstein AD, et al: The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing, Pacing Clin Electrophysiol 25:261, 2002.) Table 51-3
Permanent Pacemaker (Assessing Function)
PREREQUISITE NURSING KNOWLEDGE
 Symptomatic sinus node dysfunction
Symptomatic sinus node dysfunction
 Acquired atrioventricular (AV) block in adults
Acquired atrioventricular (AV) block in adults
 Chronic bifascicular and trifascicular block
Chronic bifascicular and trifascicular block
 AV block associated with acute myocardial infarction
AV block associated with acute myocardial infarction
 Hypersensitive carotid sinus and neurocardiogenic syncope
Hypersensitive carotid sinus and neurocardiogenic syncope
 Specific conditions related to cardiac transplantation, neuromuscular diseases, sleep apnea syndromes, or infiltrative and inflammatory diseases such as cardiac sarcoidosis
Specific conditions related to cardiac transplantation, neuromuscular diseases, sleep apnea syndromes, or infiltrative and inflammatory diseases such as cardiac sarcoidosis
 Prevention and termination of supraventricular tachycardia via pacing
Prevention and termination of supraventricular tachycardia via pacing
 Hypertrophic cardiomyopathy with sinus node dysfunction or AV block
Hypertrophic cardiomyopathy with sinus node dysfunction or AV block
 Certain congenital heart defects
Certain congenital heart defects
 Left ventricular dysfunction, to restore ventricular synchrony (cardiac resynchronization therapy [CRT])1,3,8
Left ventricular dysfunction, to restore ventricular synchrony (cardiac resynchronization therapy [CRT])1,3,8
Sensing
Ability of the pacemaker to detect intrinsic myocardial electrical activity.
The pacemaker is either inhibited from delivering a stimulus or initiates an electrical impulse based on the programmed response.
Pulse generation
Occurs when the pacemaker produces a programmed electrical current for a programmed duration. This energy travels through the transvenous lead wires to the myocardium. The electrical impulse is seen as a line or spike on the ECG recording (pacemaker spikes are shown in Fig. 51-4).
Capture
Successful stimulation of the myocardium by the pacemaker impulse that results in depolarization. Two settings are used to ensure capture: amplitude and pulse width. Evidenced on the ECG by a pacemaker spike/stimulus followed by either an atrial or ventricular complex, depending on the chambers being paced (see Fig. 51-4).
Lead impedance
Opposition to flow of electrical current by the leads, electrodes, the electrode-myocardial interface, and body tissues.6 Measured in ohms, normally between 200 and 1200 ohms. A lead insulation break can cause impedance to fall below 200 ohms. A lead fracture can cause impedance to exceed 2000 ohms.
Failure of pulse generation
The pacemaker does not discharge a pacing stimulus to the myocardium at its programmed time. Evidenced by the absence of a pacemaker spike on the ECG where expected (see Fig. 51-5).
Failure to sense
The pacemaker has either detected extraneous signals that mimic intrinsic cardiac activity (oversensing) or has not accurately identified intrinsic activity (undersensing).
Oversensing is recognized on the ECG by pauses where paced beats were expected and prolongation of the interval between paced beats (see Fig. 51-6). Oversensing leads to underpacing.
Undersensing is recognized on the ECG by inappropriate pacemaker spikes relative to the intrinsic electrical activity (pacemaker spikes occurring within the P wave, QRS complex, or T wave) and shortened distances between paced beats (see Fig. 51-7). Undersensing leads to overpacing.
Failure to capture
Pacemaker has delivered a pacing stimulus that was unable to initiate depolarization and contraction of the myocardium. Evidenced on the ECG by pacemaker spikes that are not followed by a P wave for atrial pacing or spikes not followed by a QRS complex for ventricular pacing (see Fig. 51-8).
Pacemaker Code
Pacemaker Response
AOO
Atrial pacing; no sensing; asynchronous mode→paces atria at fixed, preprogrammed rate.
AAI
Atrial pacing, atrial sensing and inhibition; intrinsic P waves inhibit atrial pacing; if no sensed atrial events0paces in atria at preprogrammed rate.
AAIR
Atrial pacing; atrial sensing; intrinsic P waves inhibit atrial pacing; if no sensed atrial events→paces in atria; rate response to patient’s activity.
VOO
Ventricular pacing; no sensing; asynchronous mode→paces ventricle at fixed, preprogrammed rate.
VVI
Ventricular pacing: ventricular sensing; intrinsic QRS inhibits ventricular pacing; if no sensed events→paces in ventricle at preprogrammed rate.
VVIR
Ventricular pacing: ventricular sensing; intrinsic QRS inhibits ventricular pacing; if no sensed events→paces in ventricle; rate response to patient’s activity. 
Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access



