Procedures appropriate for ambulatory surgery are those associated with postoperative care that is easily managed at home and with low rates of postoperative complications that require intensive physician or nursing management.
 Whatever their age, ambulatory surgery is not restricted to patients of ASA physical status I or II. Patients of ASA physical status III or IV are appropriate candidates, providing their systemic diseases are medically stable.
Whatever their age, ambulatory surgery is not restricted to patients of ASA physical status I or II. Patients of ASA physical status III or IV are appropriate candidates, providing their systemic diseases are medically stable.
 In the 2006 ASA guidelines, the authors state that for patients with OSA, if a procedure is typically performed as an outpatient procedure and local or regional anesthesia is used, that the procedure can also be performed as an ambulatory procedure.
In the 2006 ASA guidelines, the authors state that for patients with OSA, if a procedure is typically performed as an outpatient procedure and local or regional anesthesia is used, that the procedure can also be performed as an ambulatory procedure.
 For adults, airflow obstruction has been shown to persist for up to 6 weeks after viral respiratory infections. For that reason, surgery should be delayed if an adult presents with a URI until 6 weeks have elapsed.
For adults, airflow obstruction has been shown to persist for up to 6 weeks after viral respiratory infections. For that reason, surgery should be delayed if an adult presents with a URI until 6 weeks have elapsed.
 In 2011, the ASA updated practice guidelines for preoperative fasting. The guidelines allow a patient to have a light meal up to 6 hours before an elective procedure and support a fasting period for clear liquids of 2 hours for all patients.
In 2011, the ASA updated practice guidelines for preoperative fasting. The guidelines allow a patient to have a light meal up to 6 hours before an elective procedure and support a fasting period for clear liquids of 2 hours for all patients.
 Time until discharge from ambulatory surgery is no different after peripheral nerve, central neuraxial blocks or general anesthesia.
Time until discharge from ambulatory surgery is no different after peripheral nerve, central neuraxial blocks or general anesthesia.
 Postoperative pain control is best with regional techniques.
Postoperative pain control is best with regional techniques.
 Nerve blocks using catheters can be placed before surgery that can be used to provide analgesia after the operation.
Nerve blocks using catheters can be placed before surgery that can be used to provide analgesia after the operation.
 After induction doses of propofol or thiopental, impairment after thiopental can be apparent for up to 5 hours, but only for 1 hour after propofol.
After induction doses of propofol or thiopental, impairment after thiopental can be apparent for up to 5 hours, but only for 1 hour after propofol.
 Although many factors affect the choice of agents for maintenance of anesthesia, two primary concerns for ambulatory anesthesia are speed of wake-up and incidence of postoperative nausea and vomiting.
Although many factors affect the choice of agents for maintenance of anesthesia, two primary concerns for ambulatory anesthesia are speed of wake-up and incidence of postoperative nausea and vomiting.
 It is important to distinguish between wake-up time and discharge time. Patients may emerge from anesthesia with desflurane and nitrous oxide significantly faster than after propofol or sevoflurane and nitrous oxide, though the ability to sit up, stand, and tolerate fluids and the time to fitness for discharge may be no different.
It is important to distinguish between wake-up time and discharge time. Patients may emerge from anesthesia with desflurane and nitrous oxide significantly faster than after propofol or sevoflurane and nitrous oxide, though the ability to sit up, stand, and tolerate fluids and the time to fitness for discharge may be no different.
 Nausea, with or without vomiting, is probably the most important factor contributing to a delay in discharge of patients and an increase in unanticipated admissions of both children and adults after ambulatory surgery.
Nausea, with or without vomiting, is probably the most important factor contributing to a delay in discharge of patients and an increase in unanticipated admissions of both children and adults after ambulatory surgery.
 In addition to the PACU, most ambulatory surgery centers in the United States have Phase II Recovery, which may be located in a different space than the PACU, but may also be conducted in the PACU space. Patients remain in Phase II Recovery until they are able to tolerate liquids, walk, and (depending on the operation) void.
In addition to the PACU, most ambulatory surgery centers in the United States have Phase II Recovery, which may be located in a different space than the PACU, but may also be conducted in the PACU space. Patients remain in Phase II Recovery until they are able to tolerate liquids, walk, and (depending on the operation) void.
Multimedia
 Vomiting Pharmacology
Vomiting Pharmacology
PLACE, PROCEDURES, AND PATIENT SELECTION
Ambulatory surgery occurs in a variety of settings. Some centers are within a hospital or in a freestanding satellite facility that is either part of or independent from a hospital. The independent facilities are often for-profit and not located in rural or inner-city areas. Some private companies acquire or build ambulatory facilities and then work usually with local surgeons who become the company’s affiliated staff. Physician’s office may also serve procedures (see Chapter 31 Office-based Anesthesia). Freestanding, independent facilities will continue to grow in number and popularity, although some consumers prefer care in units affiliated with hospitals.
A major concern of freestanding ambulatory surgery growth is that the surgery centers may force some hospitals out of business. This issue can be particularly problematic in areas in which population density or median income is low. Hospitals usually are nonprofit and care for patients who both can and cannot pay. Freestanding ambulatory facilities may also be nonprofit but usually do not provide charity care.
Some surgeons may work exclusively in a freestanding facility and not be on the staff of a hospital. A requirement for hospital staff privileges frequently is that a physician provides coverage for the hospital’s emergency department. Hospitals may try to expand emergency department coverage, but are pressured by some specialist surgeons. Some hospitals have lost emergency department coverage for an entire surgical specialty because that surgical specialty works exclusively in a freestanding facility.
Costs are lower for ASCs. Scheduling can be more predictable because the variety of cases is low. Turnaround times are usually also lower. The profits, particularly for freestanding facilities, do not have to subsidize more expensive areas of the hospital, such as ICUs. They also tend to serve only well-insured patients. Medicare also pays ASCs at a lower percent than what they pay hospitals for the same procedure. Medicare can then save money, though the payment system may force some ambulatory facilities to decide whether they accept Medicare patients.
Procedures appropriate for ambulatory  surgery are those associated with postoperative care that are easily managed at home and with low rates of postoperative complications that require intensive physician or nursing management. Establishing a low rate of postoperative complication depends on the relative aggressiveness of the facility, surgeon, patient, and payer. For example, procedures that postoperatively result in intense pain may be treated with continuous regional techniques that are continued at home whereas in other settings, these procedures are limited to inpatients.
surgery are those associated with postoperative care that are easily managed at home and with low rates of postoperative complications that require intensive physician or nursing management. Establishing a low rate of postoperative complication depends on the relative aggressiveness of the facility, surgeon, patient, and payer. For example, procedures that postoperatively result in intense pain may be treated with continuous regional techniques that are continued at home whereas in other settings, these procedures are limited to inpatients.
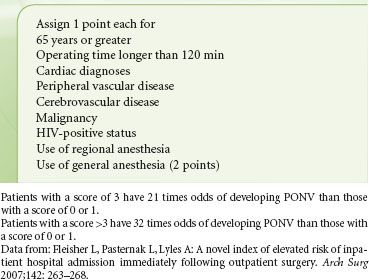
Scoring systems have been developed to help determine the likelihood of hospital admission after ambulatory surgery. One system is based on patients who were hospitalized after ambulatory surgery1 (Table 30-1).
TABLE 30-1. INDEX SCORING SYSTEM TO HELP IDENTIFY PATIENTS AT HIGHER RISK FOR HOSPITAL ADMISSION AFTER OUTPATIENT SURGERY
Many facilities set a 4-hour limit as a criterion for performing a procedure. Patients undergoing longer procedures should have their operations earlier in the day, primarily because in most freestanding facilities, the anesthesiologist cannot leave until the last patient is discharged. The need for transfusion is also not a contraindication for ambulatory procedures. Some patients undergoing outpatient liposuction, for example, are given autologous blood. Because of blood banking issues, though, ambulatory procedures that require the use of a blood bank are more commonly performed in larger facilities. Freestanding dialysis facilities commonly receive blood shipped from a blood bank located elsewhere and the same can be set up with freestanding ambulatory surgery facilities. The key is to have proper procedures established.
Some have wondered about the safety office-based procedures, following reports of deaths in Florida (see Chapter 31 Office-based Anesthesia). In one series from Florida that reviewed office surgical incidents from January of 2000 to January of 2006 that resulted in death, injury, or hospital transfer, 46 deaths were identified.2 Thrombophlebitis was the cause of death in the majority of patients. In a survey of 7,010 patients undergoing abdominal liposuction, the incidence of deep vein thrombosis was 0.04% and that of pulmonary embolus was 0.02%.3 It is hoped that organizations will soon provide better guidelines for stratifying risk and strategies to prevent venous thromboembolism after liposuction surgery.
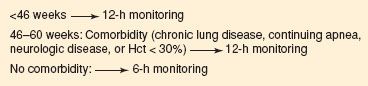
Infants whose postconceptual age is <46 weeks, or whose actual age is <60 weeks should be monitored for 12 hours after their procedure because they are at risk of developing apnea even without a history of apnea (Fig. 30-1).4 Infants older than 46 weeks and <60 weeks without disease should be monitored for 6 hours after their procedures. In one series of 127 premature patients who underwent inguinal hernia surgery, though, none had postoperative apnea.5 Some have found that spinal anesthesia without the use of other drugs intraoperatively or postoperatively is not associated with apnea; although in one study of 62 premature and former-premature infants who underwent surgery using spinal anesthesia, postoperative apnea was seen in 5 of 55 premature infants.6 Intravenous caffeine, 10 mg/kg, may help prevent apnea in infants, though the use of caffeine in the care of ambulatory patients at risk for apnea has not been studied.
FIGURE 30-1. Guide to determine length of monitoring for former preterm infants with a postconceptual age <60 weeks. Modified from: Walther-Larsen S, Rasmussen L. The former preterm infant and risk of postoperative apnoea: recommendations for management. Acta Anaesthesiol Scand. 2006;50:888–893.
At the other extreme of life, advanced age alone is not a reason to disallow surgery in an ambulatory setting. In a study of 89 patients who were 65 years and older randomized to receive either inpatient or outpatient care before undergoing inguinal hernia repair, all patients who were randomized to receive care as an outpatient were discharged on the day of surgery.7 Up to 2 weeks later, outcome was no different between groups. Increasing age, however, does affect the pharmacokinetics of drugs (see Chapter 7 Basic Principles of Clinical Pharmacology). Even short-acting drugs such as midazolam and propofol have decreased clearance in older individuals. In addition, as mentioned above, increased age may be a factor that affects the likelihood of unanticipated admission.
Admission, by itself, is not necessarily bad if it results in a better quality of care or uncovers the need for more extensive surgery. With proper patient selection for ambulatory procedures, which are usually elective, the incidence of readmission should be very low. Most medical problems that older individuals may experience after ambulatory procedures are not related to patient age, but to specific organ dysfunction. For that reason, all individuals, whether young or old, deserve a careful preoperative history and physical examination.
Whatever their age, ambulatory  surgery is no longer restricted to patients of American Society of Anesthesiologists (ASA) physical status I or II. Patients of ASA physical status III or IV are appropriate candidates, providing their systemic diseases are medically stable. In a review of ASA III patients who were compared with ASA I or II patients undergoing outpatient surgery, no significant increase in unplanned admissions, unplanned contact with health professionals, and postoperative complications was found.8 Certainly, not all life-threatening diseases have been studied as to how appropriate such patients with these diseases might be if they were to undergo ambulatory surgery. Yet, of those patients with such diseases who have been studied, the disease label itself does not seem to preclude an ambulatory surgical procedure.
surgery is no longer restricted to patients of American Society of Anesthesiologists (ASA) physical status I or II. Patients of ASA physical status III or IV are appropriate candidates, providing their systemic diseases are medically stable. In a review of ASA III patients who were compared with ASA I or II patients undergoing outpatient surgery, no significant increase in unplanned admissions, unplanned contact with health professionals, and postoperative complications was found.8 Certainly, not all life-threatening diseases have been studied as to how appropriate such patients with these diseases might be if they were to undergo ambulatory surgery. Yet, of those patients with such diseases who have been studied, the disease label itself does not seem to preclude an ambulatory surgical procedure.
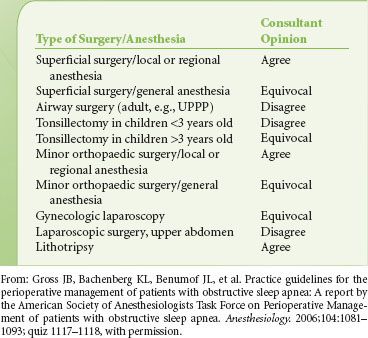
Patients who are obese represent a special situation. They are not more likely to have adverse outcomes, although they have a higher incidence of obstructive sleep apnea (OSA). In a review of 235 obese patients (body mass index [BMI] >40) who underwent outpatient surgery and were matched with control patients, unplanned admissions did not differ between groups.7,9 In a study of obstructive sleep apnea in patients undergoing ambulatory surgery, undiagnosed OSA was relatively common, and there was no relationship between OSA and unplanned hospital admission. Patients with OSA, though, had a higher likelihood of difficult intubation, needed more pressors, and needed more oxygen management in the PACU.10 Some feel that patients who need more narcotics may be at greater risk for apnea and should be observed for a longer period after their procedure. The ASA published practice guidelines for the perioperative management of patients with  OSA.11 In those guidelines, the authors state that for patients with OSA, if a procedure is typically performed as an outpatient procedure and local or regional anesthesia is used, the procedure can also be performed as an ambulatory procedure. Yet for patients who are at increased risk for perioperative complications, the procedure should not be performed in a freestanding ambulatory surgery facility. Table 30-2 presents a more complete list of recommended ambulatory procedures for patients with OSA, based on the ASA guidelines.
OSA.11 In those guidelines, the authors state that for patients with OSA, if a procedure is typically performed as an outpatient procedure and local or regional anesthesia is used, the procedure can also be performed as an ambulatory procedure. Yet for patients who are at increased risk for perioperative complications, the procedure should not be performed in a freestanding ambulatory surgery facility. Table 30-2 presents a more complete list of recommended ambulatory procedures for patients with OSA, based on the ASA guidelines.
TABLE 30-2. CONSULTANT OPINIONS REGARDING PROCEDURES THAT MAY BE PERFORMED SAFELY ON AN OUTPATIENT BASIS FOR PATIENTS AT INCREASED PERIOPERATIVE RISK FROM OBSTRUCTIVE SLEEP APNEA
Patients who undergo ambulatory surgery should have an adult take them home and stay with them afterward to provide care. Before the procedure, the patient should receive information about the procedure itself, where it will be performed, laboratory studies that will be ordered, and dietary restrictions. The patient must understand that he or she will be going home on the day of surgery. The patient, or some responsible person, must ensure all instructions are followed. Once at home, the patient must be able to tolerate the pain from the procedure, assuming adequate pain therapy is provided. The majority of patients are satisfied with early discharge, although a few prefer a longer stay in the facility. Patients for certain procedures such as laparoscopic cholecystectomy or transurethral resection of the prostate should live close to the ambulatory facility because postoperative complications may require their prompt return. “Reasonable” distance and time for the patient to get care if problems arise are not easily defined. This issue must be addressed by each facility and by each patient, and also depends on the type of surgery to be performed.
PREOPERATIVE EVALUATION AND REDUCTION OF PATIENT ANXIETY
Each outpatient facility should develop its own method of preoperative screening to be conducted before the day of surgery. The patient may visit the facility, or the staff members may telephone to obtain necessary information about the patient, including a complete medical history of the patient and family, the medications the patient is taking, and the problems the patient or the patient’s family may have had with previous anesthetics. Screened patients may be less likely to cancel surgery. The screening may uncover the need for transportation to the facility or the need for child care. The process also provides the staff with an opportunity to remind patients of arrival time, suitable attire, and dietary restrictions (e.g., when to stop eating and drinking, no jewelry or makeup). Staff members can determine whether a responsible person is available to escort the patient to and from the facility and care for the patient at home after surgery. The screening is the ideal time for the anesthesiologist to talk to the patient, but if that is not possible, the anesthesiologist may review the screening record to determine whether additional evaluation by other consultants is necessary and whether laboratory tests must be obtained. Patients who do not show up for their clinic appointment may be more likely not to show up for their operation.12
Automated history-taking may also prove beneficial during the screening of a patient. Computerized questionnaires or checklists with plastic overlays automate the acquisition of patient histories, flag problem areas, and suggest laboratory tests to be ordered. Such devices can also be used in a surgeon’s office, both to guide the surgeon in the selection of laboratory tests and to serve as a medical summary for the anesthesiologist. Such devices are particularly useful to control the cost of preoperative testing. They enable test ordering based on information obtained from a patient’s responses to health questions, thus eliminating requests for tests that are not warranted by history or physical examination.
Upper Respiratory Tract Infection
For adults, airflow obstruction has  been shown to persist for up to 6 weeks after viral respiratory infections. For that reason, surgery should be delayed if an adult presents with an upper respiratory infection (URI) until 6 weeks have elapsed. In the case of children, whether surgery should be delayed for that length of time is questionable. In a year-long survey of almost 10,000 children who underwent surgery, URI was associated with an increased risk for perioperative respiratory adverse events only when symptoms were present or had occurred within the 2 weeks before the procedure.13 Although a case may be cancelled because a child is symptomatic, the child may develop another URI when the procedure is rescheduled. In children, URI has not been shown to be associated with an increased length of stay in the hospital after a procedure. Independent risk factors for adverse respiratory events in children with URIs include use of an endotracheal tube (versus use of a laryngeal mask airway [LMA] or face mask), history of prematurity, history of reactive airway disease, history of parental smoking, surgery involving the airway, presence of copious secretions, and nasal congestion. Generally, if a patient with a URI has a normal appetite, does not have a fever or an elevated respiratory rate, and does not appear toxic, it is probably safe to proceed with the planned procedure.
been shown to persist for up to 6 weeks after viral respiratory infections. For that reason, surgery should be delayed if an adult presents with an upper respiratory infection (URI) until 6 weeks have elapsed. In the case of children, whether surgery should be delayed for that length of time is questionable. In a year-long survey of almost 10,000 children who underwent surgery, URI was associated with an increased risk for perioperative respiratory adverse events only when symptoms were present or had occurred within the 2 weeks before the procedure.13 Although a case may be cancelled because a child is symptomatic, the child may develop another URI when the procedure is rescheduled. In children, URI has not been shown to be associated with an increased length of stay in the hospital after a procedure. Independent risk factors for adverse respiratory events in children with URIs include use of an endotracheal tube (versus use of a laryngeal mask airway [LMA] or face mask), history of prematurity, history of reactive airway disease, history of parental smoking, surgery involving the airway, presence of copious secretions, and nasal congestion. Generally, if a patient with a URI has a normal appetite, does not have a fever or an elevated respiratory rate, and does not appear toxic, it is probably safe to proceed with the planned procedure.
Restriction of Food and Liquids Prior to Ambulatory Surgery
To decrease the risk of aspiration of gastric contents, patients are routinely asked not to eat or drink anything (non per os [NPO] or “nothing by mouth”) for at least 6 to 8 hours before surgery. Prolonged fasting could be detrimental to a patient. Yet in one study, where patients fasted from under 2 hours to more than 21 hours, there were minimal differences in blood pressure after propofol bolus for anesthesia induction.14 No trial has shown that a shortened fluid fast increases the risk of aspiration. Fluids actually empty quickly from the stomach. In one study of children 6 to 14 years who fasted overnight and then drank 7 mL/kg, median half-life for gastric emptying as assessed using MRI, was 24 minutes, though there was considerable individual variation.15 Admittedly, the majority of studies have not been specifically performed in individuals who are at an increased risk for aspiration.
In 2011, the ASA revised  practice guidelines for preoperative fasting16 (Table 30-3A and B). The guidelines allow a patient to have a light meal up to 6 hours before an elective procedure and support a fasting period for clear liquids of 2 hours for all patients. Coffee and tea are considered clear liquids. Coffee and tea drinkers should follow fasting guidelines but should be encouraged to drink coffee prior to their procedure because physical signs of withdrawal (e.g., headache) can easily occur. It is not clear if the guidelines should apply to patients with diabetes or dyspepsia. There is some evidence that shorter periods of preoperative fasting are accompanied by less postoperative nausea and vomiting (PONV). Yet, it is unclear whether rehydration during surgery is equivalent to a shorter fast before surgery in relation to PONV.
practice guidelines for preoperative fasting16 (Table 30-3A and B). The guidelines allow a patient to have a light meal up to 6 hours before an elective procedure and support a fasting period for clear liquids of 2 hours for all patients. Coffee and tea are considered clear liquids. Coffee and tea drinkers should follow fasting guidelines but should be encouraged to drink coffee prior to their procedure because physical signs of withdrawal (e.g., headache) can easily occur. It is not clear if the guidelines should apply to patients with diabetes or dyspepsia. There is some evidence that shorter periods of preoperative fasting are accompanied by less postoperative nausea and vomiting (PONV). Yet, it is unclear whether rehydration during surgery is equivalent to a shorter fast before surgery in relation to PONV.
TABLE 30-3. SUGGESTED GUIDELINES TO REDUCE THE RISK OF PULMONARY ASPIRATION
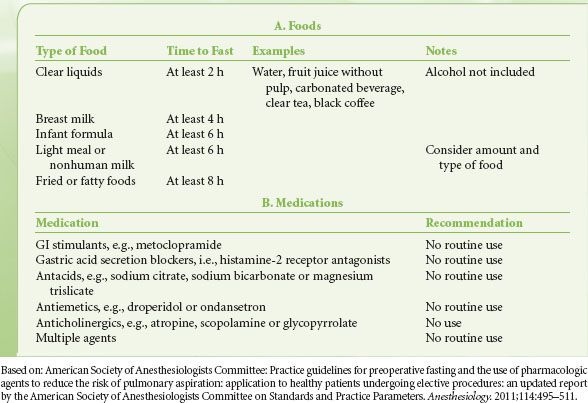
To ensure patients are optimally medically managed before their outpatient surgery, given the fact that clear liquids can be taken up to 2 hours before surgery, patients should be encouraged to take their chronic medications.
Anxiety Reduction
Clearly, some patients scheduled to undergo surgery are anxious, and they are probably anxious long before they come to the outpatient area. Indeed, anxiety probably begins as soon as the surgeon states the patient needs an operation and may not end even after discharge from the outpatient facility. Reasons for anxiety may include concerns about family, worry about pain after the procedure, and fear of complications.17 Preoperative reassurance from nonanesthesia staff and providing booklets with information about the procedure also reduce preoperative anxiety. However, use of booklets is less effective than a preoperative visit by the anesthesiologist. Audiovisual instructions also reduce preoperative anxiety. However, not all outpatients are anxious. Indeed, physicians often tend to overestimate the level of anxiety that patients are actually experiencing.18 Some operations can certainly generate more anxiety than others. If in doubt about patient anxiety, ask the patient.
Like adults, children should have some idea of what to expect during a procedure. But much of a child’s anxiety before surgery concerns separation from a parent or parents. A child is more likely to demonstrate problematic behavior from the time of separation from parents to induction of anesthesia if the procedure has not been explained preoperatively. Parents and children need to be involved in some preoperative discussions together so the anxiety of the parents is not transmitted to the child. The transmission of anxiety is at least as problematic as is the separation itself (e.g., experiences of children being left with babysitters). If the parents are calm and can effectively manage the physical transfer to a warm and playful anesthesiologist or nurse, premedication is not necessary. Semisedation may be awkward, and recovery after premedication may be prolonged.
If a child is accompanied by a parent during the induction of anesthesia, the child’s anxiety can be reduced. Some parents can become upset when they see their anesthetized child, who appears to be dead, albeit breathing and with a beating heart. Separation anxiety on the part of the parents is probably no different if the child is awake or asleep. Those children who have preoperative instructions and coaching (child life specialist) both for themselves and their families, and their parent/s present during induction have less anxiety preoperatively, less postoperative delirium, shortened discharge time after surgery, and reduced analgesic consumption after surgery.19 In addition, the patients had less severe emergence delirium symptoms, needed less fentanyl postoperatively, and were discharged earlier. Two important components of this technique are having the child practice with the anesthesia mask at home and use of distraction on the day of surgery.20
MANAGING THE ANESTHETIC: PREMEDICATION
The outpatient is not that different from the inpatient undergoing surgery. In both, premedication is useful to control anxiety, postoperative pain, nausea and vomiting, and to reduce the risk of aspiration during induction of anesthesia. Because the outpatient is going home on the day of surgery, the drugs given before anesthesia should not hinder recovery afterward. Most premedicants do not prolong recovery when given in appropriate doses for appropriate indications, although drug effects may be apparent even after discharge.
Benzodiazepines
Although historically many classes of drugs (e.g., barbiturates, antihistamines) have been used to reduce anxiety and induce sedation, benzodiazepines are currently the drugs most commonly used. Midazolam is the benzodiazepine most commonly used preoperatively. It can be used intravenously and orally. In adults, it can be used to control preoperative anxiety and, during a procedure alone or in combination with other drugs, for intravenous sedation. For children, oral midazolam in doses as small as 0.25 mg/kg produces effective sedation and reduces anxiety.21 With this dose, most children can be effectively separated from their parents after 10 minutes and satisfactory sedation can be maintained for 45 minutes. Some children, particularly younger and more anxious children, even when they receive midazolam 0.5 mg/kg, show signs of distress.22 Discharge may be delayed when midazolam is given before a short procedure. Oral diazepam is useful to control anxiety in adult patients, either the day before surgery or the day of surgery and before an intravenous line has been inserted.
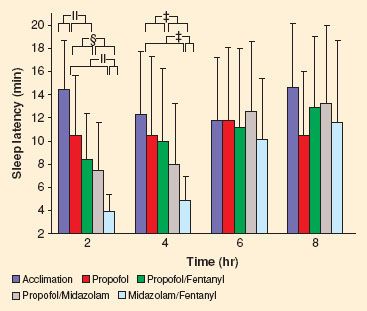
Fatigue associated with the effects of anxiolytics may delay or prevent the discharge of patients on the day of surgery, although more frequently patients are not discharged because of the effects of the operation. With regard to anesthesia effects, patients normally stay in the facility not because they are too sleepy but because they are nauseous. In adults, particularly when midazolam is combined with fentanyl, patients can remain sleepy for up to 8 hours (Fig. 30-2).23 Although children may be sleepier after oral midazolam, discharge times are not affected.
FIGURE 30-2. Patients can remain sleepy after receiving midazolam and fentanyl, even 8 hours after drug administration. The abscissa represents time (hours) after sedation. The ordinate represents sleep latency (i.e., time to fall asleep). Data are the mean time to fall asleep. An individual is sleepier if less time is required to fall asleep. Subjects receiving the midazolam and fentanyl combination were much sleepier than the same subjects receiving other types of sedation. Although not seen in the figure, up to 8 hours after sedation, some subjects were still sleepier than before they received drug. Reprinted from: Lichtor JL, Alessi R, Lane BS. Sleep tendency as a measure of recovery after drugs used for ambulatory surgery. Anesthesiology. 2002;96:878–883, with permission.
At proper doses, neither midazolam nor diazepam place patients at any additional risk for cardiovascular and respiratory depression. Decreased oxygen saturation has been reported after injection of midazolam. Routine administration of supplemental oxygen with or without continuous monitoring of arterial oxygenation is recommended whenever benzodiazepines are given intravenously. This precaution is important not only when midazolam is given as a premedicant but also when it is used alone or with other drugs for conscious sedation. The potential for amnesia after premedication is another concern, especially for patients undergoing ambulatory surgery. Anterograde amnesia certainly occurs. Although benzodiazepines facilitate retrograde amnesia, in one study there was no immediate retrograde amnesia after intravenous midazolam, 2 to 10 mg.24 For benzodiazepines, the effects on memory are separate from the effects on sedation. In addition, amnesia is not simply an effect of drug administration but, among other factors, it is also a function of stimulus intensity.
Opioids and Nonsteroidal Analgesics
Opioids can be administered preoperatively to sedate patients, control hypertension during tracheal intubation, and decrease pain before surgery. Meperidine (but not morphine or fentanyl) is sometimes helpful in controlling shivering in the OR or the postanesthesia care unit (PACU), although treatment is usually instituted at the time of shivering and not in anticipation of the event.
Opioids are useful in controlling hypertension during tracheal intubation. Opioid premedication prevents increases in systolic pressure in a dose-dependent fashion. After tracheal intubation, systolic, diastolic, and mean arterial blood pressures sometimes decrease below baseline values.
It would seem that preoperative administration of opioids or nonsteroidal anti-inflammatory drugs (NSAIDs) may be useful for controlling pain in the early postoperative period. Indeed, in a study where patients undergoing laparoscopic cholecystectomy received oxycodone preoperatively, they had lower pain scores, required less rescue analgesic consumption, and had shorter time to discharge from the recovery room.25 In another study, though, pain management for major plastic surgery procedures after celecoxib given before, during and after surgery, was no better than celecoxib given the day after surgery.26 Ibuprofen or acetaminophen can be given rectally to children around the time of induction. In children, time to rescue analgesia is longer if rectal as opposed to intravenous acetaminophen is used.27 In children, an initial loading dose of 40 mg/kg is appropriate. And, when preoperative rectal acetaminophen is combined with a nonsteroidal anti-inflammatory drug, particularly for more painful procedures, postoperative pain is less than when either drug is given individually.28
Preoperative sedation is not needed for every patient. The following is our practice when patients require drugs to relieve anxiety. For the patient who has been seen at least 24 hours before a scheduled procedure and expresses a desire for medication to relieve anxiety or has anxiety that cannot be relieved with comforting, oral diazepam, 2 to 5 mg per 70 kg body weight, is prescribed for the night before and at 6 am on the day of surgery (even if surgery is scheduled for 1 pm or later). For patients seen for the first time in the preoperative holding area who seem to need medication, midazolam, 0.01 mg/kg, is administered intravenously, or the patient is brought into the OR and propofol, 0.7 mg/kg, is injected intravenously. For children, when necessary, oral midazolam, 0.25 mg/kg, is administered in the preoperative holding area. When the child is asleep, acetaminophen, 40 mg/kg rectally, and ketorolac, 0.5 mg/kg intravenously, are administered prior to initiation of surgery.
INTRAOPERATIVE MANAGEMENT: CHOICE OF ANESTHETIC METHOD
There are several choices among anesthetic methods: General anesthesia, regional anesthesia, and local anesthesia. Regional and local anesthesia can be used with or without sedation. Except for obstetric cases, for which regional anesthesia may be safer than general anesthesia, all three types are otherwise equally safe. However, even for experienced anesthesiologists, there is a failure rate associated with regional anesthesia.
Certainly, some procedures are possible only with a general anesthetic. For others, the preference of patients, surgeons, or anesthesiologists may determine selection. The cost of sedation is usually less than the cost of a general or regional anesthetic. In a comparison of costs for patients undergoing inguinal hernia surgery in ten hospitals in Sweden, for example, intraoperative and postoperative costs were least in patients who received local anesthesia.29 Those patients who received local anesthesia also spent less time in the OR, had less postoperative pain, and the least problems with urination. The three types of anesthesia, though, are not an option for all operations. In another study that compared groin hernia repair after either general, regional or local infiltration, medical complications were more common after regional versus general anesthesia and urologic complications were more common after regional versus local infiltration.30 Less cost, then, may not always also be accompanied by improved quality. Where spinal anesthesia was compared to general anesthesia for patients undergoing hip or knee replacement procedures, costs for drugs and supplies were less for spinal anesthesia; recovery costs were also less due to less cost for pain management.31
Time to recovery may also influence the choice of anesthetic method. In a study of patients undergoing prostate biopsy, discharge after general anesthesia was faster than after spinal anesthesia.32 Conversely, in a study of patients undergoing upper limb trauma surgery, pain in the PACU and time to meet criteria for hospital discharge was less than for patients who underwent general anesthesia for the procedure.33  In a meta-analysis of peripheral nerve and central neuraxial blocks compared with general anesthesia, time until discharge from the ambulatory surgery unit was no different for the three groups.34 Interestingly also, postoperative nausea in the central neuraxial block group was not different from the general anesthesia group. In a study of patients undergoing spinal or general anesthesia for knee surgery, recovery times were equivalent, but after spinal anesthesia, postoperative side effects were fewer.35 In a study of stop-flow perfusion, a chemotherapeutic technique, where spinal anesthesia and general anesthesia were compared, anesthesia preparation was 5 minutes longer for spinal anesthesia, though using the study’s standards for PACU admission, only patients receiving general anesthesia needed PACU admission.36 Also, pain and PONV were greater in the general anesthesia group. When applying studies of regional anesthesia to everyday practice, remember that the studies come from centers where the authors are experienced in performing regional anesthesia and that might not be the case in other practices.
In a meta-analysis of peripheral nerve and central neuraxial blocks compared with general anesthesia, time until discharge from the ambulatory surgery unit was no different for the three groups.34 Interestingly also, postoperative nausea in the central neuraxial block group was not different from the general anesthesia group. In a study of patients undergoing spinal or general anesthesia for knee surgery, recovery times were equivalent, but after spinal anesthesia, postoperative side effects were fewer.35 In a study of stop-flow perfusion, a chemotherapeutic technique, where spinal anesthesia and general anesthesia were compared, anesthesia preparation was 5 minutes longer for spinal anesthesia, though using the study’s standards for PACU admission, only patients receiving general anesthesia needed PACU admission.36 Also, pain and PONV were greater in the general anesthesia group. When applying studies of regional anesthesia to everyday practice, remember that the studies come from centers where the authors are experienced in performing regional anesthesia and that might not be the case in other practices.
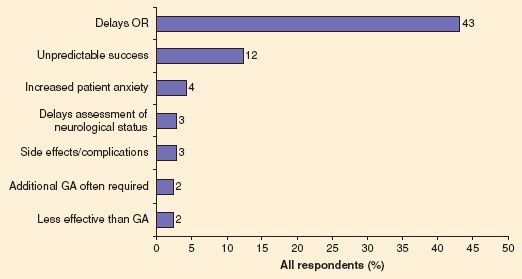
For some procedures such as arthroscopy, patients might prefer a regional anesthetic simply because they are curious and want to watch the surgery.37 Postoperative pain is less after regional anesthesia, which is discussed in more detail later in this section. Also, with regional anesthesia or sedation, some of the side effects of general anesthesia can be avoided, although no form of medical care is without side effects. Whenever drugs are given that affect memory, patients might complain that they do not remember events that occur after the procedure. Although with regional anesthesia more time is required to place a block than it takes to induce a general anesthetic, a meta-analysis of several studies showed this increased time to be on average no more than 8 to 9 minutes.34 In one survey of orthopedic surgeons, the majority of surgeons who direct their patients’ choice of anesthetic choose regional anesthesia, although the potential delay in establishing a block and perceived unpredictable success detracted from their enthusiasm with regional anesthesia (Fig. 30-3).38 For patients, the distinction between general anesthesia and regional anesthesia is probably less important than the fact the patient needs to undergo a procedure.39
FIGURE 30-3. Operating room (OR) delays are the major reasons orthopedic surgeons do not favor regional anesthesia. GA, general anesthesia. Reprinted from: Oldman M, McCartney CJ, Leung A, et al. A survey of orthopedic surgeons’ attitudes and knowledge regarding regional anesthesia. Anesth Analg. 2004;98:1486–1490, with permission.

Full access? Get Clinical Tree






