Edited by George Jelinek Stephen A Bernard and Paul A Jennings Ambulance services have the primary role of providing rapid stretcher transport of patients to an emergency department (ED). Increasingly, paramedics are also trained to provide emergency medical care prior to hospital arrival in a wide range of life-threatening illnesses with the expectation that earlier treatment will improve patient outcomes. Many countries have a single telephone number for immediate access to the ambulance service in cases of emergency, such as 911 in North America, 999 in the United Kingdom and 000 in Australasia. However, the accurate dispatch of the correct ambulance skill set in the optimal time frame is complex. It is inappropriate to dispatch all ambulances on a ‘code 1’ (lights and sirens) response, since this entails some level of risk to the paramedics and other road users. On the other hand, it may be difficult to identify accurately life-threatening illnesses or injuries using information gained from telephone communication alone, especially from bystanders. Also, it may be inappropriate to dispatch paramedics with advanced life-support training to routine cases where these skills are not required since they then become unavailable for a subsequent call. In order to have consistent, accurate dispatch of the appropriate skill set in the optimal time frame, many ambulance services are now using computer-aided dispatch programs. These computer programs have structured questions for use by call-takers with limited medical training. Pivotal to accurate telephone dispatch is identification of the chief complaint, followed by subsequent structured questions to determine the severity of the illness. The answers to these questions allow the computerized system to recommend the optimal paramedic skill set and priority of response. This computer algorithm is medically determined according to local protocols and practices and provides consistency of dispatch. Most ambulance services generally have at least four dispatch codes. A code 1 (or local equivalent terminology) is used for conditions that are considered immediately life threatening. For these, emergency warning devices (lights and sirens) are routinely used. The possibility of life-saving therapy arriving as soon as possible is judged as outweighing the potential hazard of a rapid response. In a code 2 (or equivalent) response, the condition is regarded as being urgent and emergency warning devices may be used only when traffic is heavy. In a code 3 response, an attendance by ambulance within an hour is deemed medically appropriate. Finally, a non-emergency or ‘booked’ call is a transport arranged at a designated time negotiated by the caller and the ambulance service. Despite continuous developments in computer algorithms, accurate telephone identification of life-threatening conditions may be difficult. For example, identification of patients who are deceased (beyond resuscitation) [1], in cardiac arrest [2], or suffering acute coronary syndrome [3] has been shown to lack the very high sensitivity and specificity that might be expected. The dispatch centre also has a role for telephone instructions on bystander cardiopulmonary resuscitation [4] and first aid. For conditions that are regarded as non-urgent, the dispatch centre may transfer the call to a ‘referral service’ for the provision of a medical response other than an emergency ambulance. This might include dispatch of a district nurse for a home visit or the provision of simple medical advice with instructions to see a family physician or attend an emergency department if symptoms persist. Ambulance treatment protocols vary considerably around the world. Since there are few randomized, controlled trials to provide high quality evidence-based guidance for pre-hospital care, there is still much controversy and considerable variation in the ambulance skill set in different ambulance services. Many ambulance services provide a number of varying levels of skill set, dispatching ambulance officers trained in basic life support (including defibrillation) to non-emergency or urgent cases (ambulance paramedics) and more highly trained officers (designated as advanced life-support paramedics or intensive-care paramedics) to patients with an immediately life-threatening condition for which advanced life-support skills may be appropriate [5]. In addition, ambulance services may co-respond with other emergency services (such as fire fighters) to provide rapid-response defibrillation. The evidence for some of the more common pre-hospital interventions is outlined in the following sections. Pre-hospital trauma care may be considered as either basic trauma life support (clearing of the airway, assisted ventilation with a bag/mask, administration of supplemental oxygen, control of external haemorrhage, spinal immobilization, splinting of fractures and the administration of inhaled analgesics) or advanced trauma life support (ATLS) including intubation of the trachea, intravenous (IV) fluid therapy, decompression of tension pneumothorax and the administration of intravenous analgesia. On arrival at the scene of the patient with suspected major trauma, paramedics are trained to perform an initial ‘DR-ABCDE’ evaluation which is similar to the approach that has been developed for physicians, namely consideration of dangers, response, airway, breathing, circulation, disability and exposure. Of particular importance in the pre-hospital trauma setting are dangers to paramedics from passing traffic, fallen electrical wires and fire from spillage of fuel. The initial assessment of the airway and breathing includes the application of cervical immobilization in patients who have a mechanism of injury that suggests a risk of spinal column instability. Although decision instruments have been developed to identify patients in the emergency department who require radiographic imaging [6], the accuracy of these guidelines in the pre-hospital setting is uncertain. Spinal immobilization of many patients with minimal risk of spinal cord injury is uncomfortable and may lead to unnecessary radiographic studies [7]. Therefore, the recommendation to immobilize the neck in all cases of suspected spinal-column injury based on mechanism of injury alone is currently being challenged [8]. On the other hand, if spinal cord injury is suspected, patients should be transported with full spine immobilization [9]. Accurate triage of major trauma patients is an important component of trauma care in cities with designated major trauma centres. Triage tools based on vital signs, injuries and modifying factors, such as age, co-morbidities and mechanism of injury, are used [10]. Paramedic judgement may also have a role, although some injuries, such as occult intra-abdominal injuries, are difficult to detect on clinical grounds [11]. The role of ATLS by paramedics, particularly intubation of the trachea in comatose patients and intravenous cannulation for fluid therapy in hypotensive patients, is controversial. Although these interventions are routinely used in critically injured patients after hospital admission, studies to date indicate that the provision of ATLS provided by paramedics may not improve outcomes [5,12]. On the other hand, few studies conducted to date have been sufficiently rigorous to allow definitive conclusions and many were conducted in an urban setting with predominantly penetrating trauma rather than blunt trauma. Therefore, many ambulance services continue to authorize advanced airway management and intravenous fluid resuscitation in selected trauma patients, particularly those who are injured some distance from a trauma service. Following severe head injury, many unconscious patients have decreased oxygenation and ventilation during pre-hospital care and this secondary brain injury is associated with worse neurological outcome [13]. In addition, a depressed gag or cough reflex may lead to aspiration of vomit and this may cause a pneumonitis, which may be fatal or result in a prolonged stay in an intensive care unit. To prevent these complications of severe head injury, endotracheal intubation may be performed. This facilitates control of oxygen and carbon dioxide, provides airway protection and is routinely performed in patients with Glasgow coma score<9 following severe head injury after hospital arrival [14]. Most patients with severe head injury maintain a gag or cough reflex and successful intubation requires the use of drugs to facilitate laryngoscopy and placement of the endotracheal tube. The usual approach in the emergency department involves rapid sequence intubation (RSI), which is the administration of both a sedative drug and a rapidly acting muscle-relaxant, such as suxamethonium. It is unclear from the literature as to whether RSI should be performed pre-hospital by paramedics or, alternatively, be performed in an emergency department by appropriately trained physicians. Pre-hospital RSI performed by paramedics has been reported in numerous studies as having a high success rate [15]. However, it is uncertain whether this procedure is associated with improved outcomes [16]. Recently, a prospective, randomized, trial in adult patients with severe traumatic brain injury reported that paramedic RSI increased the rate of favourable neurological outcome at 6 months when compared to intubation in the hospital by physicians [17]. On the other hand, this study also showed a relatively high incidence of cardiac arrest in the patients who underwent paramedic RSI. Therefore, some uncertainty remains as to the efficacy of this procedure. Intravenous fluid resuscitation has been shown to worsen outcome in patients with penetrating trauma and hypotension [18]. However, most major trauma in Australasia and Europe is blunt rather than penetrating and few patients require urgent surgical control of haemorrhage. Therefore, the issue of pre-hospital IV fluid for the treatment of hypotension remains the subject of debate. Supporters of pre-hospital IV fluid therapy suggest that this treatment is intuitively beneficial and that any delay of this therapy increases the adverse effects of prolonged hypotension, which may result in end-organ ischaemia, leading to multiorgan system failure and increased morbidity and mortality. On the other hand, opponents of pre-hospital IV fluid therapy suggest that this therapy prior to surgical control in patients with uncontrolled bleeding increases blood loss due to increased blood pressure, dilution coagulopathy and hypothermia from large volumes of unwarmed IV fluid. Any additional blood loss would increase transfusion requirements and could be associated with increased morbidity and mortality. There is no evidence from clinical trials for benefit of the administration of IV fluid to bleeding patients in the pre-hospital setting. A meta-analysis of the studies to date suggests that pre-hospital IV fluid does not improve outcomes [5]. Nevertheless, if intravenous fluid is given to patients with hypotension and severe head injury, crystalloid rather than colloid should be given, particularly in hypotensive patients with severe traumatic brain injury [19]. The administration of effective analgesia in the pre-hospital setting for traumatic pain remains a difficult issue for ambulance services. Many paramedics are not trained to administer IV therapy and treatment options are, therefore, limited to inhaled therapy. Inhaled analgesic treatments include methoxyflurane and oxygen/nitrous oxide. However, while the former is reasonably effective [20], there are concerns with the administration of this agent in an enclosed space, such as the rear of an ambulance, because of the perceived risk of repeated exposures of these analgesics to the paramedics. Alternatively, the training of paramedics in the insertion of an IV cannula and administration of small increments of IV morphine is increasingly regarded as a feasible alternative to inhalation analgesia. Alternative routes of narcotic administration, such as intranasal administration, are the subject of current studies. For example, the use of intranasal fentanyl has been shown to be equivalent to intravenous morphine [21]. An alternative analgesic agent for paramedic use is ketamine. Ketamine, in addition to morphine, has been shown to be superior to morphine alone for traumatic pain. In a randomized, controlled trial, adult patients with moderate to severe traumatic pain were randomized to receive either 5 mg of morphine followed by ketamine, or morphine alone [22]. Those who received morphine and ketamine reported a significant pain score reduction compared to those who received morphine alone. However, the rate of adverse effects, such as nausea and dysphoria, was higher following ketamine compared with morphine. In 1966, external defibrillation was introduced into pre-hospital care and this led to the development of ‘mobile coronary care units’ in many countries for the delivery of advanced cardiac care for the patient with suspected myocardial ischaemia [23]. This approach was subsequently extended to rapid response for defibrillation of patients in cardiac arrest. Protocols for the management of pre-hospital cardiac arrest are based on the concept of the ‘chain of survival’, which includes an immediate call to the ambulance service, the initiation of bystander CPR, early defibrillation and advanced cardiac life support (intubation and drug therapy). The patient in cardiac arrest represents the most time-critical patient attended by ambulance services. For the patient with ventricular fibrillation, each minute increase from time of collapse to defibrillation is associated with an increase in mortality of approximately 10%. However, most ambulance services have urban response times that average 8–9 minutes. Since there may be 2 minutes between collapse and dispatch and 1 minute between arrival at the scene to delivery of the first defibrillation, total time from collapse to defibrillation would usually be approximately 12 minutes. Therefore, current survival rates for witnessed cardiac arrest in urban areas are low [24] and there are even fewer survivors in rural areas [25]. The most effective strategy to improve outcomes would be to decrease ambulance response times. However, this would require very significant increases in ambulance resources and would be an expensive strategy in terms of cost per life saved. Alternatively, response times to cardiac arrest patients may be reduced with the use of co-response by first responders equipped with defibrillators. Such a first responder programme has been introduced in Melbourne, Australia with promising results [26]. The role of advanced cardiac life support (ACLS) during cardiac arrest remains controversial [27]. For example, in a randomized, controlled trial comparing a basic life-support approach with an advanced life-support approach, the rate of survival to hospital discharge was 10.5% for the ACLS group compared with 9.2% for the no ACLS group (P=0.61) [28]. This finding of a lack of efficacy of ACLS during cardiac arrest remained after adjustment for underlying differences between the groups in the rates of ventricular fibrillation, response interval, witnessed arrest or arrest in a public location. Therapeutic hypothermia after resuscitation from cardiac arrest is used in many hospitals, particularly when the initial cardiac arrest rhythm is ventricular fibrillation. A number of clinical trials have tested whether therapeutic hypothermia should be initiated by paramedics after resuscitation using a bolus of cold IV fluid [29,30] or intranasal cooling [31]; however, the results of these studies do not currently support this therapy prior to hospital arrival. Most ambulance services have protocols for the management of the patient with chest pain where the cause is suspected as an acute coronary syndrome. These protocols usually include administration of aspirin and sublingual trinitrates followed by rapid transfer to an emergency department for definitive diagnosis and management. In addition, pain relief using intravenous morphine may be given by advanced life-support paramedics. The role of supplemental oxygen in patients with ST segment elevation myocardial ischaemia (STEMI) but without hypoxia remains uncertain [32]. While these interventions may decrease symptoms, more recent strategies to improve overall outcomes involve triage by paramedics of patients with STEMI using 12-lead electrocardiography to centres for interventional cardiology [33]. For patients with STEMI who are greater than 1 hour to a cardiac catheterization laboratory (i.e. rural patients), pre- hospital thrombolysis may be considered. In a recent European trial, patients with STEMI who presented within 3 hours after symptom onset but who were unable to undergo primary percutaneous coronary intervention (PCI) within 1 hour were assigned to undergo either primary PCI or fibrinolytic therapy [34]. The primary endpoint of death, shock, congestive heart failure or reinfarction occurred in 12.4% of patients in the pre-hospital fibrinolysis group and in 14.3% of patients in the primary PCI group (relative risk in the fibrinolysis group, 0.86; 95% confidence interval, 0.68 to 1.09; P=0.21). The rates of intracranial bleeding were similar in the two groups (after the dose of fibrinolysis was halved in the over 75 years patients). These data suggest that pre-hospital thrombolytic therapy is appropriate if there is a delay of greater than 1 hour in transport to a definitive centre for PCI. Some patients with an acute coronary syndrome develop a cardiac arrhythmia during ambulance care. Pulseless ventricular tachycardia is treated with immediate defibrillation and amiodarone by slow IV infusion is recommended for ventricular tachycardia where a pulse is palpable and the patient is alert [35]. However, the pre-hospital drug treatment of supraventricular tachycardia is more controversial. While the use of verapamil or adenosine appears to be equivalent in efficacy [36], many ambulance services require the patient to be transported for 12-lead electrocardiography and management of the supraventricular tachyarrhythmia in an emergency department. During myocardial ischaemia, the patient may develop pulmonary oedema and, in these patients, the use of oxygen and glyceryl trinitrates is regarded as useful [37]. Despite common use of non-invasive ventilation (NIV) in the emergency department for patients with acute pulmonarty oedema, pre-hospital continuous positive airway pressure for this indication has not been widely adopted, since the equipment is expensive and oxygen consumption is high. Nevertheless, there is some evidence that continuous positive airway pressure is feasible in the pre-hospital setting, may reduce the need for intubation and may reduce short-term morbidity [38]. Early identification and effective management of stroke aims to promote optimal recovery. The ambulance plays an important role in stroke management by triaging patients with suspected stroke to an appropriate hospital. Use of a validated stroke screen tool has been shown to increase diagnostic accuracy in identifying stoke and thus facilitate transfer to a stroke centre. There are a number of published stroke screening tools for paramedic use such as the Los Angeles Motor Score (LAMS) [39] and the Melbourne Ambulance Stroke Score [40] that have been shown to be effective in accurately identifying stroke. Patients suspected to be suffering from a stroke should be preferentially transported to a facility with stroke expertise. The patient with hypoglycaemia due to relative excess of exogenous injected insulin will suffer neurological injury unless the blood glucose level is promptly corrected. Treatment of the conscious patient involves orally administered dextrose. For unconscious patients, intravenous 20% dextrose should be administered. For paramedics who are not trained to insert IV cannulae or where IV access is not possible, the administration of intramuscular glucagon is also effective, although this is associated with an increase in the time to full consciousness [41]. Patients who respond to treatment may refuse transport to hospital since they feel they have recovered. However, patients on oral hypoglycaemic agents may later develop recurrent hypoglycaemia [42]. Therefore, transport to hospital in this patient group is recommended. Patients who inject narcotic drugs may suffer coma and respiratory depression which is readily reversed by naloxone. However, the administration of IV naloxone by paramedics is somewhat problematic, since IV access may be difficult and the half-life of IV naloxone (approximately 20 minutes) may be shorter than the injected narcotic. If the patient awakens and leaves medical care, there may also be a recurrence of sedation. Therefore, many ambulance services administer naloxone via the intramuscular or subcutaneous route. While the absorption via this route may be slower, overall, the time to return of normal respirations is equivalent. To avoid the use of needles, naloxone may also be administered via the intranasal route and this has an equivalent onset time to intramuscular naloxone [43]. Many patients with known severe anaphylaxis are prescribed adrenaline (epinephrine) by their physician for self-administration. The use of intramuscular adrenaline (epinephrine) by paramedics is a safe and effective pre-hospital therapy [44]. Generally, a dose of adrenaline 0.3 mg IM together with IV fluid therapy is recommended as first-line therapy for anaphylaxis with intravenous adrenaline reserved for patients who become severely hypotensive. Out-of-hospital status epilepticus is also regarded as a time-critical medical emergency. The first-line treatment of status epilepticus is usually a benzodiazepine. For many years, this was provided using the IV or rectal route of administration. More recently, there are supportive data that intramuscular midazolam is equally effective to intravenous benzodiazepine [45]. Many ambulance services therefore now authorize midazolam 0.1 mg/kg in the adult patient with seizure, with a half dose considered in older patients. Marcus Kennedy The definition of retrieval varies by jurisdiction, however, it includes the interhospital transfer of critical patients using specialized clinical staff, transport platforms and equipment. In most regions, this definition extends to the pre-hospital environment when medical staff crewing is deployed and, in this setting, is termed primary retrieval. In various systems, staff may include medical, nursing, advanced life support (ALS) paramedic or intensive care paramedic (or equivalents) in a range of combinations or crew-mix. Retrieval generally involves the transfer of patients with critical illness or life-threatening injury: situations where the patient requires the highest levels of clinical care and vigilance. Retrieved patients are often unstable, at the margin of physiological compensation and in need of specialized investigation and intervention. They are often at that phase of an emergency presentation where diagnosis is incomplete, treatment is problem-focused and risk is high. This setting therefore requires special expertise, risk-averse processes and fail-safe systems characterized by anticipation, redundancy, rapid response and reliability. Retrieval is a coordinated process that provides specialized assessment and management, prior to and during transfer of critically ill patients from situations where resources or services are inadequate, to a destination where definitive care can be provided. It aims to deliver the same or higher level of clinical care as that available at the point of referral, thus ensuring that the patient is not exposed to any reduction in the quality of clinical care, despite the inherent risks of the transport environment. The need for retrieval is related to the limitations of health facilities and the geography of populations. It is a reasonable premise that rural communities have a right to equitable and timely access to critical care medicine; however, it is recognized that there is often an urban/rural divide in regard to the accessibility of healthcare generally and to specialized critical care in particular. Key clinical ‘gap’ areas exist at both urban and rural and regional levels in regard to trauma, neurosurgery, cardiac and neonatal and paediatric critical care. Advances in medicine and technology are inevitably (at least initially) usually concentrated in major metropolitan centres, thus increasing the need for critical patient transport (e.g. coronary percutaneous procedures, interventional radiology, such as angio-embolization, major trauma centres and paediatric tertiary and quaternary care hospitals. Given that such divides exist and that critical-care transfer is inevitable, retrieval medicine aims to ensure quality of care in transfer in distinction to the somewhat ad hoc approach to irregular critical-care transfers that otherwise may be the case in less systematized approaches. Retrieval systems are often a product of their geography and some services have evolved due to their unique environment. Examples include Nordic systems and alpine systems that have emerged from the demands of challenging altitude and temperature extremes, urban trauma service (such as HEMS London) and systems driven by the tyranny of distance, such as the Queensland retrieval system. Retrieval systems vary by state and internationally. There are no uniform system designs or standards and, consequently, services vary in their use of transport platforms and crew types (nurse, paramedic, doctor). Staff may be employed by a health department, ambulance service, by contract with a private provider or a retrieval service may utilize hospital personnel. A state service may incorporate several retrieval service providers with central coordination; alternately, systems exist with local governance and responsibility at a district or area level. Transport platforms are generally state owned and operated or contracted; however, non-government-owned helicopters may be part of a state system (and have historically received both benevolent and state funding). In the past, such services were the mainstay of retrieval practice and were often initiated by passionate volunteers, being funded by community donations, corporate sponsorship and government grants. Governance systems for such services and their coordination and performance responsibilities were typically variable. Consequently, retrieval systems have evolved, leading to increased systematization and corporate and clinical governance, aiming at reduction in variation, greater accountability and increased reliability at the system level. Most countries have progressively moved towards centralized state systems. These are characterized by central coordination centres that use nurses, paramedics and doctors who work together utilizing their complementary skills and experience. Neonatal, paediatric, perinatal and adult retrieval services may be integrated, co-located or separate; however, the trend of recent years is to co-locate these services with common governance, to allow synergies to be realized in regard to operational processes, infrastructure, management, education, research, response platforms and clinical staff. Most retrieval services have developed similar systems for management of the generic operational processes of: patient referral, case coordination, response and logistics, clinical intervention, and destination determination (Table 26.2.1). In addition, these are usually supported by a formal array of governance elements (Table 26.2.2). Table 26.2.1 Elements of operational management of retrieval services Programme guidelines Quality reporting Reporting to Medical Standards Committee Management guidelines Data management Organizational structure Contracts and memoranda of understanding Budget and financial system Annual and strategic planning Management and data reports Table 26.2.2 Elements of clinical governance of retrieval services Guidelines for coordinators Guidelines for retrieval clinicians Support staff guidelines Equipment management systems Orientation and training Professional development Clinical documentation Case follow up and feedback Case review and audit Incident management Indicator measurement Credentialling Performance management In addition, states may legislate [1] or learned and academic bodies may publish guidelines and standards to promote safe systems of patient transfer, particularly in the critical-care sector [2]. Case coordination is at the heart of all retrieval systems. As a process it commences with the initiation of contact from a referral site. It is important for referrers to understand the indications for retrieval and to have clear guidelines (both system and local) to encourage early referral and good decision making. Statewide trauma systems and neonatal paediatric care systems often have well established transfer criteria; however, processes for other clinical groups are often less developed and may be ad hoc. Mature retrieval systems act as a single point of entry for the referrer, preferably providing services by initiation of a single call to a system-wide phone number. Coordination staff are appropriately qualified senior clinicians, with specialized training and knowledge. Case coordination fundamentally answers: what are the needs of the referrer and their patient? Are the needs for clinical advice, for organization of transport and crew or for assistance in obtaining an appropriate destination for a critical patient? The coordinator must determine quickly and efficiently the planning and intervention priorities for each case. These may be for immediate care or advice, immediate response, destination planning or consideration of complex decisions involving logistics, crew or transport platforms. Coordinators need to display leadership while at all times taking a systems perspective and avoiding tunnel vision or task fixation. Coordination must be provided through high performance organizations and, typically, utilizes sophisticated communication technologies, such as multiparty conference calls, telehealth videoconferencing, case recording and comprehensive data management systems. Coordination of retrieval also implies an ongoing process of communication and feedback with the referrer of case progress, estimated response times and knowledge of patient status changes. During the response and transfer phase the coordination centre maintains communication with response teams, providing logistic support and mission oversight. Retrieval services generally use road, rotary wing (helicopter), or fixed wing aircraft response and transport platforms. For international retrieval missions, commercial larger jet transport is used and, in uncommon settings, aquatic transport platforms may be used. In consideration of platform selection for a mission, clinical factors must be factored first; these will include need for pressurization, need for space for specialized crew or equipment and patient size. Further to these factors, urgency (of response or return leg or both outbound and return components), distance to referral hospital, availability of helipads at referral and destination hospitals and need to minimize the out-of-hospital time for the patient. Heightened risk for patients in transit is experienced during platform transfers (from bed to trolley to ambulance to aircraft stretcher and so on) and, in general terms, in the out-of-hospital setting. Minimization of number of patient transfers and the out-of-hospital time for the critical care retrieval patient are important principles. Road transport platforms should be specifically designed and fitted out for retrieval purposes to minimize variation (improving crew performance and safety) and the risk of ad hoc unsecured equipment placement. Use of helicopters (with crews of appropriate skill mix) in retrieval response has been demonstrated to improve patient outcomes [3,4], particularly patients with severe trauma and others with a need for time-critical interventions. In general, helicopter transfer is considered for retrieval of patients approximately 75–175 km from base, with road response used for shorter transfers and fixed wing for longer. These broad recommendations vary depending on road, geography and climatic conditions and on the performance characteristics and landing options for individual aircraft. Fixed wing transfers have the advantage of providing a (usually) pressurized aircraft, greater speed and comfort, more space and a controlled temperature. Rotary wing aircraft have advantages of door-to-door transfer where helipads exist at referral and destination sites, the primary response capability and the potential to avoid road transport legs, and multiple patient transfers. Road transfer offers spatial flexibility, door-to-door transfer and cost efficiency (Fig. 26.2.1). Staff selected for roles in retrieval must meet required professional and personal standards. Critical-care capability is essential and medical staff specialist training in a critical-care specialty is desirable. Similarly, nursing and paramedic staff must be trained to intensive care practitioner level. In addition, all staff must have specific training in management of the retrieval environment, clinical care in transport settings and personal and crew behaviours. The retrieval environment poses particular risk and technical training regarding platforms, procedures, relevant legislation, communication methods, rescue and escape procedures and equipment performance characteristics is needed. Training in clinical care during retrieval needs to ensure capability in management of the complete range of critical care, trauma and intensive care scenarios and an ability to apply depth of clinical knowledge to the relatively compact window of patient care that the retrieval mission represents. Practitioners need to understand in a retrieval setting that an intervention may be possible and ideal while also being inappropriate and inefficient or, that an intervention may be desirable but not be possible or practical. Compromise and pragmatism have a role in pre- and interhospital transfer particularly where priority exists for reaching a definitive care destination. Training in personal and crew behaviours is necessary to optimize the cohesiveness and functionality of the retrieval team – formal exposure to crisis resource management tools is a standard component of aeromedical and road-based retrieval education [5]. In interaction with referring practitioners and primary responders, the retrieval team needs to exhibit empathy, listening skills and professional behaviours – avoiding arrogance, premature conclusions or judgemental behaviour. The training and knowledge base required is significant, therefore training processes must be formalized and must be supported by ongoing professional development and regular credentialling in addition to compliance with relevant regulations. Crew safety is paramount, so personal protective equipment and clothing which meets aviation and ambulance service standards is mandatory. Safety risk arises also in long and overnight missions and crewing must be adequate to allow sharing of clinical vigilance duties and patient interventions at times of fatigue and to allow for adequate breaks and rest. Retrieval services play a major role in disaster response and management and generally provide a significant component of the early response to such incidents. Retrieval services and, in particular, their coordination processes are also key to the distribution and reception phase of the disaster response – providing system overview of capability and capacity of health services to receive victims. Retrieval staff must therefore be trained to expert status in this discipline [2,6]. Retrieval medicine and primary response aeromedical settings provide the most challenging of all clinical environments and, therefore, choice of staff skill sets and professional team makeup is fundamental to optimizing clinical outcomes. The central tenets of this clinical environment are that a critical-care retrieval team must consist of (at least) two professionals [6]. They must be trained to critical-care standard and work within their core scope of practice. The skill set they provide must meet the clinical needs of the patient. In most national and international jurisdictions, blended medical practitioner and paramedic or nursing crews satisfy these tenets. Significant literature supports the role of medical practitioners in this environment due to the additional diagnostic capability, procedural range, extent of knowledge and depth of clinical understanding they contribute [7]. Such skills are complemented by the skill set of critical-care-trained nursing staff. Paramedic staff contribute substantial critical-care capability (depending on individual jurisdictional training levels) together with expertise in the transport and pre-hospital scene environments. Crews comprised of paramedic or nursing staff paired in various combinations and without a medical crew member are appropriate for lower risk critical-care transfers, or for non-critical-care retrieval. Skill set needs to match the requirements of the patient in the basic dimensions of clinical complexity and physiological stability; the more unstable and complex patient clearly requiring a higher skill mix in the retrieval team. In rare situations, and where life-saving intervention may be possible, the transport of highly specialized clinical staff to the patient may be appropriate and should be considered, for example, transporting a surgeon to perform an infield amputation on an entrapped patient (Fig. 26.2.2).
Emergency and Medical Systems
26.1 Pre-hospital emergency medicine
Introduction
Dispatch
Clinical skills
Trauma care
Basic trauma life support
Advanced trauma life support
Intubation
Intravenous fluid
Analgesia
Cardiac care
Cardiac arrest
Acute coronary syndromes
Cardiac arrhythmias
Pulmonary oedema
Other medical emergencies
Stroke
Hypoglycaemia
Narcotic overdose
Anaphylaxis
Seizures
26.2 Retrieval
Retrieval systems
Retrieval processes
Retrieval coordination
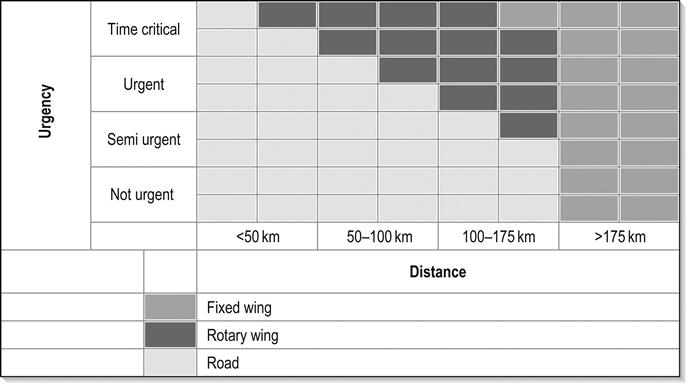
Transport platforms
Crew
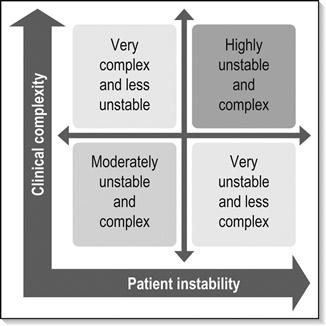
Skill sets
< div class='tao-gold-member'>

Full access? Get Clinical Tree


26. Emergency and Medical Systems
Only gold members can continue reading. Log In or Register to continue